Frequency of EGFR Mutations in Patients with Lung Adenocarcinoma: Comparative Study between Private and Public Healthcare Centers
Article Information
Rodríguez-Cid Jeronimo Rafael1*, Martos-Ramírez Guillermo2, García-Montes Vanessa3, Flores-Mariñelarena Rodrigo Rafael4, Bonilla-Molina Diana1, Olivares-Beltran Guillermo2, Imaz-Olguin Victoria2, Green-Renner Dan2, Zarate-Osorno Alejandra3, Garcia Socrates3, Martínez-Barrera Luis1, Alatorre-Alexander Jorge Arturo1, Santillan-Doherty Patricio Javier5
1Department of Oncology, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico city, Mexico
2Department of Oncology, America British Cowdray Medical Center, Mexico city, Mexico
3Department of Oncology, Hospital Español, Mexico city, Mexico
4School of Medicine, Monterrey Institute of Technology and Higher Education, Mexico city, Mexico
5Medical direction, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico city, Mexico
*Corresponding Author: Jeronimo Rafael Rodríguez-Cid, Instituto Nacional de Enfermedades Respiratorias. Calzada de Tlalpan 4502, Colonia Belisario Dominguez Sección XVI, Delegación Tlalpan, C.P. 14080, Clínica de Oncología Torácica, Pabellón 6.
Received: 04 December 2019; Accepted: 12 December 2019; Published: 20 January 2020
Citation: Rodríguez-Cid Jeronimo Rafael, Martos-Ramírez Guillermo, García-Montes Vanessa, Flores-Mariñelarena Rodrigo Rafael, Bonilla-Molina Diana, Olivares-Beltrán Guillermo, Imaz-Olguín Victoria, Green-Renner Dan, Zárate-Osorno Alejandra, García Sócrates, Martínez-Barrera Luis, Alatorre-Alexander Jorge Arturo, Santillan-Doherty Patricio Javier. Frequency of EGFR Mutations in Patients with Lung Adenocarcinoma: Comparative Study between Private and Public Healthcare Centers. Archives of Clinical and Medical Case Reports 4 (2020): 97-105.
View / Download Pdf Share at FacebookAbstract
Purpose: The present study aims to describe the differences in the prevalence of EGFR mutation of lung adenocarcinoma between private and public healthcare institutions.
Methods: This was a descriptive, observational, retrospective, multicenter study with confirmed diagnosis of non-small cell lung cancer, adenocarcinoma subtype, distributed between two private practice centers and one public healthcare institution. After a pathology review to determine whether there was enough tumor tissue to make a molecular biology study, mutations were determined using real-time PCR for EGFR tyrosine-kinase domain gene.
Results: After exclusions a total of 328 patients results for the final analysis. Two hundred thirty-five patients (71.64%) attended a public healthcare institution and ninety-three patients (28.35%) to a private healthcare institution (Table 1). From the public healthcare institution, 113 (34.45%) patients had a positive EGFR mutation, while only 27 patients (8.23%) from the private healthcare institution were positive for an EGFR mutation. When comparing the total number of patients in the study, this difference was statistically significant when comparing public versus private hospitals (p=0.002).
Conclusion: We found that there is a statistically significant difference between the frequency of EGFR mutations between populations attending public and private healthcare institutions, probably related to ethnic differences between populations. Despite what has been reported in the present study, these conclusions cannot be generalized and further investigation is needed.
Keywords
Lung adenocarcinoma; EGFR; Private healthcare institution; Public healthcare institution
Lung adenocarcinoma articles, EGFR articles, Private healthcare institution articles, Public healthcare institution articles
Article Details
1. Introduction
Lung cancer is one of the most prevalent malignancy in the world and the leading death cause due to cancer [1, 2]. The estimated number of new cases detected every year is 1.8 million, accounting for 12.9% of all malignancies diagnosed in 2012, with an annual mortality rate of 19.4%, which translates to 1.59 million deaths according to worldwide statistics. The most prevalent rates (up to 58%) have been found in Europe, East Asia, and Sub-Saharan Africa [3]. In Mexico, the incidence of lung cancer ranges between 4.3-6.8/100,000 habitats in the latest epidemiological report, accounting for 11% of cancer-specific deaths [4, 5]. Notwithstanding that smoking is one of the most recognized risk factors for lung cancer (85% in men and 47% in women), different risk factors have been described, including exposure to wood smoke, work-related exposure (silica, carbon, radon, and petrochemical substances), among others [6, 7].
The most common subtype of lung cancer is adenocarcinoma (40% in men and up to 50% in women), being especially prevalent in non-smokers with a high frequency of mutations in specific genes, such as EGFR, KRAS, ALK, and ROS1. These mutations can be present in up to 64% of patients with adenocarcinoma, having special importance for the use of targeted therapy [7, 8]. EGFR classically described as the most prevalent gene mutated in lung adenocarcinoma have different mutations of clinical relevance, for example, exon 19 deletions and L858R substitutions in exon 21 accounting 90-95% of the cases. Their frequency varies depending on several factors like smoking history (more prevalent in non-smokers), sex (more common in female patients) and race (10-15% in Caucasians and up to 50% in the Asian population) [9]. The differences mentioned above have been of utility for the introduction in the therapeutic approach of multiple agents approved in first-line, including Erlotinib, Gefitinib, and Afatinib [10-15]. More recently, due to T790M tyrosine kinase inhibitors resistance mutation, a third-generation of inhibitors have been approved, with promising results [16-21]. In Mexico, there are multiple disparities and limitations towards access to an adequate health system generating a great heterogeneity of population among those who attend a public and private institute. This exemplifies a common problem raised in developing countries where we need more investigation to improve the oncological approach.
The present study aims to describe the differences in the prevalence of EGFR mutation of lung adenocarcinoma between private and public healthcare institutions.
2. Material and Methods
This was a descriptive, observational, retrospective, multicenter study with a consecutive selection of 333 patients with confirmed diagnosis of non-small cell lung cancer, adenocarcinoma subtype, distributed between two private practice centers (ABC Medical Center and the Spanish Society, Spanish Hospital of Mexico) and one public healthcare institution (Instituto Nacional de Enfermedades Respiratorias, Ismael Cosío Villegas [INER]). The study design was approved by INER’s Institutional Ethics Board following the Declaration of Helsinki, Fortaleza Brazil 2013. The study included patients aged 18 years or older, with a pathology report and determination of complete mutations, who had been diagnosed between January 2011 and January 2016. Early stages were analyzed for research purposes only. After a pathology review to determine whether there was enough tumor tissue to make a molecular biology study, mutations were determined using real-time PCR for EGFR tyrosine-kinase domain gene involving exons 18, 19, 20, and 21 (exon 19 deletion and exons 18, 20, and 21 insertions [G719X, T790M, and L858R-L861Q]). Neoplastic cells were selected and their genomic DNA was extracted; fluorescein and non-fluorescein primers to detect mutated and wild- type forms of the EGFR gene were used. Sample delta Ct values for mutation and control reactions were calculated and compared versus delta Ct values in each mutated reaction, to determine the presence of each type of mutation. Positive and negative controls were used with each sample. The statistical analysis was done using SPSS software version 24.0 (IBM software, Armonk, NY, USA). Pearson’s correlation was used to assess significance between quantitative variables with a criterion for statistical significance of p <0.05. One-factor Anova was used to determine between-group variability. All financial related issues were absorbed by the investigation group from the study.
3. Results
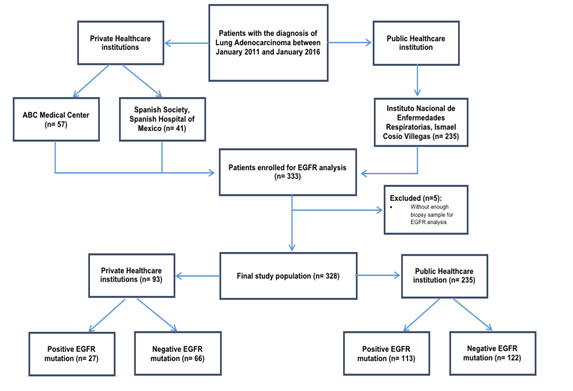
A total of 333 patients were included, distributed among the 3 healthcare centers: 57 patients in the ABC Medical Center, 41 patients in the Spanish Society, Spanish Hospital of Mexico and 235 at the INER. Five patients were excluded due to a lack of enough biopsy sample for EGFR analysis resulting in a total of 328 patients for the final analysis (Figure 1). From the total study population, 193 patients were female (58.84%) and 135 Male (41.16%), with a mean age of 62.4 years (±13). The vast majority confirmed a smoking status (69.4%), however, only 1.38% referred exposure to wood smoke. The clinical-stage distribution was 5.2% stage I, 4.3% stage II, 7.9% stage III, and 75.3% were stage IV, however, the 7.3% of the patients were non-evaluable. Regard the functional status (according to the Eastern Cooperative Oncology Group) 12.2% were grade 0, 5.2% were grade 1, 7.01% were grade 2 and 75.6% were grade 3. We found a general EGFR mutation frequency of 42.7% with Del19 and L858R substitutions [21] being the two most common types, with 66.4% and 30%, respectively, while exon 20 and 18 alterations accounted for 3.5% (2.1% and 1.4%, respectively).
Two hundred thirty-five patients (71.64%) attended a public healthcare institution and ninety-three patients (28.35%) to a private healthcare institution (Table 1). From the public healthcare institution, 113 (34.45%) patients had a positive EGFR mutation, while only 27 patients (8.23%) from the private healthcare institution were positive for an EGFR mutation. When comparing the total number of patients in the study, this difference was statistically significant when comparing public versus private hospitals (p=0.002). Another finding with a tendency to significance was gender (p=0.084), being more common among women.
|
Variable |
Private healthcare institution (n= 93) |
Public healthcare institution (n= 235) |
|
Age, mean (±SD^) |
67.1 years (±12.6) |
60.5 years (±12.7) |
|
Gender |
46 (49.5) |
146 (62.13) |
|
· Female, n (%) |
||
|
· Male, n (%) |
47 (50.5) |
89 (37.9) |
|
Clinical Stage |
||
|
· Stage I, n (%) |
16 (17.2) |
1 (0.4) |
|
· Stage II, n (%) |
9 (9.7) |
5 (2.1) |
|
· Stage III, n (%) |
11 (11.8) |
15 (6.4) |
|
· Stage IV, n (%) |
57 (61.3) |
190 (80.9) |
|
· Non-evaluable, n (%) |
0 (0) |
24 (10.2) |
|
ECOG+ |
||
|
· 0, n (%) |
38 (40.9) |
1 (0.4) |
|
· 1, n (%) |
12 (12.9) |
5 (2.1) |
|
· 2, n (%) |
8 (8.6) |
15 (6.4) |
|
· 3, n (%) |
35 (37.6) |
214 (91.1) |
|
· 4, n (%) |
0 (0) |
0 (0) |
|
· 5, n (%) |
0 (0) |
0 (0) |
|
Positive EGFR mutation, n (%) |
27 (29) |
113 (48.1) |
|
EGFR mutation subtype |
||
|
· Exon 18, n (%) |
2 (7.4) |
0 (0) |
|
· Exon 19, n (%) |
11 (40.7) |
82 (72.6) |
|
· Exon 20, n (%) |
2 (7.4) |
1 (0.9) |
|
· Exon 21, n (%) |
12 (44.4) |
30 (26.5) |
^SD= Standard Deviation, *INER= Instituto Nacional de Enfermedades Respiratorias, Ismael Cosío, +ECOG = Eastern Cooperative Ongology Group
Table 1: General characteristics of the study population (n=328).
4. Discussion
Results from many studies have suggested that there are biological, clinical, and pathological differences across populations diagnosed with lung cancer, and these differences are known to influence not only the prognosis but also the efficacy of cancer treatments. The frequency of EGFR mutations has been reported in Asia at 60-50%, 10-14% in the United States, and 11% in the European population [22], however, Latin America had shown a great heterogeneity by country and this can be explained by ancestral background and ethnicity of each population. Peru is the country with the highest incidence of mutations, with 51.1% (very similar to the Asian population), while Argentina has 14.4% (more comparable with European populations) [23], in contrast, countries like Panama or Colombia show 27.3% and 24.7%, respectively. The Mexican population has also shown differences versus other Hispanic populations around the world, such as the Hispanic population in the United States [24, 25]. However, the results of this study also show that there can be major biological differences within a particular population. This can involve several different factors, including the high level of miscegenation in the Mexican population. The frequency of EGFR mutations from the total study population reported by this study (42.7%) shows similarity to the reports in the Asian population, and to prior reports from other hospitals in our country [22], however, frequency in private institutions shows a prevalence of EGFR mutations of 29%, which does not match what has been reported in our population but rather aligns with the frequency of presentation in some Anglo-Saxon countries and the rest of Western Europe. With these specific results, we could infer that there are population differences between institutions, due to differences in access to private healthcare in the overall population. While most of the population has access to a social security program, a small group also enjoys coverage in private institutions; this small part of the population usually involves first- or second-generation European immigrants (primarily from countries with linguistic similarities), although they are Mexican by birth, a small proportion reside in Mexico City for a number of reasons, such as work or personal reasons. These patients are very different from the large majority of our country’s population, and this could explain why their mutation expression resembles that of their country of origin. The higher presentation of EGFR mutations the public healthcare institution must consider that this healthcare center acts as a reference center for lung cancer, increasing the probability of patients with an EGFR mutation.
Our findings regarding age at presentation and clinical stage are consistent with what has been reported worldwide; however, a larger percentage of women was observed (58.8% vs. 41.2%), which is probably explained, because of lower exposure to smoking in Mexico and higher exposure to wood smoke, a factor higher association of EGFR mutations in prior studies [25].
The lower exposure to smoke in Mexico is also an important factor to consider, as there is compelling data showing that mutations presenting in smokers are different somatic mutations in the non-smoking population, with TP53 (38%), EGFR (20%), KRAS (13%), NFE2L2 (6%), and PIK3CA (4%) mutations were more common among smokers, and EGFR (61%), TP53 (15%), KRAS (4%), and PI3KCA (2%) mutations being more common among non-smokers [6]. The incidence of TP53 and KRAS mutations increases with smoking, while EGFR mutations decrease [26-28]. Clinical stage IV was the most prevalent, as would be expected due to usually late diagnosis. However, we found that most patients with clinical stage I-II were diagnosed in private hospitals, which can be due to better access to programmed follow-up tests or routine laboratory exams that help to detect anomalies earlier, leading to an earlier intervention.
5. Conclusion
While findings in terms of age, gender, and clinical presentation were similar to prior reports, we found that there is a statistically significant difference between the frequency of EGFR mutations between populations attending public and private healthcare institutions, probably related to ethnic differences between populations. The predominant population in private hospitals involves immigrants from Europe and the United States and their descendants in the analyzed population. Within what appears to be a single population, they are different factors (ethnicity, ancestral background, exposure to smoking, firewood smoke, prior infectious processes) that create differences within it. This explains why individual clinical characteristics are to be considered at all times, as they influence both the prognosis and the efficacy of treatments and warrants the need for personalized medicine. Despite what has been reported in the present study, these conclusions cannot be generalized and further investigation is needed.
Conflicts of Interest
Dr. Jeronimo Rafael Rodriguez-Cid has educational, investigational and advice relations with MSD, Bristol Myers, Roche, Takeda, Amgen, Abvie, Aztra Zeneca, Boehringer Ingelheim, Pfizer, Celgen, Novartis and Bayer; Dr. Jorge Arturo Alatorre-Alexander has educational, investigational and advice relations with MSD, Bristol Myers, Roche, Takeda, Aztra Zeneca, Boehringer Ingelheim and Pfizer. The other authors have no conflicts of interest to declare.
References
- Kauffmann-Guerrero D, Huber RM, Reu S, et al. NSCLC Patients Harbouring Rare or Complex EGFR Mutations Are More Often Smokers and Might Not Benefit from First-Line Tyrosine Kinase Inhibitor Therapy. Respiration 95 (2018): 169-176.
- Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304 (2004): 1497-500.
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer (2014).
- inegi.org.mx/est/contenidos/proyectos/registros/vitales/mortalidad/tabulados/ConsultaMortalidad.asp
- SINAIS/SINAVE/DGE/SALUD/Perfil epidemiológico de los tumores malignos en México.Junio.2011
- Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365 (2011): 395-409.
- Hagop Kantarjian M, Robert Wolff A, McGraw Hill. The MD Anderson Manual of Medical Oncology 3e (2016).
- DeVita Vincent T, Lawrence Theodore S, Rosenberg Steven A. Principles and Practice of Oncology, 8th Edition, Lippincott Williams and Wilkins (2008).
- NCCN Clinical Guidelines in Oncology: Non-Small Cell Lung Cancer, Version 4 (2016).
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361 (2009): 947-957.
- Maemondo M, Inoue A, Kobayashi K, et al. North-East Japan Study Group. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362 (2010): 2380-2388.
- Mitsudomi T, Morita S, Yatabe Y, et al. West Japan Oncology Group. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 11 (2010): 121-128.
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 12 (2011): 735-742.
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13 (2012): 239-246.
- Gridelli C, Ciardiello F, Gallo C, et al. First-line erlotinib followed by second-line cisplatin-gemcitabine chemotherapy in advanced non-small-cell lung cancer: the TORCH randomized trial. J Clin Oncol 30 (2012): 3002-3011.
- Gil-Bazo I, Rolfo C. AZD9291 in TKI EGFR resistance in non-small cell lung cancer and the new concept of phase I trials. Transl Lung Cancer Res 5 (2016): 85-88.
- https://clinicaltrials.gov/ct2/show/NCT02296125 - AZD9291 Versus Gefitinib or Erlotinib in Patients With Locally Advanced or Metastatic Non-small Cell Lung Cancer (FLAURA)
- Cortinovis D, Abbate M, Bidoli P, Capici S, Canova S. Targeted therapies and immunotherapy in non-small-cell lung cancer. Ecancermedicalscience 23 (2016): 648.
- Sequist LV, Soria JC, Goldman JW, et al. Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med 372 (2015): 1700-1709.
- https://clinicaltrials.gov/ct2/show/NCT02186301 - TIGER-3: Open Label, Multicenter Study of Rociletinib Mono Therapy Versus Single-agent Cytotoxic Chemotherapy in Patients With Mutant EGFR NSCLC Who Have Failed at Least One Previous EGFR-Directed TKI and Platinum-doublet Chemotherapy (CO-1686).
- https://clinicaltrials.gov/ct2/show/NCT02186301 - TIGER-1: Safety and Efficacy Study of Rociletinib or Erlotinib in Patients With EGFR-mutant/Metastatic NSCLC Who Have Not Had Any Previous EGFR Directed Therapy (CO-1686).
- Patel MI, Schupp CW, Gomez SL, et al. How do social factors explain outcomes in non-small-cell lung cancer among Hispanic in California Explaining the Hispanic Paradox J. Clin. Oncol 31 (2013): 1-8.
- Arrieta O, Ramírez LA, Baéz R, et al. Different mutation profiles and clinical characteristics among Hispanic patients with non-small cell lung cancer could explain the “Hispanic paradox”. Lung Cancer 90 (2015): 161-166.
- Arrieta O, Cardona AF, Bramuglia F, et al. Genotyping non-small cell lung cancer (NSCLC) in Latin America, J. Thorac. Oncol 6 (2011): 1955-1959.
- Saeed AM, Toonkel R, Glassberg MK, et al. The influence of Hispanic ethnicity on no small cell lung cancer history and patient survival: an analysis of the survival, epidemiology, and end results database, Cancer 118 (2012): 4495-4501.
- Guerrero-López CM, Muños Hernández JA, de Miera JuárezBS, et al. Evidencia para la política pública en salud: Consumo de tabaco en México 2000–2012:los beneficios de su reducción. ENSANUT (2012).
- Kawachi T, Koh Y, Ando M, et al. Prospective Analysis of Oncogenic Driver Mutations and Environmental Factors: Japan Molecular Epidemiology for Lung Cancer Study. Journal of Clinical Oncology 34 (2016): 2247-2257.
- Cancer Genome Atlas Research N. Comprehensive molecular profiling of lung adenocarcinoma. Nature 511 (2014): 543-550.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
