Giant Left Pheochromocytoma and its Innovative Therapeutic Paradigm
Article Information
Madathipat Unnikrishnan1*, Ramankutty Ramraj2, Dathan Neetu S3
1Department of Vascular surgery, SUT Hospital, Pattom, Trivandrum, Kerela, India
2Department of General surgery, SUT Hospital, Pattom, Trivandrum, Kerela, India
3Department of Pathology, SUT Hospital, Pattom, Trivandrum, Kerela, India
*Corresponding Author: Madathipat Unnikrishnan, Department of Vascular surgery, SUT Hospital, Pattom, Trivandrum, Kerela, India
Received: 26 August 2019; Accepted: 09 September 2019; Published: 16 September 2019
Citation: Unnikrishnan M, Ramraj R, Neetu SD. Giant Left Pheochromocytoma and its Innovative Therapeutic Paradigm. Journal of Surgery and Research 2 (2019): 188-192.
View / Download Pdf Share at FacebookAbstract
Pheochromocytoma, rare tumour arising from chromaffin cells of suprarenal medulla presents with paroxysmal hypertension due to biochemical endocrine activity. Nevertheless, giant tumour is known to show endocrine inactivity. We describe 56-yr-old lady on antihypertensives who incidentally showed large suprarenal mass in abdominal ultrasonogram with no overt endocrine activity biochemically. Computed tomography scan showed well circumscribed left sided giant suprarenal tumour pushing left diaphragmatic dome upwards and left kidney downwards. Thoraco-phreno-laparotomy was employed instead of standard laparotomy for its safe and tidy removal. Tumour weighed 490 grams and histopathology confirmed benign pheochromocytoma. During follow-up at one year she remains asymptomatic.
Keywords
Giant pheochromocytoma, Therapeutic paradigm
Giant pheochromocytoma articles, Therapeutic paradigm articles
Giant pheochromocytoma articles Giant pheochromocytoma Research articles Giant pheochromocytoma review articles Giant pheochromocytoma PubMed articles Giant pheochromocytoma PubMed Central articles Giant pheochromocytoma 2023 articles Giant pheochromocytoma 2024 articles Giant pheochromocytoma Scopus articles Giant pheochromocytoma impact factor journals Giant pheochromocytoma Scopus journals Giant pheochromocytoma PubMed journals Giant pheochromocytoma medical journals Giant pheochromocytoma free journals Giant pheochromocytoma best journals Giant pheochromocytoma top journals Giant pheochromocytoma free medical journals Giant pheochromocytoma famous journals Giant pheochromocytoma Google Scholar indexed journals Therapeutic paradigm articles Therapeutic paradigm Research articles Therapeutic paradigm review articles Therapeutic paradigm PubMed articles Therapeutic paradigm PubMed Central articles Therapeutic paradigm 2023 articles Therapeutic paradigm 2024 articles Therapeutic paradigm Scopus articles Therapeutic paradigm impact factor journals Therapeutic paradigm Scopus journals Therapeutic paradigm PubMed journals Therapeutic paradigm medical journals Therapeutic paradigm free journals Therapeutic paradigm best journals Therapeutic paradigm top journals Therapeutic paradigm free medical journals Therapeutic paradigm famous journals Therapeutic paradigm Google Scholar indexed journals chromaffin cells articles chromaffin cells Research articles chromaffin cells review articles chromaffin cells PubMed articles chromaffin cells PubMed Central articles chromaffin cells 2023 articles chromaffin cells 2024 articles chromaffin cells Scopus articles chromaffin cells impact factor journals chromaffin cells Scopus journals chromaffin cells PubMed journals chromaffin cells medical journals chromaffin cells free journals chromaffin cells best journals chromaffin cells top journals chromaffin cells free medical journals chromaffin cells famous journals chromaffin cells Google Scholar indexed journals suprarenal medulla articles suprarenal medulla Research articles suprarenal medulla review articles suprarenal medulla PubMed articles suprarenal medulla PubMed Central articles suprarenal medulla 2023 articles suprarenal medulla 2024 articles suprarenal medulla Scopus articles suprarenal medulla impact factor journals suprarenal medulla Scopus journals suprarenal medulla PubMed journals suprarenal medulla medical journals suprarenal medulla free journals suprarenal medulla best journals suprarenal medulla top journals suprarenal medulla free medical journals suprarenal medulla famous journals suprarenal medulla Google Scholar indexed journals paroxysmal hypertension articles paroxysmal hypertension Research articles paroxysmal hypertension review articles paroxysmal hypertension PubMed articles paroxysmal hypertension PubMed Central articles paroxysmal hypertension 2023 articles paroxysmal hypertension 2024 articles paroxysmal hypertension Scopus articles paroxysmal hypertension impact factor journals paroxysmal hypertension Scopus journals paroxysmal hypertension PubMed journals paroxysmal hypertension medical journals paroxysmal hypertension free journals paroxysmal hypertension best journals paroxysmal hypertension top journals paroxysmal hypertension free medical journals paroxysmal hypertension famous journals paroxysmal hypertension Google Scholar indexed journals giant tumour articles giant tumour Research articles giant tumour review articles giant tumour PubMed articles giant tumour PubMed Central articles giant tumour 2023 articles giant tumour 2024 articles giant tumour Scopus articles giant tumour impact factor journals giant tumour Scopus journals giant tumour PubMed journals giant tumour medical journals giant tumour free journals giant tumour best journals giant tumour top journals giant tumour free medical journals giant tumour famous journals giant tumour Google Scholar indexed journals abdominal ultrasonogram articles abdominal ultrasonogram Research articles abdominal ultrasonogram review articles abdominal ultrasonogram PubMed articles abdominal ultrasonogram PubMed Central articles abdominal ultrasonogram 2023 articles abdominal ultrasonogram 2024 articles abdominal ultrasonogram Scopus articles abdominal ultrasonogram impact factor journals abdominal ultrasonogram Scopus journals abdominal ultrasonogram PubMed journals abdominal ultrasonogram medical journals abdominal ultrasonogram free journals abdominal ultrasonogram best journals abdominal ultrasonogram top journals abdominal ultrasonogram free medical journals abdominal ultrasonogram famous journals abdominal ultrasonogram Google Scholar indexed journals adrenal medulla articles adrenal medulla Research articles adrenal medulla review articles adrenal medulla PubMed articles adrenal medulla PubMed Central articles adrenal medulla 2023 articles adrenal medulla 2024 articles adrenal medulla Scopus articles adrenal medulla impact factor journals adrenal medulla Scopus journals adrenal medulla PubMed journals adrenal medulla medical journals adrenal medulla free journals adrenal medulla best journals adrenal medulla top journals adrenal medulla free medical journals adrenal medulla famous journals adrenal medulla Google Scholar indexed journals large benign articles large benign Research articles large benign review articles large benign PubMed articles large benign PubMed Central articles large benign 2023 articles large benign 2024 articles large benign Scopus articles large benign impact factor journals large benign Scopus journals large benign PubMed journals large benign medical journals large benign free journals large benign best journals large benign top journals large benign free medical journals large benign famous journals large benign Google Scholar indexed journals necrotic area articles necrotic area Research articles necrotic area review articles necrotic area PubMed articles necrotic area PubMed Central articles necrotic area 2023 articles necrotic area 2024 articles necrotic area Scopus articles necrotic area impact factor journals necrotic area Scopus journals necrotic area PubMed journals necrotic area medical journals necrotic area free journals necrotic area best journals necrotic area top journals necrotic area free medical journals necrotic area famous journals necrotic area Google Scholar indexed journals
Article Details
1. Introduction
Pheochromocytoma originating from chromaffin cells of adrenal medulla may present unilateral or bilateral and as paragangliomas from extraadrenal sympathetic ganglia in chest, abdomen or neck in our body. Usually small in size, pheochromocytoma is hormonally active presenting with episodic severe hypertension along with flushing, headache, sweating and palpitation [1]. Nevertheless those larger than ten cms in size, called giant tumours, are by and large benign and biochemically hormonally inactive [2]. Herein we report innovative surgical approach for excision of giant pheochromocytoma.
2. Case Report
A 56-year-old housewife reported dull ache in left upper back since two years. Pain was nondisabling and she denied bowel or urinary symptoms. She was hypertensive since five years controlled with two drugs [Clinidipine 5 mg and Losartan 25 mg, each twice daily]. Examination showed middle aged lady comfortable at rest. Her blood pressure (BP) measured 130/80 mmHg in right upper limb and all her peripheral pulses were well felt. All other system examination appeared normal with no features of hereditary syndromes. Ultrasonogram (USG) showed large well-defined heterogenous retroperitoneal mass in left suprarenal region with mildly enhancing periphery, nonenhancing necrotic area centrally, preserved fat planes around, pushing kidney downwards and dome of diaphragm upwards. Computed tomography (CT) scan confirmed USG features of well-circumscribed heterogenous mass in left suprarenal area measuring 12.5 × 9 × 8.5 cms in size, displacing body and tail of pancreas anteriorly, kidney downwards and dome of diaphragm upwards. Arterial branches arose directly from aorta and upper polar branch of left renal artery [Figure 1].
Investigations showed normal haematological and biochemical parameters. Specific biochemical estimation of plasma free metanephrines and urinary vanillyl mandelic acid (VMA) was within normal limits. Her blood group was A-negative. In view of CT Scan features of giant tumour, adrenal carcinoma and pheochromocytoma were considered and open surgery was planned.
2.1 Surgery
Under general anaesthesia and tracheal intubation, radial arterial line, jugular triple lumen central line, epidural catheter and bladder catheterisation, patient was positioned with left hemithorax 50 degree raised and abdomen close to supine. As a matter of precaution, noradrenaline, nitroglycerine infusions and injectable esmalol were prepared and kept ready for instant use. Autologous blood was collected in view of her A-negative blood group. Thoraco-phreno-laparotomy was performed through seventh left intercostal space, costal margin was transected, retroperitoneal region was accessed after dividing oblique muscles and left dome of diaphragm was partially divided. Intact peritoneum with all contents was reflected to the right and tumour was easily identified in Gerota’s fascia wherein kidney was pushed downwards [Figure 2A].
The vascular tumour appeared separate from all structures by layer of thick fat with no features of infiltration. Mutiple arterial branches and venous channels were carefully divided between suture ties. Vascular tumour was removed in-toto uneventfully. Satisfactory haemostasis was obtained. Thoraco-laparotomy was repaired in standard fashion along with drainage tubes in situ and patient returned to intensive care unit in stable condition. Patient’s BP remained above 200 mmHg while tumour was being dissected and manipulated despite all available vasodilators and injectable beta blockers. Once removed BP transiently dropped to 50 mmHg requiring noradrenaline, fluids and autologous blood for haemodynamic stability [3]. Her post-operative recovery was smooth. She was dismissed from hospital on seventh post-op day on deescalated antihypertensives. Six months later she is asymptomatic, BP controlled with half tablet Repace, and is on close follow-up.
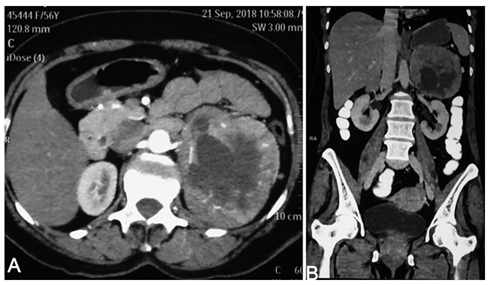
Figure 1: (A) Contrast enhanced CT scan axial and (B) coronal views showing large suprarenal well circumscribed mildly enhancing mass in retroperitoneum abutting abdominal aorta, pushing left kidney downwards and dome of diaphragm upwards with central large hypodense necrotic area.
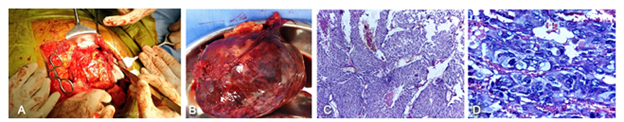
Figure 2: (A) Intraoperative photograph showing thoraco-phreno-laparotomy, dissection and release of tumour in progress. This approach provided direct access and safe approach to Gerota’s fascia,whole mass and control of vascular pedicles for disconnection; (B) Resected specimen of encapsulated tumor weighing 490 grams which was solid and cystic, soft to firm and brown red in appearance; (C) Photomicrograph showing cellular neoplasm in large nests [zellballen] with central comedo type necrosis (H&E, ×100); (D) Photomicrograph showing tumor cells with nuclear hyperchromasia, pleomorphism and mitotic activity (0-3 per10hpf) (H&E, ×400). The atypical features added up to a pheochromocytoma of adrenal scaled score (PASS) of 10/20, benign with malignant potential.
2.2 Pathology
On gross examination, the tumour weighing 490 gm and measuring 12.5 × 9 × 8.5 cm was encapsulated with variegated cut surface predominantly solid, firm, brownish with cystic degeneration centrally [Figure 2B]. Microscopy showed cellular neoplasm in nests with tumoural capsular invasion. Inked resection margins, vessels and periadrenal tissue were tumour free.Immunohistochemistry confirmed pheochromocytoma [synaptophysin/chromogranin-strong positive, inhibin-negative] with low proliferation [Ki67<1%] and PASS score 10/20 [Figure 2C and D] [4].
3. Discussion
Pheochromocytoma has its origin from chromaffin cells in adrenal medulla and rarely from medulla of sympathetic ganglia in chest, neck or abdomen when the latter is called paraganglioma[s]. Tumour, usually small in size, at times bilateral and hormonally active with its production of catecholamines, presents with classic features of paroxysmal hypertension, sweating, flushing and palpitation. Nevertheless, a small subset attains size over ten cms called giant tumour characterised by hormonal inactivity and benign clinical presentation like index case. USG helps in finding suprarenal mass, but CTScan or MRI is needed for delineation of details. Hormonal activity is identified by measuring plasma metanephrine level and urinary VMA. These tests have 98% sensitivity and over 90% specificity respectively and our patient's tumour was biochemically inactive [1]. For pheochromocytoma small in size [<6 cms], laparoscopic resection is standard therapeutic option. However in view of its size [12.5 × 9 × 8.5 cms] and possibilty of malignancy, open surgical removal was considered for complete resection, avoid local reccurence and tumour seedling. Standard laparotomy with midline transperitoneal entry and left paracolic access to retroperitoneal space is generally practiced [2]. Tumour of size [eventually weighed 490 gms], placed very deep and high under the left dome of diaphragm abutting suprarenal aorta along with large multiple arterial feeders and draining venous channels pose difficult technical challenge.
Although most large tumors are hormonally inactive, surgical manipulation may lead to surge of catecholamines into circulation leading to severe hypertension and precipitous pressure drop after resection like index case reported [1, 2]. We chose to perform tumour resection through thoraco-phreno-laparotomy to obtain direct access using pleural entry in seventh left intercostal space, transecting costal margin and dividing oblique abdominal muscles without transgressing the peritoneal cavity. Our approach led to direct and safer access for dissection, control of blood vessels and protection of neighbouring vital organs requiring only autologous blood transfusion in operating room. In addition, oral fluids could be commenced next day avoiding paralytic ileus and potential for laparotomy related adverse events. However this approach could be used only for left sided tumour since liver would not permit thoracolaparotomy likewise for right sided suprarenal mass.
4. Conclusion
Authors report left sided giant pheochromocytoma surgically excised using thoraco-phreno-laparotomy [akin to Stoney's procedure for exposure of thoracoabdominal aorta] that provided direct, safer and less morbid approach leading to tidy resection. This report potentially pertains to 39th case of giant pheochromocytoma in English literature and first ever experience using thoraco-phreno-laparotomy for successful and hassle free excision.
Acknowledgements
Authors wish to place on record their appreciation to our colleagues Prof Sivaramakrishnan, Head of Department of Urology and Transplantation, for technical help and urological expertise and Dr Sharad, Associate Consultant Department of General surgery for clinical work up,intra operative and post op care of patient.
Ethical Approval
Authors certify that Instituitional ethics committee approval was obtained. Written informed consent from patient was obtained. Financial support was not used.
Conflict of Interest
No conflicts of interest exist.
References
- Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and Paraganglioma; An Endocrine Society Clinical Practice Guidelines. J Clin Endocrinol Metab 99 (2014): 1915-1942.
- Maharaj R, Parbhu S, Ramcharan W, et al. Giant cystic pheochromocytoma with low risk of malignancy: a case report and literature review. Case Rep Oncol Med (2017): 1-7.
- Prakash P, Ramachandran R, Tandon N, et al. Changes in Blood pressure, Blood sugar and Quality of life in patients undergoing Pheochromocytoma surgery - Prospective Cohort Study. Indian J Urol 35 (2019): 34-40.
- Lester DR Thompson. Pheochromocytoma of the Adrenal Gland Scaled Score (PASS) to Separate Benign From Malignant Neoplasms. A Clinicopathologic and Immunophenotypic Study of 100 Cases. Am J Surg Pathol 26 (2002): 551-566.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 