Oxygen Saturation in Neonates After Birth in Rural Hospital
Article Information
Amar Taksande*, Rewat Meshram, Amol Lohakare, Sadhana Purandare, Ankush Kommawar
Department of Pediatrics, Jawaharlal Nehru Medical College, Sawangi Meghe, Wardha, Maharashtra, 442102, India.
*Corresponding Author: Amar Taksande, Department of Pediatrics, Jawaharlal Nehru Medical College, Sawangi Meghe, Wardha, Maharashtra, 442102, India
Received: 20 November 2016; Accepted: 19 January 2017; Published: 27 January 2017
View / Download Pdf Share at FacebookAbstract
Background: Pulse oximetry is a noninvasive test for quantification of hypoxemia. It is a simple bedside test to determine the amount of oxygen in a baby's blood and use for early detection of critical congenital heart disease (CCHD).
Aim: To analyze the influence of birth weight, gestational age, mode of delivery and gender, on levels of SpO2 in healthy newborns.
Methods: Within first 6 hours of life, pulse oximetry was performed on clinically normal newborns. Echocardiography was performed, if oxygen saturation (SpO2) was below 90%. Inclusion criteria: Newborns who were admitted in postnatal ward & NICU. Exclusion criteria: Out born babies and babies with a prenatal diagnosis of duct dependent circulation. SpO2 were performed using a Massimo Single Extraction Technology (SET) handheld pulse oximeter with a neonatal reusable Nellcor SpO2 sensor OXI-A/N probe. For each newborn, SpO2 was measured by trained social worker of the newborn within the first 6 hours of life. The probe was held manually to the sole of the foot.
Results: A total of 6101 neonates were born at the hospital during the period of January 2013 to December 2014 and registered in the CCHD screening project. For 68 neonates (1.1%), the first SpO2 was <95% and they were not included in the further analyses. 1958 neonates with weight less than 2.5 kg were excluded from the study. A total of 4075 neonates (1961 boys and 2114 girls) fulfilled the criteria for inclusion in the final analyses. The mean birth weight of the neonates was 2.81±0.27 Kg and the mean GA was 38.64±1.29 weeks. SpO2 was not related to GA when analyzed by one-way ANOVA (F: 0.88; P>0.01). No statistical significant difference in SpO2 was found in children born by caesarean section (98.62±1.20) than in those delivered vaginally (98.62±1.17).
Keywords
Pulse Oximetry; Oxygen Saturation; Newborn; Screening; Birth Weight
Oxygen Saturation articles Oxygen Saturation Research articles Oxygen Saturation review articles Oxygen Saturation PubMed articles Oxygen Saturation PubMed Central articles Oxygen Saturation 2023 articles Oxygen Saturation 2024 articles Oxygen Saturation Scopus articles Oxygen Saturation impact factor journals Oxygen Saturation Scopus journals Oxygen Saturation PubMed journals Oxygen Saturation medical journals Oxygen Saturation free journals Oxygen Saturation best journals Oxygen Saturation top journals Oxygen Saturation free medical journals Oxygen Saturation famous journals Oxygen Saturation Google Scholar indexed journals congenital heart disease articles congenital heart disease Research articles congenital heart disease review articles congenital heart disease PubMed articles congenital heart disease PubMed Central articles congenital heart disease 2023 articles congenital heart disease 2024 articles congenital heart disease Scopus articles congenital heart disease impact factor journals congenital heart disease Scopus journals congenital heart disease PubMed journals congenital heart disease medical journals congenital heart disease free journals congenital heart disease best journals congenital heart disease top journals congenital heart disease free medical journals congenital heart disease famous journals congenital heart disease Google Scholar indexed journals
Article Details
1. Introduction
Pulse oximetry is a screening method for early detection of CCHD was base on clinically unde-tectable hypoxemia in life threatening heart cases. Recent studies have suggested that SpO2 measured during the first hours of life may be an effective screening tool for congenital heart disease [1-2]. The transition from fetus to newborn is a complex physiological process. After initial raises in SpO2 during the first minutes of life, SpO2 seems to be stable until 20-24 hours of life. Large number of studies finds that mean SpO2 is about 97-98%, with the normal range from 94 to 100% [3-5]. However, SpO2 is lower in children born at high altitude. There are multiple perinatal factors such as birth weight, gestational age (GA), gender and mode of delivery could possible influence the SpO2 level in newborns. As part of an ICMR funded study evaluating the accuracy of pulse oximetry for detecting critical congenital heart disease, SpO2 was measured in each newborn in our hospital. The objective of the present study was to analyze the influence of birth weight, GA, mode of delivery and gender, on levels of SpO2 in healthy newborns.
2. Material and Methods
This was a prospective study conducted in the Pediatric Department at Acharya Vinoba Bhave Rural Hospital (AVBRH), from January 2013 to December 2014. AVBRH is a 1206 bedded fully equipped teaching Hospital attached to the Jawaharlal Nehru Medical College with state of the art facilities at Sawangi Meghe, Wardha, India. An inclusion criterion was neonates with more than 34 weeks gestation. The exclusion criteria were outborn babies, neonates received supplemental oxygen or assisted ventilation, neonates with a prenatal diagnosis of duct dependent circulation by fetal echocardiography, and low birth weight (LBW) babies. The SpO2 measurements were performed using a Massimo Single Extraction Technology handheld pulse oximeter with a neonatal reusable Nellcor SpO2 sensor OXI-A/N probe. For each newborn, SpO2 was measured by trained social worker of the newborn within the first 6 hours of life.
The probe was held manually to the sole of the foot. Neonatal details such as date and time of birth, birth weight, sex, gestational age as well as maternal details, including her age, medical illness and pregnancy related problems were recorded. Labor details like presentation, duration, spontaneous or induced delivery, evidence of fetal distress, and passage of meconium were noted. An informed consent was obtained from parents (preferably by mother) before initial screening. The study protocol was approved by the ethical committees of the Institute.
3. Statistical Analysis
SPSS software version 17 was used for the statistical analysis. Data are presented as means (SD) and analyzed with 2-tailed t tests when normally distributed. A P value <0.05 was considered to be statistically significant.
4. Results
A total of 6101 neonates were born at the hospital during the period of January 2013 to December 2014 and registered in the CCHD screening project. For 68 neonates (1.1%), the first SpO2 was <95% and they were not included in the further analyses. 1958 neonates with weight less than 2.5 kg were excluded from the study. A total of 4075 neonates (1961 boys and 2114 girls) fulfilled the criteria for inclusion in the final analyses. The mean oxygen saturation for all new-borns was 98.62±1.19. Mean levels were slightly higher in boys 98.64±1.19 than in girls 98.60±1.18 (P<0.01), but no statistical significant gender difference existed when corrected for weight. The mean age at the time for measurement of SpO2 was 4 hr. The mean birth weight of the neonates was 2.81±0.27 Kg and the mean GA was 38.64±1.29 weeks. SpO2 was not related to GA when analyzed by oneway ANOVA (F: 0.88; P>0.01). No statistical significant difference in SpO2 was found in children born by caesarean section (98.62±1.20) than in those delivered vaginally (98.62±1.17). Figure 1 shows the box plot of mean oxygen saturation (SpO2) (Mean; 95% CI) in relation to type of deliver. The mean SpO2 with 95% CI or SD for different groups of birth weight is given in Table 1. There was no significant decrease in oxygen saturation with increasing birth weight (P>0.01), when analyzed by oneway ANOVA.
|
Birth Weight (gm) |
Number |
SpO2 (Mean±SD) |
|
2500-2999 |
2849 |
98.63±1.19 |
|
3000-3500 |
1092 |
98.60±1.18 |
|
3500-3999 |
123 |
98.60±1.23 |
|
>4000 |
16 |
98.33±1.24 |
Table 1: Oxygen Saturation measured within 6 hours after birth in healthy newborns with gestational age >34weeks and birth weight >2500gm relation to birth weight.
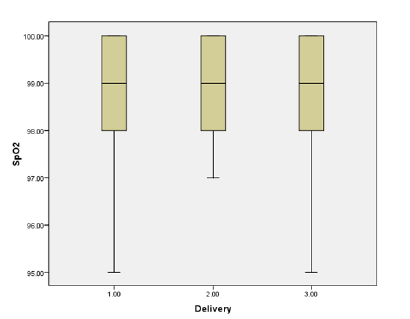
Figure 1: Mean oxygen saturation (SpO2) (Mean; 95%CI) in relation to type of delivery (1: Vaginal delivery; 2: Instrumental; 3: Caesarean Section) in healthy newborns.
5. Discussion
An important component of intensive care of the newborn is oxygen supplementation. To minimize the pulmonary toxicity or the consequences of hypoxemia or hyperoxia, careful monitoring is required. The two main complications of excessive oxygen are lung injury and retinopathy of prematurity. It has been suggested that the FiO2 could be determined by monitoring infants’ SpO2 by using pulse Oximetry. Pulse oximetry allows us to continuously measure arterial oxygenation noninvasively. The main use of pulse oximetry is to detect acute episodes of reduced oxygenation. Røsvik A et al. [6] mentioned that the mean SpO2 measured in all children was 98% which is similar to our study i.e. 98.2%. However, Levesque et al. [7] found a lower mean SpO2 of 97% in 718 healthy newborns. O’Brien et al. [8] found that levels of SpO2 were stable few minutes after birth thereafter until a minor decline during the 20?24 h of age, whereas Levesque et al. [7] found a slight increase in SpO2 from admission to the nursery to 24 h postnatally. We did not perform longitudinal measurements, but our study suggests that levels of SpO2 do not vary significantly by age from 2 to 24 h postnatally. Røsvik A et al. [6] demonstrated levels of SpO2 during the first day of life were related to birth weight and mode of delivery in healthy newborns. They also reported mean SpO2 was higher in children with a low birth weight and varied from 98.3% in those with a birth weight of 2750?2999 g to 97.6% in those with a weight above 4500 g same finding was present in our study also. Røsvik A et al. [6] didn’t know the reason for the relation between birth weight and SpO2. As weight increases with GA, differences in SpO2 could possibly be related to hemodynamic differences related to GA. SpO2 was not related to GA and did not differ between boys and girls after correction for birth weight.
It has been found that babies born by caesarean section have lower SpO2 values when compared with those born through vaginal delivery, and take a longer time to attain SpO2 values of >85% [9]. Røsvik A et al. [6] reported that SpO2 was higher in children born by cesarean section than in those delivered vaginally, and this difference did not explain. It has been mentioned that children born by cesarean section have lower levels of SpO2 during the first minutes of life, probably due to increased amount of lung fluid. However, this difference was equalized within a few minutes [9].
An effect of either maternal analgesia or anesthesia on SpO2 was not demonstrated by Kamlin CO et al. [4]. Pulse oximetry data can be obtained within 1 to 2 minutes after birth and gives a continuous, noninvasive measure of SpO2 and heart rate. Kamlin CO et al. [4] reported that gestation and the presence of labor have an effect on SpO2 in the minutes after birth. Ruegger C et al. [10] found that birth weight had a positive correlation to the difference between pre and postductal values. Toth et al. [11] in his study, measured the pre and postductal SpO2 with pulse oximeter of 50 vaginally born healthy term infants. They found SpO2 at 2 minutes of age as low as 34%, and these infants took 12 to14 minutes to reach SpO2 >95%, and that preductal SpO2 rose more quickly than the postductal value. Our results confirm that measurement of SpO2 is an easy and reliable test in newborns. Ruegger C et al. [10] demonstrates that left hand pulse oximetry measurements do not significantly differ from the right hand preductal values. Using the Masimo SET technology, Kamlin CO et al. [4] measured the SpO2 of newly born infants who were not resuscitated or given supplemental oxygen.
6. Conclusion
We conclude that in healthy newborns, level of SpO2 measures within 6hours of life is negatively correlated with birth weight but not statistically significant. Also, no correlation was found in neonate born by caesarean section than in neonate delivered vaginally.
Conflict of Interest
None
Funding
As part of an Indian Council of Medical Research (ICMR) funded study evaluating the accuracy of pulse oximetry for detecting critical congenital heart disease.
Acknowledgment
We would like to extend our sincere appreciation to the Indian Council of Medical Research, New Delhi for its funding.
References
- Bakr AF, Habib HS. Normal values of pulse oximetry in newborns at high altitude. J Trop Pediatrics 51 (2005): 170-173.
- Meberg A, Bru gman S, Due R Jr, Eskedal L, Fagerli I, et al. First day of life pulse oximetry screening to detect congenital heart defects. J Pediatr 152 (2008): 761-765.
- Dawson JA, Davis PG, O’Donnell CP, Kamlin CO, Morley CJ. Pulse oximetry for monitoring infants in the delivery room: a review. Arch Dis Child Fetal Neonatal Ed 92 (2007): F4-F7.
- Kamlin CO, O’Donnell CP, Davis PG, Morley CJ. Oxygen saturation in healthy infants immediately after birth. J Pediatr 148 (2006): 585-589.
- Mariani G, Dik PB, Ezquer A, Aguirre A, Esteban ML, et al. Preductal and postductal O2 saturation in healthy term neonates after birth. J Pediatr 150 (2007): 418-421.
- Røsvik A, Øymar K, Terje J, Berget KM. Oxygen saturation in healthy newborns; influence of birth weight and mode of delivery. J Perinat Med 37 (2009): 403-406.
- Levesque BM, Pollack P, Griffin BE, Nielsen HC. Pulse oximetry: what’s normal in the newborn nursery? Pediatr Pulm 30 (2000): 406-412.
- O’Brian LM, Stebbens VA, Poets CF, Heycock EG, Southall DP. Oxygen saturation during the first 24 hours of life. Arch Dis Child Fetal Neonatal Ed 83 (2000): F35-F38.
- Rabi Y, Yee W, Chen SY, Singhal N. Oxygen saturation trends immediately after birth. J Pediatr 148 (2006): 590-594.
- Ruegger C, Bucher HU, Mieth RA. Pulse oximetry in the newborn: Is the left hand pre or postductal? BMC Pediatrics 10 (2010): 35.
- Toth B, Becker A, Seelbach-Gobel B. Oxygen saturation in healthy newborn infants immedi-ately after birth measured by pulse oximetry. Arch Gynecol Obstet 266 (2002): 105-107.
Article Views: 830
Journal Statistics





Discover More: Recent Articles


