Work-Related Musculoskeletal Disorders among Greek Dentists - A Nationwide Survey
Article Information
Berdouses EB1*, Sifakaki Maria2, Katsantoni A3, Andrikoula T1, Oulis CJ4
1Paediatric Dentist, Athens, Greece
2Paediatric Dentist, Clinical Instructor, Department of Paediatric Dentistry, National and Kapodistrian University of Athens, Greece
3Paediatric Dentist, Virginia, USA
4Professor Emeritus, Department of Operative Dentistry, National and Kapodistrian University of Athens, Athens, Greece
*Corresponding Author: Berdouses Elias, Paediatric Dentist, 22 Kodrou str, Halandri, Athens 152 31, Greece
Received: 16 September 2020; Accepted: 24 September 2020; Published: 06 October 2020
Citation: Berdouses EB, Sifakaki Maria, Katsantoni A, Andrikoula T, Oulis CJ. Work-Related Musculoskeletal Disorders among Greek Dentists - A Nationwide Survey. Dental Research and Oral Health 3 (2020): 169-181.
View / Download Pdf Share at FacebookAbstract
Background: Musculoskeletal disorders (MSDs) are a significant health problem among dental professionals. The aim of this survey was to investigate the prevalence of MSDs among Greek dentists and how they are correlated to the prevailing working conditions in practicing clinical dentistry.
Methods: The sample consisted of 1500 questionnaires filled out by telephone interviews of Greek dentists, randomly selected, nationwide. The questionnaire included dentist’s demographic and background data, whether being a specialist or a general dentist, working time during the day, number and duration of breaks, dentist’s posture and patient’s position, whether practicing four-handed dentistry and the recorded MSDs. Categorical variables have been summarized through absolute and relative % frequencies and continuous ones through their median and interquartile range. Associations between categorical variables have been tested through the chi-square test.
Results: The results indicated that 54.1% of the sample experienced MSDs, the prevalence of the problems was increased after 10 years of practice (33.2%) and was doubled after 30 years of practice in the 69.6% of the cases. The most prevalent work-related MSDs was back problems (18.6%), hands problems (18.6%), cervical syndrome (14.0%), shoulder (10.5%), lower leg problems (11.9%) and carpal tunnel syndrome (8.3%). Only 12.7% of the dentists practice four-handed dentistry in a seated position with an assistant next to a prone patient. The statistics demonstrated that there was little difference in the prevalence of MSDs between those who practiced four-handed dentistry and those who didn’t. However there was a change in the distribution of MSDs between different parts of the body.
Conclusions: MSD is a significant occupational problem among dentist which is affected by the working posture an
Keywords
Musculoskeletal Disorders, Risk Factors, Questionnaire Survey, Health Effects, Four-Handed Dentistry, Method of Work, Ergonomics
Musculoskeletal Disorders articles; Risk Factors articles; Questionnaire Survey articles; Health Effects articles; Four-Handed Dentistry articles; Method of Work articles; Ergonomics articles
Musculoskeletal Disorders articles Musculoskeletal Disorders Research articles Musculoskeletal Disorders review articles Musculoskeletal Disorders PubMed articles Musculoskeletal Disorders PubMed Central articles Musculoskeletal Disorders 2023 articles Musculoskeletal Disorders 2024 articles Musculoskeletal Disorders Scopus articles Musculoskeletal Disorders impact factor journals Musculoskeletal Disorders Scopus journals Musculoskeletal Disorders PubMed journals Musculoskeletal Disorders medical journals Musculoskeletal Disorders free journals Musculoskeletal Disorders best journals Musculoskeletal Disorders top journals Musculoskeletal Disorders free medical journals Musculoskeletal Disorders famous journals Musculoskeletal Disorders Google Scholar indexed journals Risk Factors articles Risk Factors Research articles Risk Factors review articles Risk Factors PubMed articles Risk Factors PubMed Central articles Risk Factors 2023 articles Risk Factors 2024 articles Risk Factors Scopus articles Risk Factors impact factor journals Risk Factors Scopus journals Risk Factors PubMed journals Risk Factors medical journals Risk Factors free journals Risk Factors best journals Risk Factors top journals Risk Factors free medical journals Risk Factors famous journals Risk Factors Google Scholar indexed journals Questionnaire Survey articles Questionnaire Survey Research articles Questionnaire Survey review articles Questionnaire Survey PubMed articles Questionnaire Survey PubMed Central articles Questionnaire Survey 2023 articles Questionnaire Survey 2024 articles Questionnaire Survey Scopus articles Questionnaire Survey impact factor journals Questionnaire Survey Scopus journals Questionnaire Survey PubMed journals Questionnaire Survey medical journals Questionnaire Survey free journals Questionnaire Survey best journals Questionnaire Survey top journals Questionnaire Survey free medical journals Questionnaire Survey famous journals Questionnaire Survey Google Scholar indexed journals Health Effects articles Health Effects Research articles Health Effects review articles Health Effects PubMed articles Health Effects PubMed Central articles Health Effects 2023 articles Health Effects 2024 articles Health Effects Scopus articles Health Effects impact factor journals Health Effects Scopus journals Health Effects PubMed journals Health Effects medical journals Health Effects free journals Health Effects best journals Health Effects top journals Health Effects free medical journals Health Effects famous journals Health Effects Google Scholar indexed journals Four-Handed Dentistry articles Four-Handed Dentistry Research articles Four-Handed Dentistry review articles Four-Handed Dentistry PubMed articles Four-Handed Dentistry PubMed Central articles Four-Handed Dentistry 2023 articles Four-Handed Dentistry 2024 articles Four-Handed Dentistry Scopus articles Four-Handed Dentistry impact factor journals Four-Handed Dentistry Scopus journals Four-Handed Dentistry PubMed journals Four-Handed Dentistry medical journals Four-Handed Dentistry free journals Four-Handed Dentistry best journals Four-Handed Dentistry top journals Four-Handed Dentistry free medical journals Four-Handed Dentistry famous journals Four-Handed Dentistry Google Scholar indexed journals Method of Work articles Method of Work Research articles Method of Work review articles Method of Work PubMed articles Method of Work PubMed Central articles Method of Work 2023 articles Method of Work 2024 articles Method of Work Scopus articles Method of Work impact factor journals Method of Work Scopus journals Method of Work PubMed journals Method of Work medical journals Method of Work free journals Method of Work best journals Method of Work top journals Method of Work free medical journals Method of Work famous journals Method of Work Google Scholar indexed journals Ergonomics articles Ergonomics Research articles Ergonomics review articles Ergonomics PubMed articles Ergonomics PubMed Central articles Ergonomics 2023 articles Ergonomics 2024 articles Ergonomics Scopus articles Ergonomics impact factor journals Ergonomics Scopus journals Ergonomics PubMed journals Ergonomics medical journals Ergonomics free journals Ergonomics best journals Ergonomics top journals Ergonomics free medical journals Ergonomics famous journals Ergonomics Google Scholar indexed journals
Article Details
1. Background
Musculoskeletal disorders (MSDs) seem to occur commonly among dentists during the course of their career due to the physically and mentally stressful nature of their work. Work-related musculoskeletal disorders are problems of the musculoskeletal system that significantly causes workplace problems thus affecting occupational health, productivity, and career of working population [1]. The high prevalence of MSDs in dentistry has been the subject of numerous studies worldwide and has been well documented. Dentistry is a demanding profession and dentists seem to report higher frequency and severity of health problems in comparison with other high-risk medical professionals [2]. The mechanisms leading to work related MSDs are multifactorial. Various risk factors have been identified such as prolonged static positions, allowing good sight in the narrow work area of the patient’s mouth, vibrations, repetitive movements and poor positioning, mental stress, uncomfortable and asymmetric positions, standing or sitting positions and maintenance of the head, neck and shoulders in fixed positions for long intervals [2-11]. In Greece there are two studies [12, 13] investigating occupational risk factors and MSDs and one study focused on MSDs in dentists [14], concerning only one city though. Several studies report the high prevalence of MSDs among dentists in other countries, although some of them refer to the past days or months and not to all the years of practice [7, 11, 14, 15]. An important issue that is missing from most of the investigations is the symptoms that accompany the MSDs, as these define how the MSDs affect dentists’ clinical practice and quality of life. The aim of the present study is to:
- Record the prevalence of the MSDs among Greek dentists.
- Investigate the influence of work-related risk factors on the occurrence of Musculoskeletal Disorders.
- Record the prevalence of other symptoms than pain (stiffness, discomfort, fatigue) which were not reported in none earlier studies.
- Evaluate the effect of the sitting or standing position or the practice four-handed dentistry on MSD.
2. Methods
The Hellenic Statistical Authority (HSA) in 2019 [16] reported that out of the 13,300 dentists in the county 6,792 (51.1%) were males and 6,508 (48.9%) were females. Based on these data and the composition of the males and females on every prefecture of the country a sample of 1968 dentists (1007 males and 961 females) was selected from the Hellenic Dental Association (HDA) list. The sample was randomly selected with similar demographics with the data from HSA. Out of 1968 dentists that were contacted, 1500 accepted to be interviewed (855 males and 645 females). The dentists were interviewed over the phone on anonymous questionnaire focused on the work-related MSDs. The interviewer did not know the name or the location of the dentist that was interviewed. The HDA list of dentists was rearranged in random order using the software STATA 11.2 (StataCorp LLC, TX, USA) and then they were contacted by phone. The dentists were informed for the purpose of the questionnaire and the origin of the survey.
The questionnaire included four different sections. The first section referred to the background data on gender, age, demographic information, number of years since graduation, location of the University of graduation, acquired specialization if any, and frequency of exercise. The second section included questions on the mode of practice. The third section recorded the presence of any MSD during their years of practice until present, the symptoms reported, the duration of MSDs in months, whether the problem has been solved or not and whether the problem has affected the dentist's effectiveness on their clinical practice or their life quality (on a scale ranging from 0 to 10). The final section dealt identifying the problems that have been definitively solved and the treatment applied. Statistical analysis of the results was performed using statistical software STATA 11.2 (StataCorp LLC, TX, USA). Categorical variables have been summarized through absolute and relative frequencies and continuous ones through their median and interquartile range because their distribution was significantly deviating from the normal distribution. Normality was checked through the Kolmogorov–Smirnov test. Associations between categorical variables are presented through two-way contingency tables and their significance has been assessed through the chi-square test. Differences in the distribution of continuous variables between levels of a categorical (binary) variable have been assessed through the non-parametric Mann-Whitney U Test. P-values of less than 0.05 have been considered as statistically significant.
3. Results
The survey was nationwide among dentists randomly selected from all 52 geographical prefectures of the country. The biggest group in this study consisted of dentists who practiced in Attica. The response rate was 84.9% for the males, 67.1% for the females and 76.2% overall. The sample consisted of 57% male and 43% female dentists. The majority of those responded (83.9%) were general dentists-without specialization and 15.9% were specialists. Almost one quarter of those questioned had studied overseas (24.5%) and the rest of them graduated from a Greek dental school (75.5%). The mean age of the dentists among the study group was 45 years old (37-53 years old). The mean years of practice was 18 (9-26 years) and the average hours of practice duration per day was 8 (7-9 hours/day) (Table 1). The data from this study show that the majority of dentists in the study work in a sitting position whether with (28.5%) or without an assistant (38.3%). It was also found that about one fifth (18.9%) of the sample works in a standing position and the majority of them (16.3%) without any assistant. More than half (54.5%) of the dentists work with the patient in a semi-supine position, one quarter (24.3%) of them in a supine and 20.5% in a sitting position. Only 12.7% of the respondent dentists always practice four-handed dentistry (in a sitting position with an assistant next to a prone patient). The results also show that as many as 59.4% of the respondents work with at least one break and a big proportion of them (40.4%) work without any break. Half of them have less than 7-minute breaks and less than 30-minute appointments. In addition, over 69% exercise but only 33.2% regularly. The reported disorders are summarized in Table 2. More than half (54.1%) of the sample reported at least one MSD. The most frequent MSD was back problems (21.7%) followed by hands problems (18.6%), cervical syndrome (14%) and leg problems (11.9%). Carpal tunnel syndrome has been experienced by 8.3% of the respondents. Almost 6% reported experiencing circulatory system problems and sciatica (6.3% and 6.1% respectively). The detailed list of MSDs prevalence by geographical province is presented in Table 3. The most common symptom reported by those having a cervical syndrome was neck pain (68.1%) followed by dizziness (28.1%). Pain and wariness were the most frequent symptoms occurred in those having finger/hand problems (39.9% and 35.6%), carpal tunnel syndrome (47.6% and 28.2%), back problems (64.9% and 24.6%) and leg problems (36.5% and 55.6%). In order to gain a better understanding in the nature of MSDs, the correlation between MSDs and various risk factors was studied. As far as gender is concerned, females were found to experience much more frequent headache and neck pain (4.7% and 12.2% respectively, p=0.002) compared to males. However no statistically significant difference was found between genders in the rest of MSDs (Table 4). The number of years of practice also influenced the prevalence of MSDs (Figure 1). The frequency of MSDs is increased after ten years of practice with the highest value being observed during the third decade of practice (69.6%, p=0.001) then the frequency levels for the next decade. Among all reported MSDs, leg and circulatory system problems almost double in frequency from the third (20-29 years) to the fourth decade (30+ years) of practice.
Although no statistically significant correlation was found between the overall presence of musculoskeletal health related problems and break duration, there have been two MSDs in which a certain degree of correlation was found. More specifically, those who took no breaks had almost double the frequency of circulatory system problems and 1.5 fold frequency of sciatica compared to those who took less than five-minute breaks. As for the relationship between MSDs and the presence of assistant, the authors noted that both those who worked with and without an assistant had MSDs. However what differs is the problem distribution. Absence of assistant seems to affect dentists’ lower part of the body, while having an assistant impacts the upper part. Data show that 16% of those who had an assistant presented cervical syndrome, 22.6% hands problems and 10.2% carpal tunnel syndrome. These percentages were higher than the respective ones of those who worked without an assistant. The latter had higher prevalence of leg problems (15%), circulatory system problems (7.6%) and sciatica (6.6%). Similarly four-handed dentistry was one of the categorical variables that have been examined for affecting the occurrence of MSDs. Those who practiced four-handed dentistry reported more frequently cervical syndrome (17.4%) and those who didn’t suffered from leg (12%) and circulatory system (7.3%) problems (Table 5). The analysis showed statistically significant dependence (p<0.001) between the standing and seating working position and the presence of MSDs (63.4% and 52.4%, respectively). The authors found that those who worked standing had higher frequency of leg problems (26.8%), circulatory system problems (14.5%) and sciatica (9.2%) compared to those who worked seated (5.8%, 2.8% and 5% respectively) (Table 6). When compared by frequency of exercise MSDs were significantly more prevalent among those who didn’t exercise at all (70.3%) in comparison with those who practiced regularly (40.3%). Respondents who practice regularly reported significantly less back (14.5%), leg (6.3%) and circulatory system (2.7%) problems in comparison to those who didn’t practice at all. Interestingly dentists who took rare exercise didn’t seem to have a significant decline in the prevalence of MSDs compared to those who didn’t exercise at all. The effects of health problems on quality of life and work efficiency were questioned to the sample in a scale ranging from 0 to 10. The results indicated that sciatica, cervical syndrome and shoulder problem had the highest effect on the quality of dentists’ life. Additionally, finger/hands problems, carpal tunnel syndrome and sciatica were the problems highest marked on the scale of the effect on the work efficiency. When dentists were asked, what was the treatment that was chosen in cases of cervical syndrome, leg and circulatory system problem the majority of the responses was either no treatment or take a rest. Rest and medication were the most popular treatment choices among those who had shoulder, back and hands problems. Those who suffered from sciatica did nothing or took medication so as to treat the disorder. Musculoskeletal comorbidity was high. In the total population 54.1% reported at least one MSD. Among those who suffered from at least one MSD, slightly over half of them (55.5%) reported only one MSD, 24.8% reported two MSDs, 11.3% reported three MSDs and 5% reported four MSDs (Figure 2).
|
Gender |
Overall N (%) |
p-value |
||
|
Male N (%) |
Female N (%) |
|||
|
Gender |
855 (100.0) |
645 (100.0) |
<0.001 |
|
|
Specialization |
||||
|
Yes |
141 (16.5) |
97 (15.0) |
238 (15.9) |
|
|
No |
713 (83.4) |
546 (84.7) |
1259 (83.9) |
|
|
NA |
1 (0.1) |
2 (0.3) |
3 (0.2) |
|
|
Four-handed dentistry |
||||
|
Yes |
112 (13.1) |
78 (12.1) |
190 (12.7) |
|
|
No |
615 (71.9) |
475 (73.6) |
1090 (72.7) |
|
|
Unknown |
128 (15.0) |
92 (14.3) |
220 (14.7) |
|
|
Patient position |
<0.001 |
|||
|
Supine |
205 (24.0) |
159 (24.7) |
364 (24.3) |
|
|
Semi supine |
434 (50.8) |
384 (59.5) |
818 (54.5) |
|
|
Seated |
209 (24.4) |
99 (15.3) |
308 (20.5) |
|
|
NA |
7 (0.8) |
3 (0.5) |
10 (0.7) |
|
|
Exercise |
||||
|
Rarely |
314 (36.7) |
235 (36.4) |
549 (36.6) |
|
|
Not at all |
271 (31.7) |
181 (28.1) |
452 (30.1) |
|
|
Regularly |
270 (31.6) |
228 (35.3) |
498 (33.2) |
|
|
NA |
0 (0.0) |
1 (0.2) |
1 (0.1) |
|
|
Method of working |
0.001 |
|||
|
Seated/assistant |
234 (27.4) |
194 (30.1) |
428 (28.5) |
|
|
Seated/no assistant |
307 (35.9) |
268 (41.6) |
575 (38.3) |
|
|
Standing/assistant |
26 (3.0) |
13 (2.0) |
39 (2.6) |
|
|
Standing/no assistant |
165 (19.3) |
80 (12.4) |
245 (16.3) |
|
|
NA |
123 (14.4) |
90 (14.0) |
213 (14.2) |
|
Table 1: Demographic and other characteristics.
|
Gender |
Overall N (%) |
p-value |
||
|
Male N (%) |
Female N (%) |
|||
|
MSD related health problems |
||||
|
Yes |
460 (53.8) |
351 (54.4) |
811 (54.1) |
|
|
No |
360 (42.1) |
282 (43.7) |
642 (42.8) |
|
|
NA |
35 (4.1) |
12 (1.9) |
47 (3.1) |
|
|
Hands problems |
||||
|
Yes |
150 (17.5) |
129 (20.0) |
279 (18.6) |
|
|
No |
705 (82.5) |
516 (80.0) |
1221 (81.4) |
|
|
Cervical syndrome |
<0.001 |
|||
|
Yes |
95 (11.1) |
115 (17.8) |
210 (14.0) |
|
|
No |
760 (88.9) |
530 (82.2) |
1290 (86.0) |
|
|
Shoulder problem |
||||
|
Yes |
83 (9.7) |
74 (11.5) |
157 (10.5) |
|
|
No |
772 (90.3) |
571 (88.5) |
1343 (89.5) |
|
|
Back problem |
||||
|
Yes |
192 (22.5) |
133 (20.6) |
325 (21.7) |
|
|
No |
600 (70.2) |
479 (74.3) |
1079 (71.9) |
|
|
NA |
63 (7.4) |
33 (5.1) |
96 (6.4) |
|
|
Fingers/hands problem |
||||
|
Yes |
89 (10.4) |
74 (11.5) |
163 (10.9) |
|
|
No |
766 (89.6) |
571 (88.5) |
1337 (89.1) |
|
|
Elbow |
||||
|
Yes |
42 (4.9) |
30 (4.7) |
72 (4.8) |
|
|
No |
813 (95.1) |
615 (95.3) |
1428 (95.2) |
|
|
Carpal Tunnel Syndrome |
<0.05 |
|||
|
Yes |
60 (7.0) |
64 (9.9) |
124 (8.3) |
|
|
No |
795 (93.0) |
581 (90.1) |
1376 (91.7) |
|
|
Leg problem |
0.001 |
|||
|
Yes |
123 (14.4) |
55 (8.5) |
178 (11.9) |
|
|
No |
732 (85.6) |
590 (91.5) |
1322 (88.1) |
|
|
Circulatory system |
||||
|
Yes |
54 (6.3) |
40 (6.2) |
94 (6.3) |
|
|
No |
801 (93.7) |
605 (93.8) |
1406 (93.7) |
|
|
Sciatica |
<0.05 |
|||
|
Yes |
64 (7.5) |
27 (4.2) |
91 (6.1) |
|
|
No |
791 (92.5) |
618 (95.8) |
1409 (93.9) |
|
Table 2: Musculoskeletal disorders.
|
Geographical Department |
N |
Yes n (%) |
|
Attica |
441 |
249 (56.5) |
|
Thessalonica |
76 |
34 (44.7) |
|
Epirus |
50 |
29 (58.0) |
|
Thessaly |
56 |
40 (71.4) |
|
Thrace |
31 |
19 (61.3) |
|
Crete |
114 |
73 (64.0) |
|
Macedonia |
187 |
109 (58.3) |
|
Aegean Islands |
86 |
47 (54.7) |
|
Ionian Islands |
30 |
13 (43.3) |
|
Peloponnese |
277 |
145 (52.3) |
|
Central Greece |
105 |
53 (50.5) |
|
Total |
1453 |
811 (55.8) |
MSC related health problems *chi-square=17.961, p<0.01
Table 3: Prevalence of MSDs by geographical region.
|
N |
Male |
Female |
Total |
Significance |
|
855 |
645 |
1500 |
||
|
Yes - n (%) |
Yes - n (%) |
Yes - n (%) |
||
|
Headache (Cervical) |
16 (1.9) |
30 (4.7) |
46 (3.1) |
<0.05 |
|
Neck Pain (Cervical) |
64 (7.5) |
79 (12.2) |
143 (9.5) |
<0.05 |
|
Pain (Shoulder) |
46 (5.4) |
41 (6.4) |
87 (5.8) |
|
|
Pain (Fingers/hands) |
36 (4.2) |
29 (4.5) |
65 (4.3) |
|
|
Pain (Elbow) |
15 (1.8) |
18 (2.8) |
33 (2.2) |
|
|
Pain (Carpal Tunnel) |
26 (3.0) |
33 (5.1) |
59 (3.9) |
<0.05 |
|
Pain (Leg) |
40 (4.7) |
25 (3.9) |
65 (4.3) |
Table 4: Gender difference in pain and headache.
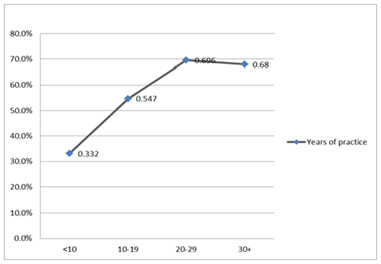
Figure 1: Prevalence of MSDs by years of Practice.
|
Yes |
No |
Total |
p-value* |
|
|
N (%) |
N (%) |
N (%) |
||
|
MSC related health problems |
87 (45.8) |
617 (56.7) |
704 (55.0) |
0.005 |
|
Back problem |
40 (21.1) |
241 (22.2) |
281 (22.0) |
0.727 |
|
Hands problems |
27 (14.2) |
216 (19.8) |
243 (19.0) |
0.068 |
|
Cervical syndrome |
33 (17.4) |
159 (14.6) |
192 (15.0) |
0.324 |
|
Fingers/hands problem |
16 (8.4) |
125 (11.5) |
141 (11.0) |
0.214 |
|
Shoulder problem |
15 (7.9) |
118 (10.8) |
133 (10.4) |
0.220 |
|
Leg problem |
7 (3.7) |
131 (12.0) |
138 (10.8) |
0.001 |
|
Carpal Tunnel Syndrome |
10 (5.3) |
93 (8.5) |
103 (8.1) |
0.126 |
|
Circulatory system |
5 (2.6) |
80 (7.3) |
85 (6.6) |
0.016 |
|
Sciatica |
10 (5.3) |
65 (6.0) |
75 (5.9) |
0.702 |
|
Elbow |
7 (3.7) |
57 (5.2) |
64 (5.0) |
0.366 |
Table 5: Prevalence of MSDs for dentists working four-handed dentistry.
|
N |
Seated |
Standing |
Total |
Significance |
|
1004 |
448 |
1452 |
||
|
Yes - n (%) |
Yes -n (%) |
Yes - n (%) |
||
|
MSC related health problems |
526 (52.4) |
284 (63.4) |
810 (55.8) |
≤0.001 |
|
Hands problems |
198 (19.7) |
80 (17.9) |
278 (19.1) |
|
|
Cervical syndrome |
158 (15.7) |
51 (11.4) |
209 (14.4) |
=0.005 |
|
Shoulder problem |
107 (10.7) |
49 (10.9) |
156 (10.7) |
|
|
Back problem |
217 (21.6) |
108 (24.1) |
325 (22.4) |
<0.05 |
|
Fingers/hands problem |
110 (11.0 |
53 (11.8) |
163 (11.2) |
|
|
Elbow |
49 (4.9) |
23 (5.1) |
72 (5.0) |
|
|
Carpal Tunnel Syndrome |
85 (8.5) |
38 (8.5) |
123 (8.5) |
|
|
Leg problem |
58 (5.8) |
120 (26.8) |
178 (12.3) |
≤0.001 |
|
Circulatory system |
28 (2.8) |
65 (14.5) |
93 (6.4) |
≤0.001 |
|
Sciatica |
50 (5.0) |
41 (9.2) |
91 (6.3) |
<0.05 |
Table 6: Prevalence of MSDs for dentists using standing of seated positions.
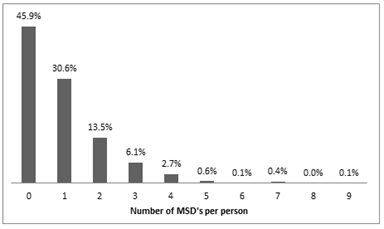
Figure 2: Number of MSDs per person.
4. Discussion
The sample of this study included 57.0% males and 43.0% females. It is evident that in this sample males are slightly overrepresented in comparison to the demographic HSA data [16] (51.1% males and 48.9% females). Another characteristic of this study is that the sample was interviewed over the telephone. During the interview the interviewer has the opportunity to ask relevant questions if a response is not clear or the dentist did not understand exactly a question. There is a possibility the information from an interview to be more accurate than by filling in a questionnaire. In the literature, most of the studies until now are by mailing a questionnaire. One of the limitations of all the studies when any kind of questionnaire is used to evaluate MSD is the subjectivity of the responses regarding the qualitative description of the symptoms and also the fact that practitioners with recent episodes will describe the event more accurately and thus may affect the results. In this cross-sectional study the prevalence of MSDs was 54.1%. The most prevalent sites that dentists experienced musculoskeletal symptoms were back, hands, legs and cervical syndrome. Pain was the most common symptom reported in all kinds of MSDs. Other frequent symptoms reported were weariness and rigidity. All other symptoms (dizziness, reflection, numbness and lassitude) were less commonly reported. In the literature there are conflicting findings regarding the prevalence of different types of MSD symptoms. For example, in our study prevalence of low back problem was found to be 21.7% which is in the same range with a study from Finland (28%) [17] but it is lower prevalence from a study in USA [18] in general practitioners (56%) and another study from Greece (46%) [14]. Similar relationship was found and for the overall prevalence of MSDs. Regarding the prevalence of all MSD symptoms, our results 54,1% are similar with the Finnish study 51% [17] and lower than other studies from USA, 64% [18], Greece 62% [14], Saudi Arabia (59.2%) [19], India (78%) [20], Australia (87.2%) [21], Lithuania (86.5%) [2], and Turkey (94%) [22]. The prevalence of our study was also higher than three older studies [23-25] that have reported prevalence between 36% and 42%. There is a clear increase in the reported prevalence of MSD in comparison with these old studies. This increase in the prevalence of MSD may be attributed to the changes in the working environment of the dental office [17, 26].
In this study there is a steady increase in the frequency of MSD’s as the years of practice increase and simultaneously the age of the practitioner. It reached the highest value during the third decade of practice and then levels. One explanation for the levelling may be that during the fourth decade dentists with serious MSD’s stop practicing. In the literature there are some studies [18, 27-29] that report a high prevalence of MSD during the first 5 or 10 years of practice which is reduced in the following decades. This is a finding that is not supported by our data. Several variables have been investigated for their association with the presence of MSDs. In our study, the gender was positively correlated with the prevalence of some types of MSDs, as female dentists seem to experience more frequently headache and neck pain due to the cervical syndrome compared with males. On the contrary, when the overall prevalence between the two genders was evaluated it was found to be the same. In the literature there are mixed results. There are studies reporting that females present MSD in higher frequency [17, 18, 27, 30-33] another study by Decharat et al, [34] supporting the opposite and two studies [20, 35] report that both genders have the same prevalence of MSDs a finding in agreement with our study.
Our data suggest that dentists who worked seated experience about 10% less MSDs compared with the dentists standing which is a statistically significant difference. There was however a difference in the distribution of MSDs between different parts of the body. When operators worked standing MSDs occurred mainly in the lower part of their body (sciatica, leg and circulatory system problems). On the other hand, operators who worked seated experienced primarily cervical syndrome. A difference in the distribution of MSDs was also noted when four-handed dentistry was examined. Dentists who practiced four-handed dentistry presented higher frequency of cervical syndrome whereas sciatica, hands, back, leg and circulatory system problems occurred in those who didn’t. Similar results were found when the presence or absence of assistant was examined as a risk factor. Although four-handed dentistry decreases operator’s stress and fatigue and achieves maximum efficiency, the operator remains stationary for longer periods in static seated postures and this might be an explanation for the results found [11]. Our findings regarding the treatment taken to deal with MSDs are the following: the majority of the dentists did nothing, took rest or used drugs. A very small percentage of the affected respondents used other types of treatment such as physiotherapy, operation and exercise. In the literature we did not find any studies addressing this issue. It was also found very little evidence on the effect of ergonomics intervention on MSD. There are two reports [36, 37] suggesting that changes in the training, work station modification, a regular exercise program or even using different types of instruments used for carrying out a dental procedure do not affected the reported MSD. These studies had a short observation time and some limitations in the design and the bias [38] they show the clear need of quality studies in this area.
5. Conclusions
Competing Interests
The authors declare that they have no competing interests.
References
- Overall, this study clearly demonstrates that MSDs represent a significant problem among dental professionals. This finding is supported not only due to the high prevalence of MSDs reported but also due to the effect on the quality of life and work efficiency as perceived by them. The mean value of the effect on quality of life ranges from 1.9 to 4 and on work efficiency from 1 to 2.8. These results show that although MSDs have an effect on dentists’ life, they don’t seem to allow MSDs influence their work efficiency.
- The high prevalence of MSDs in dentists could be attributed to risk factors related to the special nature of the profession. High visual demands, adoption of prolonged static and uncomfortable postures for long periods of time, repetitiveness of motions, handling loads that demand forcefulness, workplace stress and lack of use of an operator stool that promotes the natural low back curve are common risk factors of MSDs.
- It was found the 66.8% are working seated but only 12.7% use 4-handed dentistry.
- The results of this study demonstrate the lack of ergonomics and deficiency of prophylactic activity among Greek dentists. Maintaining low back curve, use of magnification, proper adjustment of operator’s chair and patient’s position, avoidance of static postures and twisting, chairside directional stretching during breaks, stress management and strengthening exercises are strategies to address MSDs [15].
- Education on ergonomics and prophylactic activity should be implemented in undergraduate dental studies as well as in continuing education seminars. Dentists should be aware of the way to organize the method of work and be able to train their staff members in order to eliminate MSDs.
- Nermin Y. Musculoskeletal disorders (MSDs) and dental practice. part 1. General information-terminology, aetiology, work-relatedness, magnitude of the problem, and prevention. Int Dent J 56 (2006): 359-366.
- Puriene A, Janulyte V, Musteikyte M, et al. General health of dentists. Literature review, Stomatol. Balt. Dent. Maxillofac. J 9 (2007): 10-20.
- Szymanska J. Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Env. Med 9 (2002): 169-173.
- Rundcrantz BL, Johnsson B, Moritz U. Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutical aspects, Swed Dent J 14 (1990): 71-80.
- Al Wazzan KA, Almas K, Al Shethri SE, et al. Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Pr 2 (2001): 17-30.
- Walters E. How to live with failure and stress. Dent Manag 16 (1976): 20-24.
- Myers HL, Myers LB. “It’s difficult being a dentist”: stress and health in the general dental practitioner. Br Dent J 197 (2004): 89-93.
- Hayes M, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg 7 (2009): 159-165.
- Allen J. The exhaustive effects of dental practice. Dent Cosm 17 (1875): 482-483.
- Kierklo A, Kobus A, Jaworska M, et al. Work-related musculoskeletal disorders among dentists – a questionnaire survey. Ann Agric Env. Med 18 (2011): 79-84.
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc 134 (2003): 1344-1350.
- Devereux JJ, Vlachonikolis IG, Buckle PW. Epidemiological study to investigate potential interaction between physical and psychosocial factors at work that may increase the risk of symptoms of musculoskeletal disorder of the neck and upper limb. Occup Env. Med 59 (2002): 269-277.
- Alexopoulos EC, Burdorf A, Kalokerinou A. Risk factors for musculoskeletal disorders among nursing personnel in Greek hospitals. Int Arch Occup Environm Heal 76 (2003): 289-294.
- Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord 5 (2004).
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc 134 (2003): 1604-1612.
- Hellenic Statistical Authority. Infographic: Physicians and dentists 2018, (2019).
- Kerosuo E, Kerosuo H, Kanerva L. Self-reported health complaints among general dental practitioners, orthodontists, and office employees. Acta Odontol. Scand 58 (2000): 207-212.
- La Rochelle NR. Related Musculoskeletal Disorders Among Dentists and Orthodontists, Virginia Commonwealth University (2017).
- Abduljabbar TA. Musculoskeletal disorders among dentists in Saudi Arabia, Pakistan. Oral Dent J 28 (2008): 135-144.
- Muralidharan D, Fareed N, Shanthi M. Musculoskeletal Disorders among Dental Practitioners: Does It Affect Practice?. Epidemiol. Res. Int. Article ID (2013): 1-6.
- Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia, Aust. Dent. J 51 (2006): 324-327.
- Polat Z, Baskan S, Altun S, et al. Musculoskeletal symptoms of dentists from south-east turkey, Biotechnol. Biotechnol. Equip 21 (2007): 86-90.
- Powell M, Eccles JD. The health and work of two professional groups: dentists and pharmacists. Dent Pr 20 (1970): 373-378.
- Murtomaa H. Work-related complaints of dentists and dental assistants. Int Arch Occup Environm Heal 50 (1982): 231-236.
- Lehto TU, Helenius HYM, Alaranta HT. Musculoskeletal symptoms of dentists assessed by a multidisciplinary approach. Comm Dent Oral Epidemiol 19 (1991): 38-44.
- Ekberg K, Bjorkqvist B, Malm P, et al. Case-control study of risk factors for disease in the neck and shoulder area. Occup Env. Med 51 (1994): 262-266.
- Chowanadisai S, Kukiattrakoon B, Yapong B, et al. Occupational health problems of dentists in Southern Thailand. Int Dent J 50 (2000): 36-40.
- Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Ergon, Appl 29 (1998): 119-125.
- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Heal 45 (2007): 611-621.
- Purienu A, Balciuniene I, Janulyte V, et al. Specificity of chronic self-reported occupational hazards among male and female Lithuanian dentists. Acta Medica Litu (2008).
- American Dental Association Survey Center. 1997 survey of current issues in dentistry: Repetitive motion injuries. American Dental Association, Chicago (1997).
- Ayers KMS, Thomson WM, Newton JT, et al. Self-reported occupational health of general dental practitioners. Occup. Med. (Chic. Ill) 59 (2009): 142-148.
- Marshall E, Duncombe L, Robinson R, et al. Musculoskeletal symptoms in New South Wales dentists, Aust. Dent J 42 (1997): 240-246.
- Decharat S, Phethuayluk P, Maneelok S. Prevalence of musculoskeletal symptoms among dental health workers, Southern Thailand. Adv Prev Med (2016).
- Rankin JA, Harris MB. Stress and health problems in dentists. J Dent Pr. Adm 7 (1990): 2-8.
- Dehghan N, Aghilinejad M, Nassiri-Kashani MH, et al. The effect of a multifaceted ergonomic intervention program on reducing musculoskeletal disorders in dentists. Med J Islam Repub Iran 30 (2016): 1-5.
- Rempel D, Lee DL, Dawson K, et al. The effects of periodontal curette handle weight and diameter on arm pain: a four-month randomized controlled trial. J Am Dent Assoc 143 (2012): 1105-1113.
- Mulimani P, Hoe VCW, Hayes MJ, et al. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners (Review) Summary of findings for the main comparison, Cochrane Database Syst. Rev. Art. No (2018).


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 