A Comparative Finite Element Analysis of ‘Hexa-Zygomatic’ Implants vs Conventional Quad Zygomatic Implants for The Rehabilitation of Bilateral Maxillectomy Defects
Article Information
Abhay Datarkar, Priyanka Relan*, Arwa Pardiwala, Prashant Pandilwar, Eitan Mijiritsky
1Department of Oral and Maxillofacial Surgery, Government Dental College and Hospital, 440003, Nagpur, Maharashtra, India
2Department of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 6423906, Israel
*Corresponding Author: Priyanka Relan. Department of Oral and Maxillofacial Surgery, Government Dental College and Hospital, 440003, Nagpur, Maharashtra, India
Received: 9 March 2023; Accepted: 16 March 2023; Published: 31 March 2023
Citation: Abhay Datarkar, Priyanka Relan, Arwa Pardiwala, Prashant Pandilwar, Eitan Mijiritsky. A Comparative Finite Element Analysis of ‘Hexa-Zygomatic’ Implants vs Conventional Quad Zygomatic Implants for The Rehabilitation of Bilateral Maxillectomy Defects. Journal of Environmental Science and Public Health. 7 (2023): 37-43.
View / Download Pdf Share at FacebookAbstract
Restoration of bilateral maxillectomy defects is inherently challenging. Zygomatic implants are one of the non-bone grafting solutions for restoration of such defects which require minimum armamentarium and are widely available. The Quad Zygomatic Implants have a long track record in maxillectomy defects secondary to cancer ablative surgeries. In the current scenario, they are being used in COVID associated mucormycosis maxillectomy defects. Since there is a paucity in literature on the use of zygomatic implants in the above-mentioned malady, we have used finite element analysis to assess the longevity of the Quad Zygomatic Implants concept and the newer Hexa Zygomatic Implants concept for these types of cases. The finite element analysis showed similar results for both the concepts on simulation which leads to the conclusion whereas both are viable treatment modalities. The Quad Zygomatic Implants concept is the more economically favourable and practical solution. As this a finite element analysis study, clinical based studies with long follow-up may shed light on a more conclusive clinical outcomes.
Keywords
Quad Zygomatic Implants, Hexa Zygomatic Implants, finite element analysis, bilateral maxillectomy defects
Article Details
1. Introduction
The reconstruction of a maxillary defect after resection continues to pose a challenge for the reconstructive oral and maxillofacial surgeon. There are numerous alternatives for patients with maxillectomy defects in terms of functional and aesthetic rehabilitation. The currently available maxillary reconstructive techniques include placement of a prosthetic obturator, local and regional flaps, and microvascular free flaps.[1-5] The different reconstructive techniques have specific indications and advantages depending on the ablative defect, the medical status of the patient, and the patient’s prognosis. The maxillary obturator has a long history of effectively managing the functional, cosmetic, and psychological problems associated with a maxillectomy defect. However, when extensive resections are required, significant problems with obturator retention, support, and stability can be encountered after the ablation of retentive maxillary anatomy. Other options include placing implants without bone grafting in anatomical buttresses (such as the frontomaxillary, frontozygomatic, palatal vault, pterygomaxillary buttress, etc.). [6] Bone grafting methods to fill up maxillectomy deficits frequently include a two-stage operation with delayed implant placement, which is associated with donor-site morbidity. [7] As a result, the patient will have to wait longer to start their rehabilitation, which will result in more financial loss for the patients. In the functional and aesthetic rehabilitation of patients with maxillectomy defects, zygomatic implants continue to be a crucial non-grafting option. Zygomaticus implants were originally designed for reconstruction of the atrophic, edentulous maxilla.[8] Zygomatic implants have been used since their initial design by Nobel Biocare and introduction by Branemark in 1988, reducing the number of surgeries and length of time needed for the successful rehabilitation of such patients. [9]
The biomechanical demands of the extensive maxillectomy defects have prompted the search for alternative points of anchorage for zygomatic implants that allows stabilizing a prosthesis in young patients (30 years old or more) for restitution of function and form.
The initial plan was for placing one implant in each zygoma, bilaterally, along with at least two standard implants in the anterior sector. Using more than three implants on each side of the upper maxilla (5 implants system with anchorage in malar bone) to support the dental prosthesis, Bothur et al. [10] described a modification of the standard zygomatic implant placement technique. This avoided the need for bone graft procedures in the premaxillary zone. To determine the prognosis for this method, it would be fascinating to know the long-term outcomes. The fifth implant made a difference in prosthetic stability for the resorbed maxilla, according to a protocol for a pentagonal zygomatic implant system described by Dr. Guerrero and colleagues in 2008 [11].
The authors of this study have expanded on the concept given by Dr.Guerrero and colleagues by conceptualising the utility of ‘Hexa-Zygomatic’ implants for our cases of bilateral maxillectomy defects. An FEA study was thus conducted to compare this new concept and challenge the conventional use of Quad-Zygomatic implants considering the drawbacks and clinical scenario presented by our set of cases. The motivation for this new modification was that the existing literature in favour of Quad Zygomas have largely been for the rehabilitation of atrophic maxillae and maxillectomy defects secondary to cancer ablative surgeries. Thus, the purpose of this study was to review the biochemical outcome of patients who have had maxillectomy for pathologic reasons and have been reconstructed using Hexa-Zygomatic Implants concept and Quad-Zygomatic Implants concept.
2. Material and Methods
In the present study, a low maxillectomy defect was simulated and repaired with Quad Zygoma and Hexa Zygoma Concept using a maxillofacial model of the same volunteer that was previously built using CT scan data. The implants were subjected to vertical and lateral loads that simulated bite forces, and the distribution of stresses on the zygoma implants, supporting bones, superstructures, and abutments was analysed.
The head of a 42 years old male volunteer was scanned with a clinical CT scanner (Siemens Somatom Sensation) with a slice thickness of 0.625 mm and the data was saved as Digital Imaging and Communications in Medicine (DICOM) files. The subject was explained about the purpose of this study and consent was obtained for the use of the data. The DICOM data was imported into the software of GeoMagics Freeform and every bone was separated respectively in transverse and sagittal and coronal planes slice by slice so that those can be isolated and the models can be constructed by region growing. And then the models were exported as type STL (Stereo Lithographic) files which were imported into the software of Dassault Systemes to generate elemental subparts of various shapes like rod, beam, etc connected to each other in three planes by triangles. [12]
The process of dividing the structure into discrete number of elements and nodes is designated as discretization. Nodes and elements together are known as mesh. Mesh pattern is created. To increase accuracy division is increased, number of elements is increased. If the number of elements in a model are increased it would result in fine meshing. Increase in accuracy is accompanied by increase in complexity of mathematical calculation and system requirement. Greater variation of stresses are divided into elements.
Post Discretization material properties are designed for elements. Material properties designated are Young's modulus or modulus of elasticity, Poisson's ratio, density, yield strength, etc. Amongst the above properties, Young's modulus and Poisson's ratio are more significant.
Before simulation in the model, the boundary conditions were assigned. After boundary condition was assigned, loading was done to stimulate the conditions. Loading is to be done at specific nodes and it is designated in terms of forces or displacement created by force. Vertical loads of 150 N and 135 N were applied at the posterior and anterior implant respectively. All materials involved in the models were assumed to be isotropic, homogenous, linearly elastic and static. The implants in contact with the bone were assumed to be completely osseointegrated. The properties of materials used in this study, including Young’s modulus and Poisson’s ratio, were obtained from early literatures [13], and that of the bones were calculated according to Zannoni et al.’s study. They have proved that Young’s modulus has a fixed relationship with the apparent density of bones, which is equivalent to the gray value of the bones in CT images. So Young’s modulus differs depending on the area of bony materials [14]
After initial process is completed, model is ready for analysis. Before analysis, software checks the model or cross-verifies pre-processing. Stiffness is measured. The integral part of this step is displacement of node in three planes.
The displacements of each node in each of the three planes of space are then determined by solving a basic equation.
The displacement can be solved by the equation,
{F}= [K] {u}
{F}- Nodal force matrix
{U}=nodal displacement matrix and [K] = global stiffness matrix
The nodal displacement was computed and stresses was calculated.
The solution was derived, results were displayed and analysed
3. Results
In the study of biomechanics, an equivalent force known as the von Mises stress (VM) is widely used. The researchers can quickly determine the most dangerous area of the model since it can vividly depict the stress variations throughout the whole simulation. In this study, VM stresses on the supporting bones, Hexa Zygomatic implants and Quad Zygomatic implants were used to assess the distribution of loads. Pseudo-colors on the implant structures represent the stresses borne by the implants.
3.1 Von-Miss Stress
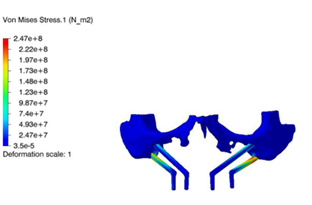
In Hexa-Zygomatic Concept, a load of 50N, 90N & 150N were applied on the bilateral anterior, middle and posterior implants respectively. The simulation of the same is depicted in Figure.1.
The most strained areas are depicted in red, while the unstressed regions are displayed in dark blue. In the above Fig.1, maximum stresses were observed at the point of emergence from the bone for all the 6 implants. The stresses though were found to be in the green zone of the VM stress colour spectrum which is considered to be the intermediate zone.
In Quad Zygomatic Implant Concept, the loads simulation applied on the anterior and posterior implants were 50 N and 150 N respectively as displayed in Figure 2.
After the application of loads, the simulated model revealed that maximum stresses were borne by the posterior implants, whereas as the anterior implants were in the blue zone along their entire length. The posterior implant on the right side showed the point of emergence of the implant from the bone to be in the mild stress zone depicted by the green colour on the VM stress colour spectrum. The posterior left implant depicted colours ranging from green, yellow and a tinge of red at the junction of bone-implant interface.
3.2 Displacement
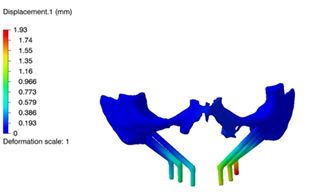
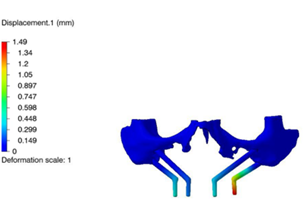
As the loads were applied on the implants, the implants exhibited some amount of displacement. A diagrammatic representation of the displacement of the Hexa-Zygomatic Implants and the Quad Zygomatic Implants are depicted in Figure 3 and Figure 4 respectively.
In Figure 3, it was observed that the part of all the 6 implants emerging from the bone showed minimal displacement. The implant-abutment interfaces of all the 6 implants were displaced moderately being within the blue-green spectrum. The highest amount of displacement was observed in the posterior most implant on the left side depicted by the red colour. In figure 4, the right anterior and posterior implants and the left anterior implants showed minimal displacement along their entire length depicted by blue colour. It was only in the left posterior implant that the implant-abutment interface showed a higher displacement as it was in the red colour on the spectrum. Nonetheless, the implant-bone interface of the said implant was within the blue colour on the spectrum.
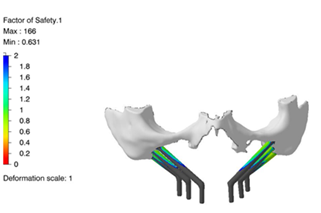
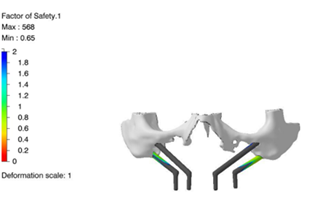
Upon these findings, it was deemed necessary to compute the safety factor which is the ratio between the strength of the material and maximum stress borne by the part. When the safety factor is below 1, the implant is at danger of failure due to breakage. In this FEA, the safety factor at no part of the implant in both Hexa-zygomatic and Quad zygomatic concepts was below 1 as can be seen in Figure.5 and Figure 6, respectively.
4. Discussion
Radical surgical excision of the jaws due to pathological reasons often leads to a severe deficit of the involved anatomical structures. Extensive surgery for maxillary tumour resection results in severe functional, emotional, and social impacts for patients. Moreover, immediate reconstruction with local pedicled flaps or microsurgical flaps is not always possible, maximizing the postoperative functional impairment [15]. Although minor maxillectomy defects can be easily repaired by means of a combined surgical and prosthetic rehabilitation, major maxillectomy defects often need a challenging implant-prosthetic rehabilitation. Indeed, major maxillectomy leads to the complete loss of alveolar bone and hard palate with a consequent severe loss of support to the facial soft tissues such as the lip, check, and nose. Moreover, in most cases surgery is associated to postoperative radiotherapy that always causes an adjunctive impairment of the elastic properties of the aforementioned anatomical facial structures [15].
The fabrication of a maxillary obturator is especially challenging in presence of a large maxillary defect. While the obturator is essential for restoring facial contour, functional mastication, articulation, and speech intelligibility, its creation could be actually impossible in wide maxillary defects. The closure of the defect depends on a pressure-resistant seal of the obturator bulb and a prosthetic design that uses all the nearest remaining anatomical structures to obtain a satisfactory stability and retention. In such case of wide bone defects, the obturator prosthesis cannot rely on any anatomical support. Dental implants positioning represents an optimal option to create a new anatomical support to the obturator prosthesis.
Conventional dental implants are the most common option to treat a patient with small and medium-sized defects of the upper jaw: in presence of a well-represented alveolar bone crest, conventional Endo-osseous implants can allow in most cases a stable support to the obturator prosthesis.[16,17,18] In all those patients that, after a subtotal maxillectomy, similar to our case, cannot be immediately reconstructed with a microsurgical revascularized bone flap, the zygoma implants represent the only available option to obtain a stable support for an obturator prosthesis. The design of zygoma implants allows the surgeons to insert these implants even in case of total maxillary bone defect because they obtain a bicortical stability through the malar bone. [19,20,21]. Moreover, zygoma implants are commonly placed at a 30-60 degree angle relative to the occlusal plane [21] in order to minimize the large lever arm and, although no implant fractures have been reported to date, to avoid any possible postoperative mechanical deficit. In presence of a severe maxillary atrophy or a wide maxillary defect, a ‘‘quad’’ approach 1 or 2 zygoma implants in the posterior maxilla and 1 or more conventional implants in the anterior maxilla is nowadays considered as the best option. A ‘‘quad’’ approach based on just 4 zygoma implants inserted in the posterior maxilla has been also described as a viable option [19,22-24].
Hexa-Zygomatic Implants in bilateral maxillectomy defect reconstruction is a new concept. In 2010, Miyamoto and colleagues describe the biomechanical aspect in maxillary prostheses with zygomatic implants, stress was dispersed around the zygomatic bone on the affected side, and stress distribution to the orbital cavity was confirmed [25]. This suggests that occlusal force affects the orbital cavity. The maximum stress was 2 MPa, suggesting that the effects of occlusal forces on the orbital cavity are minimal and that placement of implants in zygomatic bone on the affected side is feasible for dispersion of occlusal forces [25,26]. The above study by Miyamoto.et.al was carried out in cases with atrophic maxilla. This leaves us with another conundrum as there are no studies in the literature that validate the use of Hexa-Zygomatic implants in the type of bilateral maxillectomy defects.
Placing of three or two zygomatic implants on each side requires an adequate antero-posterior length of zygomatic bone to achieve the correct inclination for the distribution of forces. The reconstructive surgeon should take an anatomy guided approach to arrive at the conclusion whether placement of three or two zygomatic implants on each side is feasible on a case-to-case basis. In the present case, based on the FEA, the authors assume that four well-positioned zygomatic implants could get stability equivalent to six zygomatic implants. The authors also state that during simulation both the Hexa-zygomatic and Quad-zygomatic Implants concept were prone to the similar stresses and displacement on loading. As the use of Quad Zygomatic implants have a long track record in maxillectomy defects due to cancer ablative surgeries, so we must keep in mind that this a reliable and irrefutable option for such cases with a lot of evidence-based research backing the intervention. This is the reason that the authors have found it necessary to weigh the pros and cons of both concepts with no prior bias. The merits of Quad Zygomatic Implants concept in bilateral maxillectomy defects are that they are economical, require less operating time for placement, are easily available and have a long track record of success. The Hexa Zygomatic Implants concept on the other hand provides leeway in cases of failure of any of the individual implants which in case of Quad Zygomatic Implant would require re-insertion of a fresh implant. Keeping this in mind, the Hexa Zygomatic Implants concept will require placement of two additional implants adding to the cost and an increase in the operating time. Considering these factors, the authors pose a question that if the operating surgeons planning is sound and if the placement is accurate and fail-safe is there a requirement to place those two additional implants in extension to Quad Zygoma Concept when the data shows the longevity of both treatment concepts are similar.
The biomechanical evaluation of both the interventions have given similar values on simulation. There was a non-significant difference in the values of Von- Misses stresses, Displacement and Factor of safety for both concepts. Thus, our study supports that the use of Quad zygomatic implants is viable option in our particular patient base negating the use of additional implants which seemingly provide no added benefits and infact increase the monetary strain on the patients. Weighing all the factors from a clinical standpoint the authors believe that the quad zygomatic implant concept gives a cost-effective treatment modality for patients with bilateral maxillectomy defects which is the crux of our analysis.
5. Conclusion
Finite element analysis (FEA) has proved a useful tool to investigate the distribution of stresses around the implants. Although limited data are available on the long-term performance of zygoma implants, the literature provides evidence that such implants, associated or not to conventional implants, represent a viable and adaptable option to rehabilitate low maxillectomy defects.
The authors believe that placement of Hexa and Quad zygomatic implants are both viable reconstructive options in patients with subtotal maxillectomy defects. The final decision should be made on a case specific basis by assessing the available antero-posterior length and width of the zygomatic bone so as to say the surgeon must opt for an anatomy guided approach.
In the case in question based on the patients’ anatomy and the results of FEA simulation the authors find that it would have been possible to place ‘Quad’ or ‘Hexa’ zygomatic implants. With this in mind, we advocate the use of quad zygomatic implant system in patients with low maxillectomy defects because of the following:
- They have longer life and greater bite force and stress in the area.
- It is a cost-effective treatment modality with a smaller number of implants and its attendant complications.
The authors declare no conflict of interest for this study.
References
- Davison SP, Sherris DA, Meland NB. An algorithm for maxillectomy defect reconstruction. Laryngoscope 108(1998): 215
- Sakuraba M, Kimata Y, Ota Y, et al. Simple maxillary reconstruction using free tissue transfer and prostheses. Plast Reconstr Surg 111(2003): 594.
- Kornblith AB, Zlotolow IM, Gooen J, et al. Quality of life of maxillectomy patients using an obturator prosthesis. Head Neck 18(1996): 323.
- Brown JS. Deep circumflex iliac artery free flap with internal oblique muscle as a new method of immediate reconstruction of maxillectomy defect. Head Neck 18(1996): 412.
- Cordeiro PG, Santamaria E. A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg 105(2000): 2331.
- Prithviraj DR, Vashisht R, Bhalla HK, et al. A review of management options for rehabilitation of posterior atrophic maxilla with implants. J Dent Implants 13(2013):35–41.
- Becktor JP, Isaksson S, Abrahamsson P, et al. Evaluation of 31 zygomatic implants and 74 regular dental implants used in 16 patients for prosthetic reconstruction of the atrophic maxilla with cross-arch fixed bridges. Clin Implant Dent Relat Res 7(2005):159–65.
- Salinas T, Sadan A, Peterson T, et al. Zygomaticus implants: A new treatment for the edentulous maxilla. Quintessense Dent Technol 24(2001): 171.
- Urgell JP, Gutiérrez VR, Escoda CG. Rehabilitation of atrophic maxilla: A review of 101 zygomatic implants. Med Oral Patol Oral Cir Bucal 13(2008): E363–70.
- Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants 18(2003): 902–904.
- Guerrero C, Sabogal A. Zygoma implants. Atlas of surgery and prosthetics. RIPANO, España 10(2009): 169–183
- Wang, Mingyi & Qu, Xingzhou & Cao, et al. Biomechanical three-dimensional finite element analysis of prostheses retained with/without zygoma implants in maxillectomy patients. Journal of biomechanics 25(2013): 46.
- Geng JP, Tan KB, Liu GR. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent 85(6) (2001): 585-98.
- Cinzia Zannoni, Raffaella Mantovani, Marco Viceconti. Material properties assignment to finite element models of bone structures: a new method, Medical Engineering & Physics, Volume 20(10) (1999): 00081-2.
- Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol 11(2010): 1001Y1008.
- Baqain ZH, Anabtawi M, Karaky AA, et al. Morbidity from anterior iliac crest bone harvesting for secondary alveolar bone grafting: an outcome assessment study. J Oral Maxillofac Surg 67(2009): 570Y575.
- Chiapasco M, Biglioli F, Autelitano L, et al. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin Oral Implants Res 17(2006): 220Y228.
- Shirota T, Shimodaira O, Matsui Y, et al. Zygoma implant-supported prosthetic rehabilitation of a patient with a maxillary defect. Int J Oral Maxillofac Surg 40(2011): 113Y117.
- Malevez C, Abarca M, Durdu F, et al. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 months follow-up study. Clin Oral Implants Res 15 (2004): 18Y22.
- Branemark PI, Adell R, Albrektsson T, et al. An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. J Oral Maxillofac Surg 42(1984): 497Y505.
- Schmidt BL, Pogrel MA, Young CW, et al. Reconstruction of extensive maxillary defects using zygomaticus implants. J Oral Maxillofac Surg 62(2004): 82Y89.
- Bedrossian E, Stumpel L 3rd, Beckely ML, et al. The zygomatic implant: preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants 17(2002): 861Y865.
- Bedrossian E, Stumpel LJ 3rd. Immediate stabilization at stage II of zygomatic implants: rationale and technique. J Prosthet Dent 86(2001): 10Y14.
- Vrielinck L, Politis C, Schepers S, et al. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int J Oral Maxillofac Surg 32(2003): 7Y14.
- Miyamoto K, Ujigawa Y, Kizu M, Tonogi G-Y Yamane. Biomechanical threedimensional finite-element analysis of maxillary prostheses with implants. Design of number and position of implants for maxillary prostheses after hemimaxillectomy. Int J Oral Maxillofac Surg 39(2010): 1120–1126
- Freedman M, Ring M, Stassen LF. Effect of alveolar bone support on zygomatic implants: a finite element analysis study. Int J Oral Maxillofac Surg 42(5) (2013): 671–676.



 Impact Factor: * 3.6
Impact Factor: * 3.6 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 