Early versus Late Ureteral Stent Removal in Kidney Transplantation: A Systematic Review and Meta- Analysis of Urological Outcomes
Maher Aldemerdash1*, Ali Hussain AlShaqaq2, Abdulnaser AlAbadi1, Fahad E AlOtaibe1, Khalid Bel'eed-Akkari1, Yousef Saleh Alsowayan3
1Multi-Organ Transplant Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia
2Department of Nephrology, Johns Hopkins Aramco Healthcare Dhahran, Saudi Arabia
3Department of Urology, King Fahad Specialist Hospital, Dammam, Saudi Arabia
*Corresponding author:Maher Aldemerdash, Multi-Organ Transplant Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia.
Received: July 11, 2025;Accepted: July 28, 2025;Published: August 08, 2025
Article Information
Citation: Maher Aldemerdash, Ali Hussain AlShaqaq, Abdulnaser AlAbadi, Fahad E AlOtaibe, Khalid Bel'eed-Akkari, Yousef Saleh Alsowayan. Early versus Late Ureteral Stent Removal in Kidney Transplantation: A Systematic Review and Meta- Analysis of Urological Outcomes. Archives of Nephrology and Urology. 8 (2025): 94-105.
DOI: 10.26502/anu.2644-2833102
View / Download Pdf Share at FacebookAbstract
Background: The optimal timing for ureteral stent removal following kidney transplantation remains controversial. This meta-analysis aimed to compare outcomes between early and late stent removal.
Methods: A systematic search was conducted in PubMed, Web of Science, Cochrane Library, and Scopus databases up to July 2024 to identify studies comparing early (within 3 weeks) versus late removal of ureteral stents in kidney transplant recipients. The primary outcomes assessed were the incidence of urinary tract infections (UTIs) and ureteric leakage. Data synthesis and meta-analysis were performed using RevMan Software version 5.4.
Results: Fourteen studies comprising 3096 patients were included. Early stent removal was associated with a significantly lower incidence of UTIs compared to late removal (Odds ratio (OR) 0.46, 95% confidence interval 1 0.32-0.66, P<0.0001). This benefit was observed across different early removal time intervals. However, very early removal (within the first week) was associated with a higher risk of ureteric leakage (OR 4.71, 95% CI 1.65-13.44, P=0.004). No significant differences were found between groups for other urological complications.
Conclusion: Early ureteral stent removal, particularly within 1-3 weeks post-transplant, significantly reduces UTI risk without increasing other urological complications. However, removal within the first week posttransplant may increase the risk of ureteric leakage. These findings suggest that adopting protocols for stent removal between 1-3 weeks posttransplant could be beneficial for suitable patients, balancing the reduced risk of UTIs against the potential for early urological complications. Future prospective studies with longer follow-up are needed to further optimize stent management in kidney transplantation.
Keywords
Kidney transplantation; Ureteral stent; and Urinary tract infection; Ureteric leak
Kidney transplantation articles; Ureteral stent articles; and Urinary tract infection articles; Ureteric leak articles.
Article Details
Introduction
Kidney transplantation is a life-saving procedure for patients with end- stage renal disease, offering improved quality of life and longevity compared to dialysis [2, 3]. As surgical techniques and immunosuppressive regimens have advanced, the success rates of kidney transplants have significantly improved over the past decades [4]. However, post-transplant complications remain a concern, with urological complications being among the most common [5].
One of the key strategies to prevent urological complications, particularly ureteral obstruction and urinary leakage, is the placement of a ureteral stent during transplantation [6]. This small tube, typically made of flexible plastic, is inserted to maintain patency of the ureter and facilitate urinary drainage from the transplanted kidney to the bladder [6]. While ureteral stenting has become a standard practice in many transplant centers, there is ongoing debate regarding the optimal timing for stent removal [7]. The use of ureteral stents in kidney transplantation is associated with both benefits and potential risks [6]. On one hand, stents can reduce the incidence of major urological complications such as ureteral stenosis and leakage, which can lead to graft dysfunction or loss if left untreated [7]. On the other hand, prolonged stent placement may increase the risk of urinary tract infections (UTIs), hematuria, bladder irritation, and stent migration or encrustation [8].
Given these considerations, the timing of stent removal becomes a critical decision in post-transplant care. Traditionally, many centers have adopted a conservative approach, leaving the stent in place for several weeks to months after transplantation [1]. This practice aims to ensure complete healing of the ureterovesical anastomosis before stent removal [6]. However, recent studies have suggested that earlier stent removal may be equally effective in preventing urological complications while potentially reducing stent- related morbidity [9, 10].
The concept of early stent removal, typically defined as removal within 3 weeks post-transplantation, has gained attention in recent years. Proponents argue that early removal can decrease the risk of stent-related UTIs, reduce patient discomfort, and simplify post-transplant management [7, 9, 10]. Additionally, early removal may lead to cost savings by reducing the need for additional procedures and antibiotic treatments [11]. However, concerns persist about whether early removal might compromise the protective effects of stenting against major urological complications. Despite the importance of this issue, there is a lack of consensus in the transplant community regarding the optimal timing for ureteral stent removal. Various studies have reported conflicting results, with some favoring early removal and others supporting a more conservative approach [12-14]. This lack of agreement highlights the need for a comprehensive analysis of the available evidence to guide clinical decision- making.
The primary objectives of this systematic review and meta-analysis are to compare the incidence of urological complications, UTIs, and other stent-related morbidities between early and late ureteral stent removal groups.
Methods
In this meta-analysis, the Cochrane Handbook for Systematic Reviews and Interventions [15] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards were meticulously followed [16].
Study Selection and Data Sources
A systematic search was conducted in PubMed, Web of Science, Cochrane Library, and Scopus databases up to July 2024. The search strategy aimed to identify studies comparing outcomes of early versus late removal of ureteral stents following kidney transplantation. Detailed search strategy is shown in appendix 1.
Inclusion Criteria
Studies eligible for inclusion were randomized controlled trials (RCTs), prospective and retrospective comparative studies that evaluated outcomes such as UTI, ureteric leakage, ureteral stenosis, hydronephrosis, urinoma, and stent migration in adult patients undergoing kidney transplantation. Studies reporting comparative data on early (defined as within the first few weeks’ post-transplant) versus late (after several weeks post-transplant) removal of ureteral stents were included.
Data Extraction
Data were extracted independently by two reviewers using a standardized data extraction form. Extracted data included study design, timing of stent removal (early vs. late), study groups, sample size, participant demographics (age, sex), follow-up duration, and summary of the studies.
Quality Assessment
The quality of the included studies was assessed using different tools based on the study design. For RCTs, the revised Cochrane risk-of-bias tool (RoB 2) was used, evaluating domains such as randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selection of the reported result [17]. For cohort studies, the Newcastle-Ottawa Scale (NOS) was used, assessing selection, comparability, and outcome domains. Studies were classified as having low, moderate, or high risk of bias [18].
Data Synthesis and Analysis
Meta-analysis was conducted using RevMan software 5.4 version. Pooled odds ratios (OR) with 95% confidence intervals were calculated for dichotomous outcomes. Statistical heterogeneity was assessed using the p value of heterogeneity below 0.1 considered indicative of substantial heterogeneity. Random effect model and sensitivity analyses were performed to explore sources of heterogeneity.
Subgroup analysis
Subgroup analyses categorized studies based on specific time intervals for early versus late stent removal (e.g., within the first week, second week, or third week post- transplantation). This approach aimed to evaluate whether the observed effects on outcomes such as UTIs, ureteric leakage, and other complications varied depending on the precise timing of stent removal.
Results
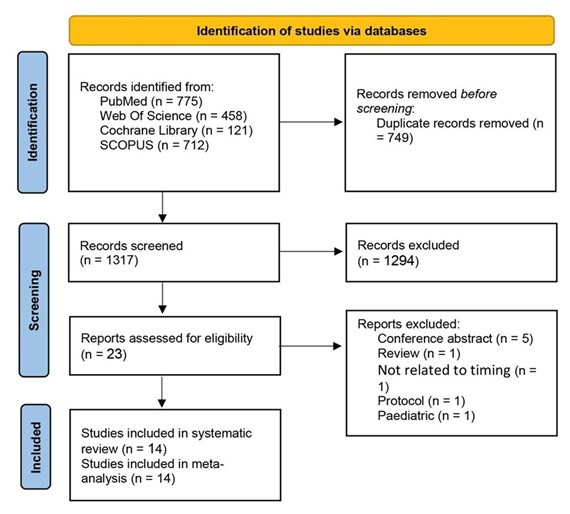
The study selection process involved an initial identification of 2066 records from PubMed, Web of Science, Cochrane Library, and Scopus. After removing 749 duplicates, 1317 records underwent title and abstract screening, resulting in the exclusion of 1294 records. Full-text screening of 23 remaining articles led to the exclusion of 9 studies, primarily due to their nature as conference abstracts, reviews, or being unrelated to the study's focus. Ultimately, 14 studies were included in the systematic review, with all 14 also included in the subsequent meta-analysis [1, 11-14, 19-27].
Baseline and summary of the included studies
In this review, there are 8 RCTs [11, 12, 14, 19, 21-24] and 6 other study designs, including retrospective [1, 13, 20, 26] and prospective comparative studies [25, 27]. Participants' ages ranged broadly across studies, ranged between 30.8 and 45.6 years; male participants were predominant across most groups. Follow-up periods ranged from one month to nine months, with the majority of studies conducting follow- ups at three months post-transplantation to assess urological outcomes and complications. Further details are shown in table 1.
Quality assessment
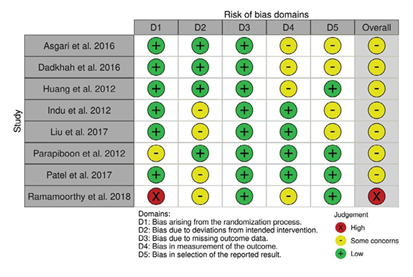
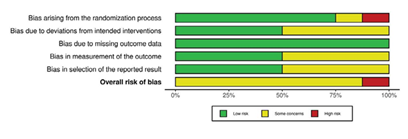
Regarding the included RCTS, 7 studies were judged as having some concerns due to lack of information about deviations from intended intervention, bias in the measurement of the outcome, or selection of the reported results. Ramamoorthy et al. 2018 was judged as having high risk of bias as it was non randomized study. Figure 2 and Figure 3
Table 1: Summary and baseline of the included studies.
Table 2: Quality assessment of the included observational studies.
|
Study ID |
Selection |
Comparability |
Outcome |
Overall |
|
Arabi et al. 2021 |
*** |
** |
*** |
Good |
|
Coskun et al. 2011 |
** |
** |
Poor |
|
|
Sarier et al. 2017 |
**** |
** |
*** |
Good |
|
Soylu et al. 2018 |
*** |
** |
*** |
Good |
|
Wingate et al. 2017 |
**** |
* |
*** |
Good |
|
Yuksel et al. 2017 |
*** |
* |
*** |
Fair |
Regarding the included observational studies, 4 studies were rated as having good quality [1, 20, 25, 26], and Yuksel et al. 2017 was judged as having fair quality [27].
On the other hand, Coskun et al. 2011 was judged as having poor quality due to insufficient data the three main domains [13].
Outcomes
Primary outcomes
Incidence of urinary tract infection (UTI)
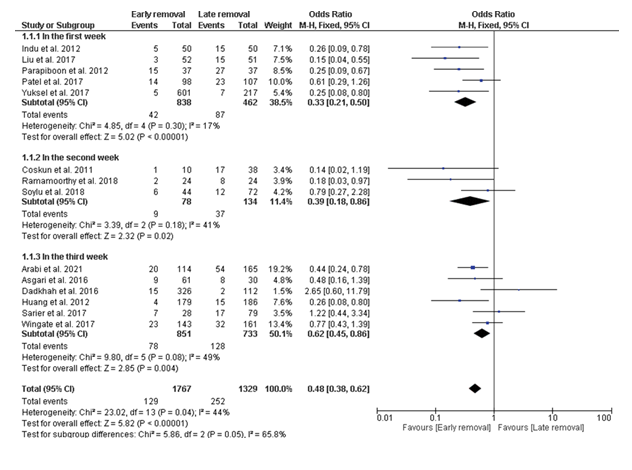
When ureteral stents were removed within the first week post-transplantation, the early removal group demonstrated a reduced incidence of UTIs compared to the late removal group (OR = 0.33 [0.21, 0.50], P < 0.00001), and the data were homogenous (P = 0.30; I² = 17%).
Similarly, when stents were removed within the second week post-transplantation, the early removal group demonstrated a reduced incidence of UTIs compared to the late removal group (OR = 0.39 [0.18, 0.86], P = 0.02), and the data were homogenous (P = 0.18; I² = 41%). When stents were removed within the third week post-transplantation, there was insignificant difference between the early removal group and the late removal group in the incidence of UTIs (OR = 0.65 [0.39, 1.08], P = 0.004), but the data were heterogeneous (P = 0.08; I² = 49%). This heterogeneity was resolved by excluding Dadkhah et al. 2016 (P = 0.20; I² = 33%). After resolving heterogeneity, the early removal group demonstrated a reduced incidence of UTIs compared to the late removal group (OR = 0.57 [0.37, 0.89], P = 0.01).
Overall, the pooled analysis of 14 studies including 3096 patients, showed a significant reduction in the incidence of UTI in the early group compared with the late group (OR = 0.46 [0.32, 0.66], P < 0.0001), but the date were heterogeneous (P = 0.04; I² = 44%). After resolving heterogeneity by excluding Dadkhah et al. 2016 (P = 0.12; I² = 33%), the results remained significant (OR = 0.43 [0.31, 0.60], P < 0.00001).
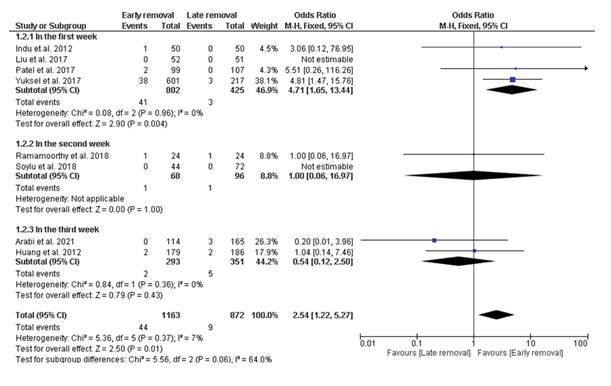
Ureteric Leakage
When ureteral stents were removed within the first week post-transplantation, the early removal group demonstrated a high incidence of ureteric leakage compared to the late removal group (OR = 4.71 [1.65, 13.44], P = 0.004), and the data were homogenous (P = 0.96; I² = 0).
When stents were removed within the third week post- transplantation, there was insignificant difference between the early removal group and the late removal group in the incidence of ureteric leakage (OR = 0.54 [0.12, 2.50], P = 0.43), and the data were homogenous (P = 0.36; I² = 0).
Overall, the pooled analysis of 8 studies including 2035 patients, showed a significant increase in the incidence of ureteric leakage in the early group compared with the late group (OR = 2.54 [1.22, 5.27], P = 0.01), and the date were homogenous (P = 0.37; I² = 7%).
Secondary outcomes
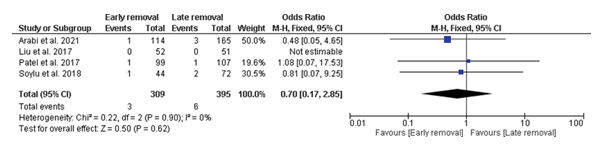
Ureteral Stenosis
There was insignificant difference between the early removal group and the late removal group in the incidence of ureteral stenosis (OR = 0.70 [0.17, 2.85], P = 0.62), and the data were homogenous (P = 0.90; I² = 0).
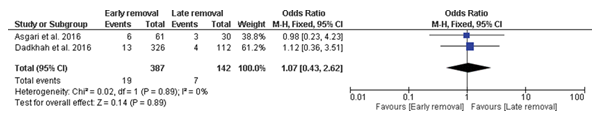
Hydronephrosis
Also, there was insignificant difference between the early removal group and the late removal group in the incidence of ureteral stenosis (OR = 1.07 [0.43, 2.62], P = 0.89), and the data were homogenous (P = 0.89; I² = 0).
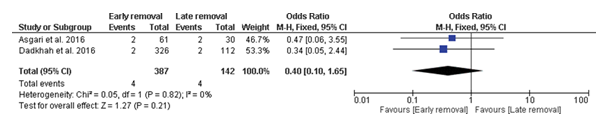
Urinoma
Similarly, there was insignificant difference between the early removal group and the late removal group in the incidence of ureteral stenosis (OR = 0.40 [0.10, 1.65], P = 0.21), and the data were homogenous (P = 0.82; I² = 0).
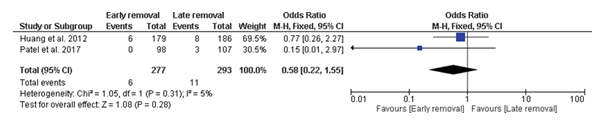
Stent migration
Finally, there was insignificant difference between the early removal group and the late removal group in the incidence of stent migration (OR = 0.58 [0.22, 1.55], P = 0.28), and the data were homogenous (P = 0.31; I² = 5%).
Discussion
Our meta-analysis provides compelling evidence that early removal of ureteral stents following kidney transplantation is associated with a significantly reduced incidence of UTIs compared to late removal. This effect was consistent across different time intervals for early removal, with the most pronounced benefit observed when stents were removed within the first week post-transplantation. The reduced UTI risk with early stent removal may be attributed to several factors. Firstly, the presence of a foreign body in the urinary tract for an extended period provides a surface for bacterial colonization and biofilm formation, increasing infection risk [28]. Early removal eliminates this nidus for infection. Secondly, prolonged stent placement can cause local irritation and inflammation of the urinary tract, potentially compromising its natural defense mechanisms against pathogens [20].
However, our analysis also revealed a higher incidence of ureteric leakage associated with very early stent removal (within the first week). This finding suggests that while early removal confers benefits in terms of UTI prevention, it may compromise the initial healing and sealing of the ureterovesical anastomosis [1]. The optimal timing for stent removal likely involves balancing these competing risks.
Moreover, our analysis found no significant differences between early and late stent removal groups in terms of other urological complications such as ureteral stenosis, hydronephrosis, urinoma formation, and stent migration. This suggests that early stent removal does not compromise the overall structural integrity of the urinary tract reconstruction, provided it is not done too early. The heterogeneity observed in some of our analyses, particularly for UTI incidence when stents were removed in the third week, highlights the complexity of this clinical decision. Factors such as surgical technique, patient characteristics, and post-operative care protocols may influence outcomes and contribute to the observed variability between studies.
Our results align closely with Wang et al. (2022) and Cai et al. (2018), showing a similar magnitude of UTI risk reduction [9, 10]. Specifically, we found an overall odds ratio of 0.46 for UTI incidence with early removal, comparable to the relative risks of 0.42 and 0.43 reported by Wang et al. and Cai et al., respectively. However, our study provides additional granularity by stratifying early removal timing, revealing benefits even within the first week post-transplantation.
Regarding major urological complications, our findings are consistent with all three studies in showing no significant differences between early and late removal groups for most complications. This includes ureteral stenosis, hydronephrosis, and urinoma formation. However, our analysis revealed an increased risk of ureteric leakage with very early (within one week) stent removal, a nuance not captured in these previous meta-analyses. This finding adds an important consideration to the risk-benefit analysis of early stent removal.
Our study's larger sample size (3096 patients) and inclusion of both randomized and observational studies may provide a more comprehensive picture than Cai et al. (2018) [10], which included only RCTs, or Visser et al. (2019) [7], which included conference abstracts. This broader inclusion criteria allows for a more real-world representation of outcomes across various clinical settings. Additionally, our subgroup analysis based on specific time intervals for stent removal offers more detailed guidance for clinical decision- making compared to the broader categorizations used in previous meta-analyses.
The results of our meta-analysis have important implications for post-transplant urological management. The clear reduction in UTI risk with early stent removal, particularly after the first week, suggests that many transplant centers could safely adopt earlier removal protocols. This could lead to reduced antibiotic use, shorter hospital stays, and improved patient comfort [29,11].
However, the increased risk of ureteric leakage with very early removal underscores the need for careful patient selection and close monitoring if adopting a very early removal strategy. It may be prudent to reserve removal within the first week for low-risk patients with optimal surgical outcomes. The lack of significant differences in other urological complications between early and late removal groups is reassuring. It suggests that concerns about increased rates of strictures or other long-term complications with early removal may be overstated, provided removal is not done too early. A key strength of our study is its comprehensive nature, including a large number of patients from diverse clinical settings. The stratification of early removal timing provides more granular insights than previous meta-analyses. Additionally, our rigorous methodology, including thorough quality assessment of included studies and careful handling of heterogeneity, enhances the reliability of our findings.
However, several limitations should be acknowledged. First, the included studies varied in their definitions of "early" and "late" removal, which could introduce some imprecision in our pooled estimates. Second, the retrospective nature of some included studies may introduce bias. Third, we were unable to account for factors such as surgical technique, immunosuppression regimens, and patient comorbidities, which could influence outcomes. Finally, the follow-up periods in most studies were relatively short, limiting our ability to assess long-term complications.
Conclusion
In conclusion, our meta-analysis supports the practice of early ureteral stent removal following kidney transplantation, particularly within the second- or third-week post-transplant. This approach appears to significantly reduce the risk of UTIs without increasing other urological complications. However, very early removal (within the first week) should be approached cautiously due to the increased risk of ureteric leakage. We recommend that transplant centers consider adopting protocols for stent removal between 1-3 weeks post-transplant for suitable patients, while maintaining close follow-up. Future prospective studies with longer follow-up periods and standardized removal time points would further refine our understanding of optimal stent management in kidney transplantation.
Acknowledgements
The authors declare no acknowledgements and received no specific funding for this work.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Trial registration: Not applicable.
References
- Soylu L, Aydin OU, Atli M, et al. Does Early Removal of Double J Stents Reduce Urinary Infection in Living Donor Renal Transplantation? Arch Med Sci 15 (2019): 402-407.
- Abecassis M, Bartlett ST, Collins AJ, et al. Kidney Transplantation as Primary Therapy for End-Stage Renal Disease: A National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQITM) Conference. Clin J Am Soc Nephrol 3 (2008): 471-480.
- Yoo KD, Kim CT, Kim MH, et al. Superior Outcomes of Kidney Transplantation Compared With Dialysis: An Optimal Matched Analysis of a National Population- Based Cohort Study Between 2005 and 2008 in Korea. Medicine (Baltimore) 95 (2016): e4352.
- Pilch NA, Bowman LJ, Taber DJ. Immunosuppression Trends in Solid Organ Transplantation: The Future of Individualization, Monitoring, and Management. Pharmacotherapy 41 (2021): 119-131.
- Choate HR, Mihalko LA, Choate BT. Urologic Complications in Renal Transplants. Transl Androl Urol 8 (2019): 141-147.
- Laftavi MR, Chaudhry Q, Kohli R, et al. The Role of Ureteral Stents for All Ureteroneocystostomies in Kidney Transplants. Int J Organ Transplant Med 2 (2011): 66-74.
- Visser IJ, van der Staaij JPT, Muthusamy A, et al. Timing of Ureteric Stent Removal and Occurrence of Urological Complications After Kidney Transplantation: A Systematic Review and Meta-Analysis. J Clin Med 8 (2019): 689.
- Geavlete P, Georgescu D, Multescu R, et al. Ureteral Stent Complications - Experience on 50,000 Procedures. J Med Life 14 (2021): 769-775.
- Wang Y, Yang Y, Zhang H, et al. Early Removal of Ureteral Stent After Kidney Transplant Could Decrease Incidence of Urinary Tract Infection: A Systematic Review and Meta-Analysis. Exp Clin Transplant 20 (2022): 28-34.
- Cai JF, Wang W, Hao W, et al. Meta-Analysis of Early Versus Late Ureteric Stent Removal After Kidney Transplantation. Transplant Proc 50 (2018): 3411-3415.
- Parapiboon W, Ingsathit A, Disthabanchong S, et al. Impact of Early Ureteric Stent Removal and Cost-Benefit Analysis in Kidney Transplant Recipients: Results of a Randomized Controlled Study. Transplant Proc 44 (2012): 737-739.
- Dadkhah F, Yari H, Ali Asgari M, et al. Benefits and Complications of Removing Ureteral Stent Based on the Elapsed Time After Renal Transplantation Surgery. Nephrourol Mon 8 (2016): e31108.
- Coskun AK, Harlak A, Ozer T, et al. Is Removal of the Stent at the End of 2 Weeks Helpful to Reduce Infectious or Urologic Complications After Renal Transplantation? Transplant Proc 43 (2011): 813-815.
- Ali Asgari M, Dadkhah F, Tara SA, et al. Early Stent Removal After Kidney Transplantation: Is It Possible? Nephrourol Mon 8 (2016): e30598.
- Cumpston M, Li T, Page MJ, et al. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10 (2019):
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. J Clin Epidemiol 62 (2009): e1-34.
- Sterne JAC, Savovic J, Page MJ, et RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 366 (2019): l4898.
- Wells GA, Shea B, O’Connell D, et The Newcastle– Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. The Ottawa Hospital Research Institute (2025).
- Appiya Ramamoorthy B, Javangula Venkata Surya P, Darlington D. Early Versus Delayed Double J Stent Removal in Deceased Donor Renal Transplant Recipients: A Prospective Comparative Study. Cureus 10 (2018):
- Arabi Z, Al Thiab K, Altheaby A, et The Impact of Timing of Stent Removal on the Incidence of UTI, Recurrence, Symptomatology, Resistance, and Hospitalization in Renal Transplant Recipients. J Transplant 2021 (2021): 3428260.
- Huang L, Wang X, Ma Y, et A Comparative Study of 3-Week and 6-Week Duration of Double-J Stent Placement in Renal Transplant Recipients. Urol Int 89 (2012): 89-92.
- Indu KN, Lakshminarayana G, Anil M, et al. Is Early Removal of Prophylactic Ureteric Stents Beneficial in Live Donor Renal Transplantation?. Indian J Nephrol 22 (2012): 275-279.
- Liu S, Luo G, Sun B, et al. Early Removal of Double-J Stents Decreases Urinary Tract Infections in Living Donor Renal Transplantation: A Prospective, Randomized Clinical Trial. Transplant Proc 49 (2017): 297-302.
- Patel P, Rebollo-Mesa I, Ryan E, et al. Prophylactic Ureteric Stents in Renal Transplant Recipients: A Multicenter Randomized Controlled Trial of Early Versus Late Removal. Am J Transplant 17 (2017): 2129-2138.
- Sarier M, Demir M, Duman I, et Evaluation of Ureteral Stent Colonization in Live-Donor Renal Transplant Recipients. Transplant Proc 49 (2017): 415-419.
- Wingate JT, Brandenberger J, Weiss A, et al. Ureteral Stent Duration and the Risk of BK Polyomavirus Viremia or Bacteriuria After Kidney Transplantation. Transpl Infect Dis 19 (2017): e12644.
- Yuksel Y, Tekin S, Yuksel D, et Optimal Timing for Removal of the Double-J Stent After Kidney Transplantation. Transplant Proc 49 (2017): 523-527.
- Samir M, Mahmoud MA, Tawfick A. Does Bacterial Colonization Influence Ureteral Stent-Associated Morbidity? A Prospective Study. Arab J Urol 21 (2023): 156-161.
- Park J, Lee SY, Lee HS, et The Impact of Prophylactic Ureteral Stenting During Kidney Transplantation on Postoperative Surgical Outcomes. Korean J Transplant 35 (2021): 41-47.
Related PubMed Articles
- Early Removal of Ureteral Stent After Kidney Transplant Could Decrease Incidence of Urinary Tract Infection: A Systematic Review and Meta-Analysis.
- Early versus late ureteric stent removal after kidney transplantation.
- Outcomes of Early Simultaneous Removal of Ureteric Stent With Indwelling Urethral Catheter After Kidney Transplant in Pediatric Recipients: A 10-Year Review.
- Timing of Ureteric Stent Removal and Occurrence of Urological Complications after Kidney Transplantation: A Systematic Review and Meta-Analysis.
- [Benefits and risks of early versus late ureteric stent removal after kidney transplantation].
- Early versus late ureteric stent removal after kidney transplantation.
- Early double J stent removal in renal transplant patients to prevent urinary tract infection - systematic review and meta-analysis of randomized controlled trials.
Article Views: 500
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
© 2016-2025, Copyrights Fortune Journals. All Rights Reserved!