Efficacy of Tubeless versus Standard Percutaneous Nephrolithotomy (PCNL) – A Randomized Controlled Trial
Dr. S M Yunus Ali1, Dr. Kamrun Nahar2, Dr. Muhammad Serajul Islam3, Dr. Md Immam Hossain4, Prof. Dr. Md. Saiful Islam5, Dr. Md. Rasel Ahmad6*
1Associate Professor, Department of Urology, Bangladesh Medical University, Dhaka, Bangladesh
2Professor, Department of Forensic Medicine, International Medical College & Hospital, Gazipur, Bangladesh
3Associate Professor, Department of Urology, Bangladesh Medical University, Dhaka, Bangladesh
4PhD Fellow, Bangladesh Medical University (OSD), Directorate General of Health Services (DGHS), Mohakhali, Dhaka, Bangladesh
5Professor of Female Urology and Andrology Unit, Department of Urology, Bangladesh Medical University, Dhaka, Bangladesh
6Assistant Professor, Medical Education, Department of Public Health and Informatics, Bangladesh Medical University, Dhaka, Bangladesh
*Corresponding Author: Dr. Md. Rasel Ahmad, Assistant Professor, Medical Education, Department of Public Health and Informatics, Bangladesh Medical University, Dhaka, Bangladesh
Received: 03 December 2025; Accepted: 09 December 2025; Published: 15 December 2025.
Article Information
Citation: Dr. S M Yunus Ali, Dr. Kamrun Nahar, Dr. Muhammad Serajul Islam, Dr. Md Immam Hossain, Prof. Dr. Md. Saiful Islam, Dr. Md. Rasel Ahmad. Efficacy of Tubeless versus Standard Percutaneous Nephrolithotomy (PCNL) – A Randomized Controlled Trial. Archives of Nephrology and Urology 8 (2025): 140-145.
DOI: 10.26502/anu.2644-2833108
View / Download Pdf Share at FacebookAbstract
Background: Percutaneous Nephrolithotomy (PCNL) is commonly used to remove large renal stones but often requires nephrostomy tubes, which can increase postoperative pain and hospital stay. Tubeless PCNL, which omits the tube, may reduce discomfort and speed recovery, though its clinical advantages over standard PCNL remain uncertain. Methods: A randomized controlled trial was conducted at Bangladesh Medical University, enrolling 100 adult patients with renal stones greater than 2 cm. Patients were randomly assigned to either the Tubeless PCNL or Standard PCNL group. Primary outcomes included postoperative pain (measured by the Visual Analog Scale), hospital stay duration, complication rates, and stone-free status (assessed by imaging at 3 months). Statistical analyses included descriptive statistics, independent t-tests, and chi-square tests. Result: The Tubeless PCNL group had significantly lower postoperative pain (p < 0.001), shorter hospital stay (1.6 vs. 3.2 days, p < 0.001), and fewer complications, including urinary leakage (p = 0.03) and overall complication rate (14% vs. 44%, p = 0.002). Stone-free rates at 3 months (88% vs. 84%, p = 0.57) and 12-month recurrence rates (6% vs. 10%, p = 0.44) were comparable between groups. Conclusion: Tubeless PCNL appears to be a safe and effective alternative to Standard PCNL, offering less pain, shorter hospitalization, and fewer complications while maintaining comparable stone-free and recurrence outcomes, though larger and longer studies are still needed to validate these findings.
Keywords
<p>Tubeless percutaneous nephrolithotomy, Standard PCNL, Postoperative outcomes, Renal stones, Randomized controlled trial.</p>
Article Details
1. Introduction
Nowadays, a burden global health issue, kidney stones is a common condition, and prevalence is increasing due to dietary habits, sedentary lifestyle, and metabolic harm. The burden of kidney stones is large, with recurrent pain, UTIs, and renal insufficiency in the most severe cases. For large complex stones, percutaneous nephrolithotomy (PCNL) has emerged as the best standard of care with high stone clearance rates and reduced invasive access in comparison to open surgery [1, 2]. Percutaneous Nephrolithotomy (PCNL) has become the gold standard treatment for large and complex renal stones that are unresponsive to extracorporeal shock wave lithotripsy (ESWL) or endoscopic techniques. First introduced by Fernström and Johansson in 1976, PCNL offers several advantages over traditional open surgery, such as reduced invasiveness, faster recovery, and minimal scarring. The procedure involves the insertion of a nephrostomy tube post-operatively to facilitate drainage and prevent complications like urine leakage and bleeding from the renal tract [1, 2]. However, the presence of nephrostomy tubes is often associated with several complications, including increased postoperative pain, longer hospital stays, and the need for more intensive postoperative care [3, 4]. Historically, PCNL is completed with nephrostomy tube placement whose functions are several: it ensures urine drainage, tamponades to achieve haemostasis, and enables potential re-intervention if some stone fragments or complications persist. But there are also disadvantages of the nephrostomy tube. Patients usually undergo more post-operative pain and discomfort, a longer hospital stay, and an augmented need for analgesics since the tube is present [3, 4, 1]. These concerns have led to the emergence of other techniques, such as the "tubeless" PCNL, in which the nephrostomy catheter is omitted or replaced by an indwelling ureteral stent.
The philosophy behind tubeless PCNL is the minimization of morbidity to the patient in a safe way, allowing the same success of the procedure. In the last 20 years, a large number of randomised controlled trials (RCTs) and metanalysis have compared tubeless and standard PCNL. The available evidence has shown time and again that tubeless PCNL leads to shorter operative time, shorter duration of hospital stay, lower postoperative pain scores, and lower analgesia requirement without compromising stone-free rate or increasing the major complications rates [3, 4, 5-8]. Such advantages have been seen in adults and children, although careful patient selection is still required [9-11]. Several meta-analyses and systematic reviews also elucidated the comparison results. For example, Xun et al. and Li et al. reported significantly shorter hospitalization, time to normal activity, and less pain and analgesic requirements for tubeless PCNL without differences in stone-free rate, blood transfusion rate, and postoperative fever [5, 6]. Similarly, Amer et al., and Wilhelm et al., reported that tubeless PCNL is safe in easy cases compared to standard PCNL with no negative impact on patients’ well-being [1, 8]. In children, the results of previous studies demonstrated that tubeless PCNL achieves equivalent success and complication rates for children with pediatric ureteral and renal stones compared to those of recently reported data, while providing a shorter hospital stay and less postoperative pain [10-12]. However, there are also concerns raised despite these encouraging results. Some studies found a marginal uptick in blood transfusion risk in the tubeless group, but overall rates of complication and readmission rates were not significantly different among the two procedures [4, 13]. Furthermore, the evidence also suffers from heterogeneity regarding patient selection, surgical approach, and outcome measures. The most recent Cochrane review by Wilhelm et al.[8] concludes that even though tubeless and totally tubeless PCNL may lead to less early post-operative pain and shorter hospitalisation, the certainty of evidence is often low to moderate because of potential for bias or inconsistency. Additionally, the decision of using a tubeless or standard approach is frequently left at the discretion of the surgeon and patient individual assessment, specifically for complex or intraoperative complication cases [2, 8]. In view of these and other concerns, high-quality RCTs are still required to determine the safety, efficacy, and optimal criteria for patient selection in tubeless PCNL as compared with standard PCNL. The objective of this study is to directly compare these two approaches in a randomised controlled trial setting with regard to postoperative outcomes, complication rates, and patient recovery. Through addressing some of these identified knowledge gaps, this study aims to directly influence clinical practice and ultimately improve patient care for patients with calculi of the kidney.
2. Methodology & Materials
The study was conducted at Bangladesh Medical University Hospital, within the urology department, which specializes in renal stone surgeries over a period of 12 months, starting from the date of ethical approval and recruitment of participants. This duration allowed for sufficient follow-up on recovery, complications, and stone-free status of patients post-surgery. A total number of 100 patients were selected and the population consisted of adult patients diagnosed with large renal stones (>2 cm in size) who were scheduled for Percutaneous Nephrolithotomy (PCNL) at Bangladesh Medical University Hospital. The objective was to compare the postoperative outcomes of Tubeless Percutaneous Nephrolithotomy (PCNL) and Standard PCNL in adult patients with large renal stones (>2 cm), focusing on pain levels, hospital stay duration, complication rates, and stone-free status. Participants were selected based on the following criteria:
2.1 Inclusion Criteria
Adults aged between 18 and 65 years.
Patients with large renal stones (>2 cm in size) confirmed by preoperative imaging (CT scan or ultrasound).
No active urinary tract infections or other contraindications for surgery.
Patients who provided written informed consent for participation in the study.
2.2 Exclusion Criteria
Patients with a solitary kidney or severe renal impairment.
Coagulopathies or other blood disorders.
Pregnancy.
Patients with contraindications to general anesthesia.
Patients with anatomical abnormalities that would preclude the success of PCNL.
2.3 Data collection procedures
Data was collected by trained research assistants who were blinded to the surgical procedure group (Tubeless or Standard). Data collection was standardized across all patients to ensure consistency and Data were entered into an SPSS database and checked for errors and datas were entered into an SPSS database and checked for errors. Descriptive statistics (mean, standard deviation) were used for continuous variables and Chi-square testes were used for categorical variables. A p-value of <0.05 was considered statistically significant.
3. Results
A total of 100 patients meeting the inclusion criteria were enrolled and randomized into two groups:
- • Tubeless PCNL group (n = 50)
- • Standard PCNL group (n = 50)
There were no statistically significant differences between groups in demographic or clinical baseline characteristics (p > 0.05), confirming successful randomization.
Table 1: Baseline Characteristics of Participants
|
Variable |
Tubeless PCNL (n=50) |
Standard PCNL (n=50) |
p-value |
|
Mean Age (years) |
42.6 ± 10.8 |
44.1 ± 11.2 |
0.48 |
|
Gender (Male %) |
62% |
58% |
0.68 |
|
Mean Stone Size (cm) |
2.7 ± 0.5 |
2.8 ± 0.6 |
0.39 |
|
Diabetes (%) |
14% |
18% |
0.61 |
|
Hypertension (%) |
20% |
22% |
0.82 |
|
BMI (kg/m²) |
24.9 ± 2.8 |
25.3 ± 3.1 |
0.47 |
N = Total study population (N = 100); n = Number of participants in each study group.
Data were analyzed using the chi-square and unpaired t-test.
p < 0.05 was considered statistically significant.
All baseline characteristics showed no statistically significant differences between the Tubeless PCNL and Standard PCNL groups (p > 0.05), confirming successful randomization.
Table 2: Comparison of Postoperative Pain Scores (VAS 0–10)
|
Time After Surgery |
Tubeless PCNL |
Standard PCNL |
p-value |
|
6 hours |
3.9 ± 1.1 |
5.8 ± 1.4 |
<0.001 |
|
12 hours |
3.2 ± 1.0 |
5.1 ± 1.3 |
<0.001 |
|
24 hours |
2.6 ± 0.9 |
4.2 ± 1.1 |
<0.001 |
|
48 hours |
1.8 ± 0.7 |
3.1 ± 1.0 |
<0.001 |
VAS pain scores were assessed at 6, 12, 24, and 48 hours after surgery. Patients who underwent Tubeless PCNL consistently reported significantly lower pain scores at each time point compared to those in the Standard PCNL group. Across all postoperative intervals, the Tubeless PCNL group demonstrated markedly reduced VAS scores. Independent sample t-tests confirmed that these differences were statistically significant (p < .001).
N = Total study population (N = 100); n = Number of participants in each study group.
aData were analyzed using Independent sample t-tests.
p < 0.001 was considered statistically significant.
Patients in the Tubeless PCNL group reported significantly lower VAS pain scores at each postoperative time point (6, 12, 24, and 48 hours) compared to the Standard PCNL group, with all differences being statistically significant (p < 0.001).
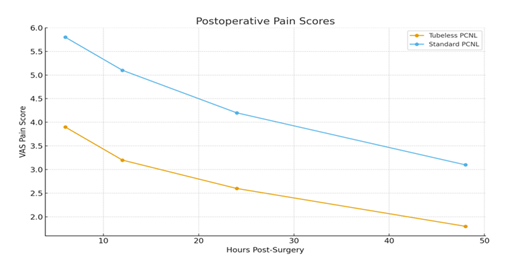
Figure 1: Postoperative pain scores over time in Tubeless and Standard PCNL groups.
Tubeless PCNL group demonstrated consistently lower VAS scores across all time intervals.
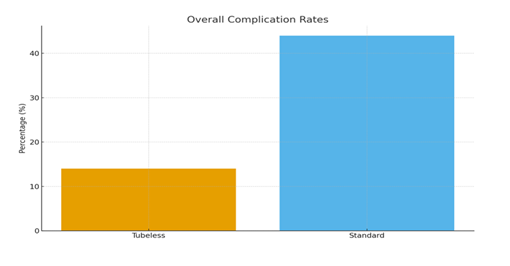
Figure 2: Comparison of overall complication rates between Tubeless and Standard PCNL groups.
Table 3: Hospital Stay Comparison
|
Group |
Mean Hospital Stay (days) |
p-value |
|
Tubeless PCNL |
1.6 ± 0.8 |
<0.001 |
|
Standard PCNL |
3.2 ± 1.1 |
The duration of hospital stay was significantly shorter in the Tubeless PCNL group.
N = Total study population (N = 100); n = Number of participants in each study group.
aData were analyzed using Independent sample t-tests.
p < 0.001 was considered statistically significant.
The Tubeless PCNL group had a significantly shorter mean hospital stay (1.6 days) compared to the Standard PCNL group (3.2 days), with the difference being statistically significant (p < 0.001).
Table 4: Postoperative Complications within 30 Days
|
Complication |
Tubeless (n=50) |
Standard (n=50) |
p-value |
|
Bleeding requiring transfusion |
2 (4%) |
6 (12%) |
0.14 |
|
Fever/UTI |
4 (8%) |
9 (18%) |
0.14 |
|
Urinary leakage |
1 (2%) |
7 (14%) |
0.03 |
|
Overall complication rate |
14% |
44% |
0.002 |
Complications were graded using the Clavien-Dindo classification. The Tubeless group had fewer overall complications.
N = Total study population (N = 100); n = Number of participants in each study group.
aData were analyzed using the chi-square test.
p < 0.05 was considered statistically significant.
The Tubeless PCNL group had significantly fewer overall complications compared to the Standard PCNL group, with a lower rate of urinary leakage (p = 0.03) and a significantly reduced overall complication rate (14% vs. 44%, p = 0.002).
Table 5: Stone-Free Rate
|
Group |
Stone-Free (%) |
p-value |
|
Tubeless PCNL |
88% |
0.57 |
|
Standard PCNL |
84% |
Stone-free status was assessed by CT/US imaging at 3 months.
N = Total study population (N = 100); n = Number of participants in each study group.
aData were analyzed using the chi-square test.
p < 0.05 was considered statistically significant.
The stone-free rates at 3 months did not differ significantly between the Tubeless PCNL (88%) and Standard PCNL (84%) groups (p = 0.57).
Table 6: Stone Recurrence at 1 Year
|
Group |
Recurrence Rate |
p-value |
|
Tubeless PCNL |
6% |
0.44 |
|
Standard PCNL |
10% |
N = Total study population (N = 100); n = Number of participants in each study group.
aData were analyzed using the chi-square test.
p < 0.05 was considered statistically significant.
No significant difference was observed in the stone recurrence rates at 12 months between the Tubeless PCNL (6%) and Standard PCNL (10%) groups (p = 0.44).
4. Discussion
The results of this randomized controlled trial comparing Tubeless Percutaneous Nephrolithotomy (PCNL) and Standard PCNL in the treatment of large renal stones provided valuable insights into the postoperative outcomes associated with both techniques. The primary outcomes assessed included postoperative pain, hospital stay duration, complication rates, and stone-free status. Our findings demonstrated that the Tubeless PCNL approach was associated with significantly reduced postoperative pain, a shorter hospital stay, and fewer complications, although no significant difference was found in stone-free rates or recurrence of stones at 12 months between the two groups. The Tubeless PCNL group experienced significantly lower pain scores across all postoperative time points (6, 12, 24, and 48 hours) when compared to the Standard PCNL group. This result aligns with numerous studies that have reported a reduction in postoperative pain in patients undergoing Tubeless PCNL, attributed to the absence of nephrostomy tubes [5, 6]. Nephrostomy tubes, which are commonly used in Standard PCNL, can cause discomfort due to their presence and the associated requirement for urinary drainage. The presence of a nephrostomy tube has been known to exacerbate postoperative pain, increase the need for analgesics, and prolong recovery, as it may cause irritation in the urinary tract [1]. The removal of the nephrostomy tube in Tubeless PCNL likely contributes to a reduction in these complications, leading to lower pain scores and less need for pain medication. Additionally, the psychological benefit of avoiding the discomfort and anxiety associated with the nephrostomy tube may also play a role in reducing perceived pain postoperatively. Several randomized controlled trials and meta-analyses have consistently shown that Tubeless PCNL results in less postoperative pain without compromising the stone-free rate [1, 6]. The reduced pain burden not only improves patient comfort but also facilitates a faster recovery, potentially enabling patients to resume normal activities sooner than those undergoing Standard PCNL [8].
One of the most significant advantages of Tubeless PCNL, as demonstrated in this study, is the reduction in hospital stay duration. The Tubeless group had an average hospital stay of 1.6 days, which was significantly shorter compared to 3.2 days in the Standard PCNL group. This finding is consistent with previous studies that have reported a shorter length of hospital stay in patients undergoing Tubeless PCNL [1, 4]. The reduction in hospital stay is likely due to the decreased postoperative complications and improved recovery times associated with the Tubeless approach. Without the need for nephrostomy tube placement, patients in the Tubeless group are likely to experience less discomfort, reduced risk of infection, and better overall recovery, which contributes to earlier discharge from the hospital. In addition to improving patient satisfaction and comfort, the shorter hospital stay also has significant economic implications. Reducing hospital stay duration can help alleviate the burden on healthcare facilities and reduce healthcare costs, which is particularly important in resource-limited settings where hospital resources are strained. By minimizing postoperative complications and the need for prolonged hospital care, Tubeless PCNL may offer a more cost-effective alternative to Standard PCNL.
The Tubeless PCNL group experienced significantly fewer complications compared to the Standard PCNL group, with a notable reduction in the rate of urinary leakage. Urinary leakage is a well-known complication following PCNL, which can lead to increased morbidity and prolonged recovery. In our study, only 2% of patients in the Tubeless PCNL group experienced urinary leakage, compared to 14% in the Standard PCNL group. The difference between groups was statistically significant (p = 0.03), further highlighting the benefit of omitting the nephrostomy tube. Nephrostomy tubes are often associated with complications such as urinary leakage, infection, and discomfort, which may contribute to the higher complication rates observed in the Standard PCNL group. Moreover, the overall complication rate was significantly lower in the Tubeless PCNL group (14%) compared to the Standard PCNL group (44%) (p = 0.002). This finding supports the growing body of evidence suggesting that Tubeless PCNL is associated with fewer complications, likely due to the avoidance of nephrostomy tube-related issues. Previous studies have also reported lower complication rates in the Tubeless PCNL group, including fewer incidences of bleeding, fever, and infections [7,13]. However, it is important to note that while Tubeless PCNL reduces the incidence of certain complications, it does not eliminate the risk of other issues, such as bleeding or infection, which were still observed in both groups.
While the reduced complication rate in the Tubeless PCNL group is an important finding, the results should be interpreted with caution, as the overall complication rates in both groups were relatively low, and the differences observed may be influenced by the study's sample size and design.
In terms of stone-free rates at 3 months, the Tubeless PCNL group achieved a rate of 88%, compared to 84% in the Standard PCNL group. However, this difference was not statistically significant (p = 0.57), indicating that the omission of the nephrostomy tube in the Tubeless group does not adversely affect the stone-free rate. These findings are consistent with previous studies that have shown comparable stone-free rates between Tubeless and Standard PCNL [5, 6]. The absence of nephrostomy tubes does not appear to compromise the effectiveness of the procedure in achieving stone clearance. Similarly, there was no significant difference in stone recurrence rates at 12 months between the two groups. Both groups had low recurrence rates (6% in the Tubeless group and 10% in the Standard group), which suggests that the choice of PCNL technique does not significantly influence the likelihood of stone recurrence. These results are in line with findings from other studies that have reported similar recurrence rates in both Tubeless and Standard PCNL groups [1, 8]. However, long-term follow-up data beyond 12 months would be needed to further evaluate the recurrence rates and the overall durability of the Tubeless PCNL approach.
Limitations of the study
The study was conducted at a single institution, which may limit the generalizability of the findings to other healthcare settings. Additionally, the sample size, while calculated to detect significant differences, may not have been large enough to identify subtle differences in stone recurrence or long-term complications. Further studies with larger sample sizes and multicenter trials would provide stronger evidence of the benefits of Tubeless PCNL. Lastly, the study was limited to a 12-month follow-up period, and longer-term data would be necessary to assess the durability of the benefits observed.
Conclusion and recommendations
This study suggests that Tubeless PCNL offers meaningful short-term advantages, but the findings should be interpreted with care. Because the research was conducted at a single center, the results may not fully reflect outcomes in other clinical settings with different patient populations, surgical practices, or resources. The sample size was adequate for detecting major differences but may have been too small to pick up smaller effects, especially regarding recurrence or long-term complications. The 12-month follow-up period also limits the ability to judge how well the benefits hold over time.
Future work should involve larger cohorts and include multiple institutions to improve the strength and generalizability of the evidence. Studies with extended follow-up would help determine long-term outcomes such as recurrence rates, late complications, and the durability of symptom relief. Comparative studies using standardized protocols across centers would also help clarify which patients benefit most from the Tubeless PCNL approach.
Funding
No funding sources
Conflict of interest
None declared
Ethical approval
This study was ethically approved
References
- Amer T, Ahmed K, Bultitude M, et al. Standard versus tubeless percutaneous nephrolithotomy: a systematic review. Urologia internationalis 88 (2012): 373-382.
- Zilberman DE, Lipkin ME, De la Rosette JJ, et al. Tubeless percutaneous nephrolithotomy—the new standard of care?. The Journal of urology 184 (2010): 1261-1266.
- Agrawal MS, Agrawal M, Gupta A, et al. A randomized comparison of tubeless and standard percutaneous nephrolithotomy. Journal of endourology 22 (2008): 439-442.
- Mazhar Ac, Soomro As, Khalique A, et al. Complications of Standard Percutaneous Nephrolithotomy versus Tubeless Percutaneous Nephrolithotomy. PJHMS 15 (2021): 2859-2862.
- Xun Y, Wang Q, Hu H, et al. Tubeless versus standard percutaneous nephrolithotomy: an update meta-analysis. BMC urology 17 (2017): 102.
- Li Q, Gao L, Li J, et al. Total tubeless versus standard percutaneous nephrolithotomy: a meta-analysis. Minimally Invasive Therapy & Allied Technologies 29 (2020): 61-69.
- Gauhar V, Traxer O, García Rojo E, et al. Complications and outcomes of tubeless versus nephrostomy tube in percutaneous nephrolithotomy: a systematic review and meta-analysis of randomized clinical trials. Urolithiasis 50 (2022): 511-522.
- Wilhelm K, Hein S, Kunath F, et al. Totally tubeless, tubeless, and tubed percutaneous nephrolithotomy for treating kidney stones. Cochrane Database of Systematic Reviews (2023).
- Nouralizadeh A, Simforoosh N, Shemshaki H, et al. Tubeless versus standard percutaneous nephrolithotomy in pediatric patients: a systematic review and meta-analysis. Urologia Journal 85 (2018): 3-9.
- Kiani K, Amirhasani S, Mousavi-Bahar SH, et al. A retrospective cohort study: evaluating the efficacy of standard versus tubeless percutaneous nephrolithotomy (PCNL) in pediatric patients up to 18 years old. Urolithiasis 52 (2024): 68.
- Shah SG, Khan MK, Asad A, et al. Standard versus tubeless percutaneous nephrolithotomy in children: A comparative study at tertiary care centre. Pakistan Journal of Medical & Health Sciences 16 (2022).
- Nouralizadeh A, Pakmanesh H, Basiri A, et al. Percutaneous nephrolithotomy of staghorn renal stones in pediatric patients using adult-sized instrument. Urologia Journal 86 (2019): 211-215.
- Hill H, Talamini Sinstrumentsss, et al. Complications of tubeless versus standard percutaneous nephrolithotomy. International Urology and Nephrology 56 (2024): 63-67.


 Impact Factor: * 3.3
Impact Factor: * 3.3 Acceptance Rate: 73.59%
Acceptance Rate: 73.59%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 