The Role of Restage Transurethral Resection of Urinary Bladder Tumor in Patients with High-Risk Non- Muscle Invasive Bladder Cancer-Our Experience in Mugda Medical College Hospital, Dhaka, Bangladesh
Mohammod Mamunur Rashid1, Muhammad Mahmud Alam2, Md. Mahmud Hasan3, Khondaker Arafuzzaman4, Shariful Islam Khan5, Mohammad Al Amin6, KM Arifur Rahman7, Md. Akter Alam8
1Associate Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
2Associate Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
3Associate Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
4Assistant Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
5Senior Consultant, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
6Assistant Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
7Assistant Registrar, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
8Assistant Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
*Corresponding Author: Mohammod Mamunur Rashid, Associate Professor, Department of Urology, Mugda Medical College & Hospital, Dhaka, Bangladesh
Received: 10 October 2025; Accepted: 21 October 2025; Published: 14 November 2025
Article Information
Citation: Mohammod Mamunur Rashid, Muhammad Mahmud Alam, Mahmud Hasan, Khondaker Arafuzzaman, Shariful Islam Khan, Mohammad Al Amin, Arifur Rahman KM, Md. Akter Alam. The Role of Restage Transurethral Resection of Urinary Bladder Tumor in Patients with High-Risk Non- Muscle Invasive Bladder Cancer-Our Experience in Mugda Medical College Hospital, Dhaka, Bangladesh. Archives of Nephrology and Urology. 8 (2025): 113-117.
DOI: 10.26502/anu.2644-2833104
View / Download Pdf Share at FacebookAbstract
Background: Transurethral resection of bladder tumor (TURBT) is the cornerstone for diagnosis and initial management of non-muscle invasive bladder cancer (NMIBC). However, in high-risk NMIBC, a significant proportion of patients harbor residual tumor or are under-staged following initial TURBT. Restage TURBT (re-TURBT) has been recommended to improve diagnostic accuracy and oncological outcomes.
Objective: To evaluate the role of re-TURBT in high-risk NMIBC patients and to share our institutional experience at Mugda Medical College Hospital.
Methods: This prospective observational study included 100 patients with high-risk NMIBC (Ta high-grade, T1, and/or carcinoma in situ) treated between January 2020 and December 2024. All patients underwent initial complete TURBT, followed by re-TURBT within 2–6 weeks. Residual tumor detection rate, tumor upstaging, recurrence, and complications were analyzed.
Results: Among 100 patients, 62% had residual tumor detected on re- TURBT. Tumor upstaging to muscle-invasive disease occurred in 14%. Residual tumor was most common in T1 high-grade lesions (71%). Re- TURBT led to change in management plan in 28% of cases (early radical cystectomy or intensified intravesical therapy). Perioperative morbidity was minimal, with no major complications.
Conclusion: Re-TURBT significantly improves staging accuracy and therapeutic planning in high-risk NMIBC. Our study supports the routine use of re-TURBT as a standard of care in high-risk cases to optimize longterm oncological outcomes.
Keywords
<p>TURBT; NMIBC; Tumor.</p>
Article Details
1. Introduction
Bladder cancer is the tenth most common malignancy worldwide, accounting for significant morbidity and mortality [1]. At initial diagnosis, nearly 70–75% of cases are classified as non-muscle invasive bladder cancer (NMIBC), confined to the mucosa (stage Ta, carcinoma in situ) or submucosa (stage T1) [2]. Among these, patients with high-risk NMIBC characterized by high-grade T1 lesions, carcinoma in situ, or large/multiple/recurrent tumors—pose a considerable management challenge due to high recurrence rates (up to 70%) and progression to muscle-invasive disease in 20–30% of cases [3,4]. Transurethral resection of bladder tumor (TURBT) remains the cornerstone of diagnosis and initial management of NMIBC [5]. It provides tissue for histopathological assessment and determines crucial prognostic factors such as grade, stage, and presence of detrusor muscle [6]. However, despite being the standard of care, initial TURBT is often incomplete due to technical limitations, large tumor size, multifocality, or surgeon experience [7]. Consequently, residual tumor is detected in a significant proportion of cases, ranging from 30% to 70%, with upstaging reported in up to 25% [8,9]. Restaging TURBT, usually performed within 2–6 weeks of the initial resection, has therefore been recommended in selected patients, particularly those with high-grade T1 tumors, incomplete resection, or absence of detrusor muscle in the specimen [10]. Evidence suggests that repeat TURBT improves the accuracy of staging, identifies residual disease, reduces recurrence, enhances response to adjuvant intravesical Bacillus Calmette–Guérin (BCG), and improves progression-free survival [11]. Consequently, both the European Association of Urology (EAU) and American Urological Association (AUA) guidelines strongly recommend restaging TURBT in patients with high-risk NMIBC [12]. Despite these recommendations, restaging TURBT is not universally practiced, particularly in resource-limited settings, due to constraints in infrastructure, patient compliance, and clinical workload [13]. Evaluating its role in different clinical environments is essential to optimize outcomes and develop context-specific management strategies. In this study, we report our institutional experience with restaging TURBT in 100 patients with high-risk NMIBC at Mugda Medical College Hospital. The aim was to assess the rate of residual disease, tumor upstaging, and overall clinical utility of restaging TURBT in improving patient management within our setting.
2. Methods
Study Design: Prospective observational study
Place & Duration: Department of Urology, Mugda Medical College Hospital, Dhaka, Bangladesh; January 2020 – December 2024.
Sample Size: 100 patients
Inclusion Criteria:
- • Age >18 years
- • Histologically confirmed high-risk NMIBC (Ta high-grade, T1, CIS) after first TURBT
- • Availability of muscle tissue in histopathology report
Exclusion Criteria:
- • Muscle-invasive disease at initial TURBT
- • Previous history of bladder cancer treatment
- • Patients unfit for repeat anesthesia
Procedure:
- • Initial complete TURBT performed with bipolar resectoscope.
- • Re-TURBT performed within 2–6 weeks by same urology team. Tumor bed, resection margins, and any suspicious areas re-resected.
- • Histopathological examination evaluated residual tumor, grade, stage, and muscle involvement.
- • Patients received intravesical BCG or chemotherapy as per guideline.
2.1 Data Analysis
All data were collected prospectively from 100 patients diagnosed with high-risk non-muscle invasive bladder cancer (NMIBC) who underwent initial transurethral resection of bladder tumor (TURBT) followed by a restage TURBT at Mugda Medical College Hospital. Data were entered into Microsoft Excel and analyzed using SPSS version 25. Continuous variables (e.g., age, tumor size) were expressed as mean ± standard deviation (SD) or median (IQR) as appropriate. Categorical variables (e.g., sex, tumor grade, stage, presence of carcinoma in situ, residual disease on restage TURBT) were summarized as frequencies and percentages.
Comparisons between groups were performed using:
- • Chi-square test (χ²) or Fisher’s exact test for categorical variables.
- • Student’s t-test / Mann-Whitney U test for continuous variables depending on normality (tested by Shapiro-Wilk test).
A p-value <0.05 was considered statistically significant.
The primary outcome was the rate of residual tumor detection at restage TURBT. Secondary outcomes included upstaging to muscle-invasive disease (≥T2), detection of additional carcinoma in situ, and tumor characteristics influencing residual disease (tumor size, multiplicity, grade, stage).
3. Results
3.1 Patient Profile
A total of 100 patients with high-risk non-muscle-invasive bladder cancer (NMIBC) were included in the study. The mean age of the cohort was 58.7 years (range: 40–78 years). There was a clear male predominance, with a male-to-female ratio of 4.5:1. The most common risk factor was cigarette smoking, reported in 61% of patients, followed by occupational exposure to bladder carcinogens in 12%.
3.2 Histopathology at Initial TURBT
On initial transurethral resection of bladder tumor (TURBT), 32 patients (32%) had Ta high-grade disease, 58 patients (58%) had T1 disease, and 10 patients (10%) had carcinoma in situ (CIS).
3.3 Findings at Restage TURBT
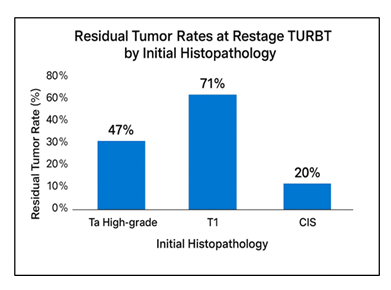
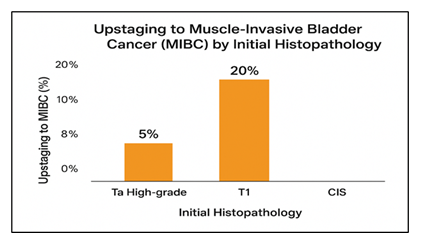
At restage TURBT, residual tumor was detected in 62 patients (62%). The residual tumor rate was highest among patients with T1 disease (71%), followed by Ta high-grade (47%) and CIS (20%). Upstaging to muscle-invasive bladder cancer (MIBC, ≥T2) was observed in 14 patients (14% of the total cohort), with the majority of upstaged cases occurring in the T1 subgroup (20%). These findings resulted in a change in management strategy in 28% of cases, leading to early radical cystectomy or initiation of intensified intravesical therapy.
Table 1: Findings at Restage TURBT in 100 Patients with High-Risk NMIBC.
|
Initial Histopathology |
Patients (n) |
Residual Tumor at re-TURBT (%) |
Upstaging to MIBC (%) |
|
Ta High-grade |
32 |
47% |
5% |
|
T1 |
58 |
71% |
20% |
|
CIS |
10 |
20% |
0% |
|
Total |
100 |
62% (overall) |
14% (overall) |
Figure 1 illustrates the residual tumor rates at restage TURBT stratified by initial histopathology. The highest residual tumor rate was observed in patients with T1 disease (71%), followed by Ta high-grade (47%) and CIS (20%).
Figure 2 shows the rate of upstaging to muscle-invasive bladder cancer (≥T2) at restage TURBT. Upstaging was most common in the T1 subgroup (20%), whereas only 5% of patients with Ta high-grade tumors were upstaged, and no upstaging was observed in patients with CIS.
3.4 Complications
Re-TURBT was generally well tolerated. Minor perioperative bleeding occurred in 8% of patients, while 15% experienced transient hematuria or irritative voiding symptoms. Importantly, there was no mortality or major morbidity reported.
4. Discussion
This prospective study of 100 patients with high-risk NMIBC highlights the pivotal role of repeat transurethral resection (re-TURBT) in improving staging accuracy, detecting residual disease, and guiding optimal management. Our results showed that 62% of patients had residual tumor on re-TURBT, and 14% were upstaged to muscle-invasive disease. Importantly, management strategy was altered in 28% of cases, reflecting the clinical significance of a second resection.
4.1 Residual Tumor Rates
The high rate of residual disease observed in our cohort (62%) is consistent with published data. Previous studies have reported residual tumor rates ranging from 33% to 78% after initial TURBT, particularly in patients with T1 disease [3,4]. In our study, residual tumor was most prevalent in T1 cases (71%), underscoring the technical difficulty of complete resection and the tendency for deeper tumor invasion in this subgroup.\
4.2 Upstaging to Muscle-Invasive Disease
Upstaging to muscle-invasive bladder cancer occurred in 14% of patients. This is comparable to international series, which report upstaging rates of 10–25% [3,6]. The highest upstaging rate was in T1 tumors (20%), highlighting the limitations of initial TURBT in accurately assessing depth of invasion. Such findings emphasize the importance of re-TURBT in avoiding under-treatment, since patients with undetected muscle-invasive disease require radical cystectomy rather than intravesical therapy alone.
4.3 Impact on Management
Re-TURBT altered the treatment plan in more than a quarter of patients in our series. This is clinically relevant, as failure to detect residual or muscle-invasive disease could delay definitive treatment and increase the risk of progression [7,10]. By identifying patients with residual or advanced disease early, re-TURBT facilitates timely initiation of appropriate therapy, such as radical cystectomy or intensified BCG treatment.
4.4 Comparison with International Guidelines
Both the European Association of Urology (EAU) and the American Urological Association (AUA) strongly recommend a second TURBT in all high-risk NMIBC cases [11-13]. Our findings align with these recommendations and reinforce the value of re-TURBT in real-world practice. In resource-limited settings like Bangladesh, patient compliance, financial constraints, and limited theatre capacity often hinder routine implementation. However, the benefits demonstrated in our study especially in reducing under-staging and recurrence risk—justify prioritizing re-TURBT for high-risk patients.
4.5 Complications and Safety
The safety profile of re-TURBT in our study was favorable. Only minor complications such as self-limiting hematuria (15%) and mild bleeding (8%) were observed. No patient experienced major morbidity or mortality. This confirms that re-TURBT is a safe procedure that can be performed without significant additional risk [14].
4.6 Clinical Implications
Our findings reaffirm that re-TURBT is not merely a confirmatory step but a critical therapeutic intervention. It ensures accurate staging, prevents under-treatment, and facilitates timely radical intervention when necessary. Given the high prevalence of residual disease and upstaging in our cohort, re-TURBT should be considered standard of care in all high-risk NMIBC patients [3,6,15].
4.7 Management Changes
Upstaging to muscle-invasive bladder cancer (≥T2) occurred in 14 patients (14%). As a result of re-TURBT, management strategy was altered in 28% of cases, leading to early radical cystectomy or intensified intravesical therapy.
4.8 Complications
Re-TURBT was generally well-tolerated. Minor perioperative bleeding occurred in 8% of patients, while 15% experienced transient hematuria or irritative voiding symptoms. Importantly, there was no mortality or major morbidity reported.
5. Conclusion
Re-TURBT is an indispensable tool in the management of high-risk NMIBC. Our experience in 100 cases demonstrates a high rate of residual tumor and clinically significant upstaging, directly impacting treatment planning. We recommend routine re-TURBT in all high-risk NMIBC patients to optimize oncological outcomes and reduce the risk of disease progression.
References
- Babjuk M, Burger M, Capoun O, et al. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer. Eur Urol 81 (2022): 75-94.
- Chang SS, Boorjian SA, Chou R, et al. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. J Urol 196 (2021): 1021-1029.
- Divrik RT, Sahin A, Yildirim Ü, et al. Impact of routine second transurethral resection on the long-term outcome of patients with newly diagnosed pT1 urothelial carcinoma. Eur Urol 58 (2010): 185-190.
- Brausi M, Collette L, Kurth K, et al. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma. Eur Urol 41 (2002): 521-523.
- Babjuk M, Burger M, Capoun O, et al. European Association of Urology Guidelines on Non–Muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ). Eur Urol 81 (2022): 75–94.
- Chang SS, Boorjian SA, Chou R, et al. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. J Urol. 206 (2021): 1117–1129.
- Divrik RT, Sahin A, Yildirim Ü, et al. Impact of routine second transurethral resection on the long-term outcome of patients with newly diagnosed pT1 urothelial carcinoma. Eur Urol 58 (2010): 185–190.
- Herr HW. The value of a second transurethral resection in evaluating patients with bladder tumors. J Urolv 162 (1999): 74–76.
- Brausi M, Collette L, Kurth K, et al. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: A combined analysis of seven EORTC studies. Eur Urol 41 (2002): 523–531.
- Sfakianos JP, Kim PH, Hakimi AA, et al. The role of repeat transurethral resection of bladder tumor in the management of non–muscle-invasive bladder cancer. Curr Urol Rep 15 (2014): 456.
- Mariappan P, Zachou A, Grigor KM. Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur Urol 57 (2010): 843–849.
- Guigui A, Basile G, Zattoni F, et al. Prognostic significance of residual tumor at restaging transurethral resection of bladder tumor. Eur Urol 42 (2024): 480.
- Alsyouf M, Konety B, Pohar K, et al. Is a restaging TURBT necessary in high-risk NMIBC if the initial resection is complete? Urol Oncol 41 (2023): 109.
- Filon M, Schmidt B. New treatment options for non-muscle-invasive bladder cancer. Am Soc Clin Oncol Educ Book 45 (2025): e471942.
- Miçooğulları U, Çakıcı MC, Özçift B, et al. The effect of second TURBT on recurrence and progression in primary Ta high-grade bladder cancers: a multicenter clinical trial comparing long-term outcomes. Urol Oncol 22 (2023): 20-27.


 Impact Factor: * 3.3
Impact Factor: * 3.3 Acceptance Rate: 73.59%
Acceptance Rate: 73.59%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 