Anesthesia for Kidney Transplantation: Our Experience. Retrospective study over a period of 12 months at EHUO
Zelmat SA*, Bouabida D, Ouadah K, Bensafir S, Boucherit A, Belcacem F, Elkebir D, Mazour F
Department of Medicine, University of Oran, Algeria
*Corresponding Author: Zelmat SA, Department of Medicine, University of Oran, Algeria
Received: 30 March 2022; Accepted: 08 April 2022; Published: 21 April 2022
Article Information
Citation: Zelmat SA, Bouabida D, Ouadah K, Bensafir S, Boucherit A, Belcacem F, Elkebir D, Mazour F. Anesthesia for Kidney Transplantation: Our Experience. Retrospective study over a period of 12 months at EHUO. Anesthesia and Critical Care 4 (2022): 84-91.
View / Download Pdf Share at FacebookAbstract
Our work is a descriptive study of patients admitted for kidney transplantation at the EHUO, with the aim of describing the protocol and specifying the severity of postoperative incidents of kidney transplantation. We conducted a descriptive study over 12 months. 76 cases of kidney transplant recipients were treated in the EHUO Anesthesia Resuscitation Department. The male/female sex ratio 33/43 is 0.77 showing a clear female predominance, with an average age of 40.61 ± 14.51 years, the age varied between 17 and 75 years for all patients. an average dry weight of 69 ± 16 kg. The average duration of surgery was 290 ± 70 minutes. All the patients benefited from a renal monograft. Our protocol is based on general anesthesia combined with spinal analgesia with morphine (in the absence of any contraindication to ALR) with the main objective of maintaining sufficient perfusion of the graft in order to prevent thrombosis of vascular anastomoses. 75 (99%) received spinal analgesia with morphine with an average bolus of 150 ± 50 ug. In the post-operative monitoring room, 1 out of 76 (1.31%) patients received morphine (titration, then PCA) with an average dose of 7 ± 7 mg. The average consumption of morphine during the first 24 hours was 17 ± 19 mg. No patient presented serious adverse effects (allergy, desaturation, bradycardia, drowsiness) attributable to the administration of morphine. 4 patients out of 76 (3.04%) patients presented at least one non-serious adverse effect (nausea, vomiting, pruritus, bradypnoea) attributable to the administration of morphine during the first 24 postoperative hours. The postoperative follow-up was simple in 66.88% of cases, the complications found: 1 case of compressive hematoma and no death.
Keywords
<p>Morphine anesthesia, Transplantation, Surgery</p>
Article Details
1. Introduction
Chronic renal failure is a progressive and irreversible decrease in the functioning of the kidneys which no longer properly filter the body's blood. The main causes are diabetes and high blood pressure. With the aging of the population, it is a disease whose incidence is increasing. At the terminal stage of the disease, renal function replacement therapy is necessary (by hemodialysis, peritoneal dialysis or renal transplantation). Currently the management of terminal CKD, kidney transplantation has a real benefit compared to dialysis in terms of improving the patient's quality of life. At EHUO, kidney transplants are from living donors. Kidney transplantation is a scheduled surgery when the transplant comes from a living donor. The surgical technique is standardized and consists of suturing the artery and the vein of the transplant on the iliac vessels of the recipient and the ureter in the bladder, through an ilioinguinal incision. Kidney transplantation from a living donor has particularities of anesthesia and resuscitation. Maintaining sufficient perfusion of the graft and preventing thrombosis of vascular anastomoses are the main objectives of the perioperative phase. The objective of this work is to describe the Protocol and to specify the severity of the incidents in postoperative renal transplantation in our surgical resuscitation anesthesia department.
2. Material and Methods
Our work is a retrospective study of a series of patients admitted to the operating room for kidney transplants at the level of the Anesthesia department- Surgical Resuscitation (ARC) of the EHUO. Over a period of 12 months, extending from January 1, 2021 to December 31, 2021. Different parameters were exploited by a pre-established operating sheet produced for this purpose, allowing the collection of epidemiological, clinical, paraclinical, therapeutic, anesthetic and evolutionary data. The objective of this work is to describe the protocol and to specify the severity of the incidents in postoperative of kidney transplantation in our ARC surgical resuscitation anesthesia department.
3. Results
During this 12-month study, 76 cases of kidney transplant recipients (donors and recipients) were treated in the EHUO ARC department. The male / female sex ratio 33/43 is 0.77 showing a clear female predominance figure 1, with an average age of 40.61 ± 14.51 years, the extremes between 17 and 75 and an average dry weight of 69 ± 16 kg
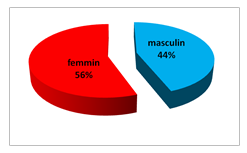
Figure 1: Distribution of patients by gender
The donor was alive within the family in 89.7%. The anesthetic technique was general anesthesia combined with spinal analgesia with morphine. The average duration of anesthesia was 6.64 h (extreme 5.8 and 7.4 h). Extubation was performed at the end of the operation (70 cases) and in resuscitation (06 cases) with an average duration of postoperative ventilation: 4.6 hours. The average warm ischemia time was 1.85h (extreme 1.6 and 2.06h) and cold ischemia 1.07h (extreme 0.9 and 1.2h). See table 1.
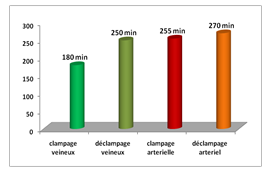
Figure 2: The average duration of the different operating times in minutes
All our patients benefited from an intraoperative filling which was guided by PVC, it was 10mL/kg/h f on average by saline and lactate ringer, albumin. Two cases were transfused with red blood cells. Perioperative stimulation of diuresis. See figure 3
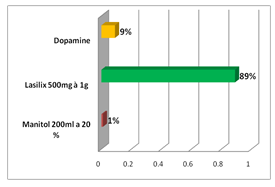
Figure 3: Stimulation of diuresis.
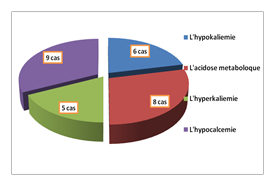
Figure 4: Distribution of patients according to metabolic disorders
Peri-operative metabolic disorders are marked by:
Hypokalemia in 6 cases
Metabolic acidosis 8cases
Lhyper kaliemie 5cas
Hypocalcemia 9 cases
(See Figure 4)
The drugs administered intraoperatively were: dopamine (21.4%), diuretics (21.4%) and antihypertensive (14.3%). Antibiotic prophylaxis consisted of a 3rd generation cephalosporin (72 cases) and adapted to carrying germs (4 cases). The time to normalization of renal function postoperatively was: day 1 (85%), day 3 (14.3%), day 6 and day 25 in the same proportion (7.1%). See figure 6
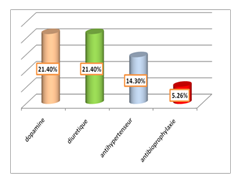
Figure 5: Breakdown of patients according to the therapeutic administered
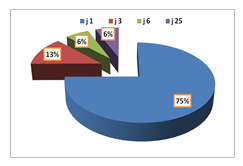
Figure 6: Distribution according to the time to normalization of renal function postoperatively
Postoperative complications were: viral pneumopathy (1 case), hyperglycaemia (2 cases), and infection of the peritoneal drainage fluid (1 case), arterial hypertension (4 cases) and favorable evolution of oligoanuria (1 case). No patient presented serious adverse effects (allergy, desaturation, bradycardia, drowsiness) attributable to the administration of morphine. (4%) patients experienced at least one non-serious adverse effect (nausea, vomiting, pruritus, bradypnea) (Figure 7)
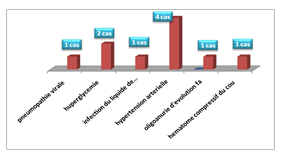
Figure 7: Breakdown by Postoperative complications
74 (98%) received spinal analgesia with morphine with an average bolus of 150 ± 50 ug. In the post-operative monitoring room, 02 patients (2%) received morphine (titration, then PCA) with an average dose of 7 ± 7 mg. The average consumption of morphine during the first 24 hours was 17 ± 19 mg. The average length of stay in the intensive care unit: 1.04 days (extremes: 0 and 6 days), that in nephrology of 01 day (extremes: 0 and 2 days). No deaths were reported. There is an association between the duration of hospitalization in intensive care and the type of intervention with a p significance of 0.198 table 2.
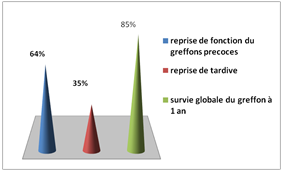
Figure 8: Distribution of patients according to graft function recovery
Anesthesia for kidney transplantation is standardized with manageable post-operative consequences in the past; the occurrence of potentially serious complications was feared by anesthetists-resuscitators. Currently, the occurrence of such complications is unlikely because well codified protocols are applied. Surgery is a very important part of therapy, it allows an improvement in the quality of life, its practice has been answered thanks to the improvements obtained in the preparation in the anesthesia and in the intraoperative monitoring. The method of anesthesia used in our series is general anesthesia, it must be associated with spinal analgesia in order to improve perioperative analgesia according to some authors [1-4]. The purpose of monitoring in intensive care is twofold: firstly to detect postoperative complications both common to all surgery and specific to kidney transplant surgery; secondly to monitor renal function. Our results are comparable to other series [5-9]. Complications are relatively infrequent in our study and no deaths were observed in our series, which testifies to the effectiveness of our protocol which is series [5-7].
4. Conclusion
The essential principles of anesthesia for kidney transplantation are to perform this intervention after preoperative preparation. The anesthetic technique of choice combines general anesthesia and spinal pain with morphine, which improves the quality.
References
- Suthanthiran M, Strom TB. Renal transplantation. N Engl J Med 331 (1994): 365-376.
- Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 23 (1999): 1725-1730.
- Klatte T, Ficarra V, Gratzke C, et al. A Literature Review of Renal Surgical Anatomy and Surgical Strategies for Partial Nephrectomy. Eur Urol 68 (2015): 980-992.
- Sampaio FJ. Renal anatomy. Endourologic considerations. Urol Clin North Am 27 (2000): 585-607.
- Graves FT. The anatomy of the intrarenal arteries and its application to segmental resection of the kidney. Br J Surg 42 (1954): 132-139.
- Leichtman AB, Cohen D, Keith D, et al. Kidney and pancreas transplantation in the United States, 1997-2006: the HRSA Breakthrough Collaboratives and the 58 DSA Challenge. Am J Transplant 8 (2008): 946-957.
- National Kidney Foundation. KDOQI Clinical Practice Guideline for Hemodialysis Adequacy: 2015 update. Am J Kidney Dis 66 (2015): 884-930.
- Meier-Kriesche HU, Ojo AO, Port FK, et al. Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J Am Soc Nephrol 12 (2001): 1293-1296.
- Abramowicz D, Cochat P, Claas FH, et al. European Renal Best Practice Guideline on kidney donor and recipient evaluation and perioperative care. Nephrol Dial Transplant 30 (2015): 1790-1797.
- Wang LW, Fahim MA, Hayen A, et al. Cardiac testing for coronary artery disease in potential kidney transplant recipients: a systematic review of test accuracy studies. Am J Kidney Dis 57 (2011): 476-487.
- Pilmore H, Dent H, Chang S, et al. Reduction in cardiovascular death after kidney transplantation. Transplantation 89 (2010): 851-857.
- Adams HP, Dawson G, Coffman TJ, et al. Stroke in renal transplant recipients. Arch Neurol 43 (1986): 113-115.
- International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms--risk of rupture and risks of surgical intervention. N Engl J Med 339 (1998): 1725-1733.
- Coleman S, Kerr H, Goldfarb D, et al. Utilization of vascular conduits to facilitate renal transplantation in patients with significant aortoiliac calcification. Urology 84 (2014): 967-970.
- McAdams-DeMarco MA, Law A, King E, et al. Frailty and mortality in kidney transplant recipients. Am J Transplant 15 (2015):149-154.
- Chapman JR, Sheil AG, Disney AP. Recurrence of cancer after renal transplantation. Transplant Proc 33 (2001): 1830-1831.
- Zlotnick DM, Axelrod DA, Chobanian MC, et al. Non-invasive detection of pulmonary hypertension prior to renal transplantation is a predictor of increased risk for early graft dysfunction. Nephrol Dial Transplant 25 (2010): 3090-3096.
- Wijdicks EF. The diagnosis of brain death. N Engl J Med 344 (2001): 1215-1221.
- Sung RS, Christensen LL, Leichtman AB, et al. Determinants of discard of expanded criteria donor kidneys: impact of biopsy and machine perfusion. Am J Transplant 8 (2008): 783-792.
- Treat EG, Miller ET, Kwan L, et al. Outcomes of shipped live donor kidney transplants compared with traditional living donor kidney transplants. Transpl Int 27 (2014): 1175-1182.
- Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, Guo H, Gross CR, Matas AJ. Long-term consequences of kidney donation. N Engl J Med 360 (2009): 459-469.
- Gill JS, Tonelli M. Understanding rare adverse outcomes following living kidney donation. JAMA 311 (2014): 577-579.
- Moers C, Smits JM, Maathuis MH, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med 360 (2009): 7-19.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 