Comparison of a Metal-Alloy Impregnated Urinary Catheter and Conventional Latex Foley Catheter for Preventing UTI in Critically Ill Trauma ICU Admitted Patients: A Prospective, Randomized Clinical Trial
Priya Singla1, Badri Prasad Das2*, Munesh Kumar Gupta3, Matendra Singh Yadav4, Sradha Choudhury3, GK Sinha2
1DR BRAIRCH, AIIMS, New Delhi, India
2Department of Anesthesiology and Critical Care, IMS BHU, Varanasi, India
3Department of Microbiology, IMS BHU, Varanasi, India
4Department of Anesthesiology, UPUMS, Saifai, India
*Corresponding Author: Badri Prasad Das, Division of Critical Care, Department of Anesthesiology and Critical Care, IMS-BHU, Varanasi, India.
Received: 15 September 2025; Accepted: 23 September 2025; Published: 06 October 2025
Article Information
Citation: Priya Singla, Badri Prasad Das, Munesh Kumar Gupta, Matendra Singh Yadav, Sradha Choudhury, GK Sinha. Comparison of a Metal-Alloy Impregnated Urinary Catheter and Conventional Latex Foley Catheter for Preventing UTI in Critically Ill Trauma ICU Admitted Patients: A Prospective, Randomized Clinical Trial. Anesthesia and Critical care 7 (2025): 98-103.
View / Download Pdf Share at FacebookAbstract
Objectives: Urinary tract infection (UTI) is the most common health-care associated infection worldwide, where the quality of Foley catheter and duration affects its occurrence. Apart from conventional Foley catheters, metal-alloy impregnated catheters (BIP Foley catheters) are also being increasingly used for urinary catheterization in ICU patients.
Material and Methods: This single-centric, prospective, single-blinded, randomized, clinical comparative study was conducted from September 2019 to August 2020 in Trauma-ICU, Department of Anesthesiology, IMS-BHU, where patients with trauma aged 18-60 years, requiring urinary catheterisation for at least 3 days, were allocated into one of the 2 study groups based on the Foley catheters used (Group A: Conventional latex Foley Catheter or Group B: BIP Foley catheter). We noted incidence of nosocomial UTI (bacterial/ fungal) in form of symptomatic CAUTI (S-CAUTI) and catheter?associated asymptomatic bacteriuria (CA?ASB) as primary outcome, while clinical outcome in form of 30-day mortality was assessed as secondary outcome. Chi-Square/ Student’s t-test were used for qualitative/ quantitative data with statistical significance at p-value ≤ 0.05.
Results: We noted comparable demographic parameters. Out of 79 analyzed patients in group A, 16 patients developed S-CAUTI as compared to 4 out of 74 analyzed patients in group B (p<0.006). Most common bacteria isolated in S-CAUTI was Escherichia coli (15.2% in group A and 4.1% in group B) followed by Enterococcus (2.5% in group A and 1.4% in group B). The relative risk reduction in group B was 48.3% as compared to group A.
Conclusion: Use of metal-alloy impregnated urinary catheter (BIP) for catheterizing critically ill patients had resulted in lower incidence of CAUTI in Trauma-ICU admitted patients, however without any significant mortality benefit.
Keywords
Symptomatic Catheter Associated Urinary Tract Infection (S-CAUTI); Catheter Associated Asymptomatic Bacteriuria (CA-ASB); Novel metal alloy Bactiguard Infection Protection (BIP) catheter; Trauma ICU
Symptomatic Catheter Associated Urinary Tract Infection (S-CAUTI) articles; Catheter Associated Asymptomatic Bacteriuria (CA-ASB) articles; Novel metal alloy Bactiguard Infection Protection (BIP) catheter articles; Trauma ICU articles
Article Details
1. Introduction
Urinary tract infection (UTI) is the most common healthcare- associated infection worldwide and accounts for almost 30–40% of all ed infections. The main causative agents for Community acquired urinary tract infections (CAUTIs) are monomicrobial, commonly caused by Escherichia coli, Enterococci, Klebsiella, and Proteus [1]. However, in ICU admitted patients, Escherichia coli, klebsiella, Pseudomonas aeruginosa, Enterococci, Candida cause UTI. Nevertheless, incidence of fungal pathogens causing UTI in Trauma ICU admitted patients too is increasing that is owing to use or misuse of antimicrobial agents, prolonged catheterization and genito-urinary manipulation in traumatic patients. In conscious patients, pain and discomfort are the usual manifestation. Moreover, CAUTIs cause additional 1-4 days hospital stay and also result in increased use of antibiotics, with consequent emergence of resistant microbial strains [2-5].
In trauma-ICU admitted patients, catheterization is done to facilitate the drainage and to observe the urine output. Conventional foley’s catheter is used widely. However, prolonged in-situ catheter promotes the colonization with subsequent UTI followed by sepsis [6]. Another type of Foley’s catheter, Bactiguard-coated Foley catheters (Bactiguard Infection Protection, BIP, Sweden) was approved for transurethral and suprapubic use for upto 90 days by the US Food and Drug Administration in 1994. This catheter has a stable noble metal alloy and hydrogel coating (also referred to as silver alloy and hydrogel−coated, SAH) on the outer- and inner-luminal surfaces of the catheter, providing repellent and anti-microbial properties, thus preventing the microbial biofilm formation. Here, the amount of noble metals at the surface is very low and there is no release of any toxic or pharmacological quantities. This makes the technology both tissue-friendly and safe.
In published literature, asymptomatic bacteriuria (ASB) alone or in combination with symptomatic UTI as the endpoint has been reported in CA-UTI prevention events. However, their clinical relevance is always questionable [6,7]. Though, there is a theoretical advantage of metal alloy coated catheters against bacterial infection (owing to antibacterial property), the incidence of fungal UTI has not been documented. Therefore, we have a prospective, interventional study to compare the CAUTI incidences in noble metal alloy Foley catheter (BIP catheter) and conventional Foley catheter in Trauma-ICU admitted patients.
2. Materials and Methods
This single-centric, prospective, single-blinded, clinical comparative interventional study was approved by Institutional Ethical Committee (Dean/2018/EC/963 dated 14/11/2018). Subsequently, the trial was also registered in clinical trial registry (CTRI/2019/09/021306). Then, this study was conducted from September 2019 to August 2020 in the Trauma Intensive care unit (ICU) of Department of Anesthesiology, IMS BHU. After obtaining written and informed consent from patients or their relative, we enrolled the patients aged 18-60 years, admitted in trauma ICU, requiring a urinary catheter for at least 3 days and using a closed drainage system. We excluded children, patients with prior UTI, known case of benign prostatic hypertrophy, urinary tract injury, urinary tract congenital abnormalities or obstetric/ gynaecological abnormalities, patients with history of diabetes and those who had urinary catheter of less than 3 days, from this study.
Using computer generated random numbers in an opaque sealed envelope, we randomized the enrolled patients were into two groups: Group A (conventional siliconized latex Foley catheters) and Group B (those who were catheterized with silver impregnated noble metal alloy BIP catheters) in a ratio of 1:1. CAUTI was clinically defined based on guidelines from the Centre for Disease Control and Prevention (CDC) - National Healthcare Safety Network criteria. Symptomatic CAUTI (S-CAUTI) was defined when the patient has, or had, a urinary catheter for 48 hours before the specimen collection with a positive urine culture of ≥103 colony forming unit/ml (cfu/ml) or ≥105 cfu/ml with no more than two organisms and at least one symptom (fever, dysuria, or suprapubic tenderness). If the patient has a positive urine culture ≥103 and <105 cfu/ml, one laboratory evidence is required (positive dipstick for leukocyte esterase and/or nitrite, pyuria, microorganism seen on Gram stain of unspun urine). The criteria for asymptomatic CAUTI (CA-ASB) was patient has, or had, a urinary catheter within 48 h before the specimen collection, a positive urine culture of ≥103cfu/ml or ≥105cfu/ml with no more than two organisms, if the patient has a positive urine culture of ≥103and <105 cfu/ml, one laboratory evidence is required (positive dipstick for leukocyte esterase and/or nitrite, pyuria, microorganism seen on Gram stain of unspun urine).
Demographic data included age, gender, and date of urinary catheter insertion, medical, and clinical data for each patient was collected. The recorded medical data included concomitant illness, such as renal tubular acidosis, pulmonary embolism, pleural effusion, status epilepticus, intracranial haemorrhage, diabetic ketoacidosis, drug overdose, and surgery (post-operative), etc. Moreover, Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment score (SOFA) scores were recorded on admission to assess the severity of illness. To reduce the risk of CAUTI, the catheters were inserted using aseptic technique and sterile equipment. The hand hygiene before and after insertion and maintenance of a closed drainage system and properly secured catheters was done. After insertion of Foleys catheter, all the branding over the catheter was obscured by sterile brown tape. Urine specimen for cultures was collected directly from the catheter or tubing either through the catheter collection port or through puncture of the tubing with a needle, to maintain a closed drainage system. All clinical data was collected both before the catheter insertion (baseline) and on the third catheterization day or earlier if fever occurred, and at every onset of fever till 30 days or earlier (when it needed to be removed due to blockage or patient died or patient was shifted to ward). Body temperature, suprapubic tenderness, costovertebral angle pain or tenderness, and UTI-related symptoms (oliguria and polyuria) monitoring was done. Clinical samples were taken whenever a patient demonstrated symptoms and signs of UTI, or as part of a sepsis workup. In addition, measured clinical parameters included white blood cells in blood and urine (pyuria) and bacterial culture in urine and blood specimen. After obtaining culture reports, escalation and de-escalation of antibiotics and anti-fungal therapy was done. For both urine culture and analysis, unspun urine samples was processed as per standard microbiological procedures.
Identification of bacteria was done by colony morphology on CLED agar and microscopic observation. Subsequently, Gram’s staining was done to categorize the organism, either gram positive, gram negative or yeast. Further identification was done by array of biochemical tests. Antibiotic susceptibility of the isolated microbes was performed by modified Kirby Bauer method and the zone of inhibition around antibiotic disc was measured and interpreted as sensitive/resistant as per CLSI guidelines.
The primary outcome of the study was to compare the incidence of CAUTI, including frequency of S-CAUTI and CA-ASB, whereas, the secondary outcomes were to assess cost effectiveness and clinical outcome in form of 30-day mortality among CAUTI diagnosed patients in both the groups.
For taking 5% alpha error and 80% power of study with a minimum difference of 30%, we needed a minimum of 128 patients. However, considering 10% attrition rate, we enrolled at least 140 patients. The recorded data were analyzed using appropriate tests using SPSS version 16.0 (SPSS Inc, Chicago, IL, USA) was used. For qualitative data and quantitative data, we used chi square and students T test, respectively. Outcome in both the groups was assessed using log rank test.
3. Results
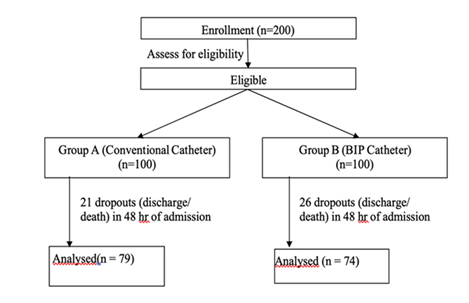
After obtaining written and informed consent, we randomized 79 patients in group A, and 74 patients in group B. The study CONSORT has been provided in Figure 1. Baseline demographics like age, sex, baseline APACHE II score, SOFA score and reason for admission were comparable in both the groups (Table 1).
|
Parameters |
Group A (n=79) |
Group B (n=74) (Mean +/- SD) |
P-value |
||
|
(Mean +/- SD) |
|||||
|
Age in years |
34.96+/-12.785 |
38.64 +/-15.365 |
0.11 |
||
|
Sex (Male/female) |
54/25 |
56/18 |
0.314 |
||
|
APACHE II |
15.15+/-5.272 |
15.51+/-5.161 |
0.669 |
||
|
SOFA |
5.38+/-2.126 |
5.15+/-1.726 |
0.463 |
||
|
Fever onset |
4.63+/-2.631 |
4.57+/-2.968 |
0.903 |
||
|
Days of ICU admission |
16.29+/-12.319 |
15.57+/-11.256 |
0.706 |
||
|
Catheter day |
14.91+/-9.324 |
14.38+/-8.251 |
0.713 |
||
|
Reason for admission |
number |
% |
number |
% |
|
|
Thoraco-abdominal trauma |
14 |
17.7 |
9 |
12.2 |
0.336 |
|
Orthopedic trauma |
25 |
31.6 |
20 |
27 |
0.53 |
|
Neuro-trauma (TBI) |
40 |
50.6 |
45 |
60.8 |
0.205 |
Table 1: Baseline demographics and characteristics.
The total sample for urine cultures sent in group A and group B were 141 and 127, respectively. The incidence of CAUTI w.r.t to total urine cultures sent was significant lower in group B as compared to group A (p=0.010) (Table 2). Out of 79 patients in group A, 16 patients developed S-CAUTI, whereas among 74 enrolled patients in group B, only 4 patients developed S-CAUTI which was significant lower (p<0.006) (Table 3). Total 7 patients in group A developed CA-ASB as compared to 2 patients in group B, which was not statistically significant (p=0.105) (Table 3). We also observed 12.75% and 12.2% incidence of candiduria in group A and group B, having no significant difference (p=0.925).
We also determined the etiology of CAUTI and observed that E. coli (15.2% in group A and 4.1% in group B) followed by Enterococcus (2.5% in group A and 1.4% in group B) were the most common cause of S-CAUTI (Table 4). E. coli (5.1% in group A and 1.4% in group B) followed by Enterococcus (2.5% in group A and 1.4% in group B) resulted in CA-ASB. We also noted 48.3% relative risk reduction in group B in comparison to group A. We also calculated the clinical outcome by determining 30-days mortality among patients with CAUTI in both the groups and observed that it was less in group B as compared to group A, but with no significant difference statistically (p value=0.807) (Table 5).
|
Total urine cultures in group A (n=141) |
Total urine cultures in group B (n=127) |
|||
|
CAUTI |
No. |
% |
No. |
% |
|
Present |
16 |
11.3 |
4 |
3.1 |
|
Absent |
125 |
88.7 |
123 |
97 |
|
Total |
141 |
100 |
127 |
100 |
(p=0.010)
Table 2: Comparison of Incidence of CAUTI w.r.t urine cultures in both groups.
|
Group |
||||
|
A |
B |
|||
|
S-CAUTI |
No. |
% |
No. |
% |
|
Present |
16 |
20.3 |
4 |
5.4 |
|
Absent |
63 |
79.7 |
70 |
94.6 |
|
Total |
79 |
100 |
74 |
100 |
|
(p=0.006) |
||||
|
CA-ASB |
No. |
% |
No. |
% |
|
Present |
7 |
8.9 |
2 |
2.7 |
|
Absent |
72 |
91.1 |
72 |
97.3 |
|
Total |
79 |
100 |
74 |
100 |
|
(p=0.105) |
||||
Table 3: Comparison of Incidence of S-CAUTI and CA-ASB w.r.t total no of patients between the two groups.
|
Group A (n=79) |
Group B (n=74) |
p-value |
|||
|
S-CAUTI |
No. |
% |
No. |
% |
|
|
Candida |
10 |
13 |
9 |
12.2 |
0.925 |
|
E. coli |
12 |
15 |
3 |
4.1 |
0.048 |
|
Enterococcus |
2 |
2.5 |
1 |
1.4 |
0.589 |
|
S.aureus |
1 |
1.3 |
0 |
0 |
0.999 |
|
Klebsiella |
1 |
1.3 |
0 |
0 |
0.999 |
|
CA-ASB |
No. |
% |
No. |
% |
|
|
E. coli |
4 |
5.1 |
1 |
1.4 |
|
|
Enterococcus |
2 |
2.5 |
1 |
1.4 |
|
|
S. aureus |
1 |
1.3 |
0 |
0 |
|
Table 4: Comparison of microbes causing CAUTI in both groups.
|
Total CAUTI in group A (n=16) |
Total CAUTI in group B (n=4) |
|||
|
No. |
% |
No. |
% |
|
|
Death |
5 |
31.3 |
1 |
25 |
|
Survived |
11 |
68.7 |
3 |
75 |
|
Total |
16 |
100 |
4 |
100 |
(p=0.807)
Table 5: Comparison of 30-days mortality among CAUTI diagnosed patients in the two groups.
We also sent blood culture in patients having CAUTI. We noted four and one blood culture positivity in group A and B, respectively without any significance difference (p=0.368). Here, one case was noted as SBUTI as the same Escherichia coli was isolated in urine as well as blood. However, in other cases, CAUTI does not resulted in secondary bacteremia and sepsis.
We also noted the number of patients who required second catheterization. In group a, 20 patients needed second catheterization, while it was nine in group B. Moreover, only 2 patients in group B, catheter was changed for third time as compared to 5 patients in group A (p=0.115). Conventional foley catheter cost around Rs 180/ catheter and cost of BIP foley catheter was Rs 1020/ catheter. Total 104 catheters were used in group A and 85 catheters were used in group B during the entire study period, which cost about Rs 18,720 and Rs 86,700 in group A and B respectively. Thus, BIP was not found to be cost effective, although a lower incidence of CAUTI rate was noted.
4. Discussion
In trauma-ICU patients, foleys catheter is placed to measure the urine output as these patients are highly vulnerable for acute renal injury as a consequence of hypovolemia. Moreover, in unconscious patients, in-site foleys catheter result in proper drainage of formed urine. However, this catheterization for more than 48hrs predispose to catheter associated urinary tract infections. Here, the microbes initially colonise the external and internal layer of the catheter with subsequently biofilm formation that result in seeding of the microbes in the urinary tract and may result in UTI. Moreover, the urethral catheter can inhibit or bypass certain defense mechanisms that would normally prevent or minimize bacteria–epithelial cell interactions. In untreated or delayed treated cases, the microbes may ascend and result in pyelonephritis and secondary blood-stream infections. Female patients having shorter urethra, unconscious patients, and fecal incontinence are the major predisposing risk-factors. However, improper hygiene practices during insertion and maintenance.
In ICU admitted patients, aseptic precautions are usually taken while insertion, however, compliance to hand hygiene is poor in developing countries. Therefore, in this condition, prevention of biofilm formation on the Foleys catheter usually remains in the focus. In comparison to conventional catheter, metal coating of BIP catheter provides repellent and anti-infective properties by preventing the formation of microbial biofilm. This coating consisting of gold, silver and palladium preserves the urethral mucosal integrity and helps to avoid the onset of inflammation. The noble metals in the Bactiguard coating cause a galvanic effect, which prevents bacteria from adhering to surface, thus, been reported to have lower biofilm-forming ability [7]. In present study, we noted lower incidence of CAUTI in patients using BIP catheter. However, there was no difference in the 30-days mortality among both the groups.
The current study is in accordance with the recent multisite cohort study by Lederer et al. [8], who reported 58% reduction in incidence of CAUTI with use of metal alloy catheter [9,10]. The incidence of CAUTIs as observed in few other studies are 1.9 − 2.4/1000 catheter-days in Polish ICUs [11,12]; 6.4 − 12/1000 catheter-days according to the SPIN-UTI Project of the Italian Nosocomial Infections Surveillance in ICUs [13] and 1.46 − 0.57/1000 catheter-days reported by the Krankenhaus Infections Surveillance System [14].
Our study is also supported by Liedberg and Lundeberg [15] who evaluated silver alloy-coated catheter in 120 patients and found that the silver alloy-coated catheter reduced the rate of catheter-associated urinary tract infections. Six patients (10%) with the silver coated catheter and 22 (37%) with the teflonised latex catheter developed bacteriuria (p<0.01). In the early 2000s, a randomised cross-over study by Karchmer et al. [16] demonstrated that the risk of UTI could be decreased by 21% on wards and by 32% among patients when a noble metal alloy catheter was used instead of a conventional catheter [16].
Escherichia coli, Enterococcus feacium, Staphylococcus aureus and klebsiella pneumoniae were the isolated uropathogens. E. coli was the most common organism in both the groups (15.2% in group A whereas 5.2% in group B). Enterococcus (2.5% in group A and 1.4% in group B) was the second most common isolated organism. This is in accordance with a study done by Santhose et al. [17], who reported E. coli (39.00%) as the predominant organism [17]. E. coli is responsible for more than 80% of the UTIs, and it causes both symptomatic UTIs and Asymptomatic bacteriuria. The persistence of E. coli strains is related to the presence of Type 1 pili, an adhesin for uroepithelium as well as the Tamm–Horsfall protein. Colonising E. coli strains lack P fimbriae in most cases of catheter-associated infections [18].
59 out of 79 patients in group A never required second catheterization during the study period as compared to 65 patients in group B who did not require re-catheterization. Although the price behind using BIP catheter was more, but because of less incidence of CAUTI rate, there was definite decrease in the antibiotic and antifungal usage. Though we did not calculate the cost benefit of antibiotic/ antifungal utilization, the usage was less.
Our study had several limitations. we could not decide whether single metal out of gold, palladium and silver or combination of three is responsible for the results obtained unless and until we study them separately. Also, we did not calculate the cost of antibiotics/antifungals usage. However, this study adds to the available literature on metal-alloy coated BIP catheter and its use can reduce the incidence of CAUTI. Moreover, there is a need for searching the exact rationale behind the reduced incidence of CAUTI in patients having in-situ BIP catheter.
5. Conclusion
Metal alloy impregnated urinary catheter (BIP catheter) for catheterization in critically ill patients admitted to Trauma ICU, can reduce the bacterial colonization and biofilm formation that eventually may result in risk reduction for symptomatic CAUTI without any added advantage.
Conflict of interest:
Nothing to disclose.
References
- Dordevic Z, Folic M, Jankovic S. Community-Acquired Urinary Tract Infections: Causative Agents and Their Resistance to Antimicrobial Drugs. Vojnosanit Pregl 73 (2016): 1109-1115.
- Schaberg DR, Weinstein RA, Stamm WE. Epidemics of Nosocomial Urinary Tract Infection Caused by Multiply Resistant Gram-Negative Bacilli: Epidemiology and Control. J Infect Dis 133 (1976): 363-366.
- Centers for Disease Control (CDC). Public Health Focus: Surveillance, Prevention, and Control of Nosocomial Infections. MMWR Morb Mortal Wkly Rep 41 (1992): 783-787.
- National Nosocomial Infections Surveillance (NNIS) System. Report, Data Summary from October 1986–April 1996. Am J Infect Control 24 (1996): 380-388.
- Haley RW, Culver DH, White JW, et al. The Nationwide Nosocomial Infection Rate: A New Need for Vital Statistics. Am J Epidemiol 121 (1985): 159-167.
- Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 50 (2010): 625-663.
- Magnusson B, Kai-Larsen Y, Granlund P, et al. Long-Term Use of Noble Metal Alloy Coated Urinary Catheters Reduces Recurrent CAUTI and Decreases Proinflammatory Markers. Ther Adv Urol 11 (2019): 1756287219857654.
- Lederer JW, Jarvis WR, Thomas L, et al. Multicenter Cohort Study to Assess the Impact of a Silver-Alloy and Hydrogel-Coated Urinary Catheter on Symptomatic Catheter-Associated Urinary Tract Infections. J Wound Ostomy Continence Nurs 41 (2014): 473-480.
- Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. Atlanta, GA: CDC; 2015. Available from: http://www.cdc.gov/nhsn/pdfs/pscmanual/psccauticurrent.pdf
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN Surveillance Definition of Health Care–Associated Infection and Criteria for Specific Types of Infections in the Acute Care Setting. Am J Infect Control 36 (2008): 309-332.
- Rutkowska K, Przybyła M, Misiołek H. Health-Care Associated Infection in the Newly-Opened Intensive Care Unit. Anaesthesiol Intensive Ther 45 (2013): 62-66.
- Wałaszek M, Wolak Z, Dobroś W. Nosocomial Infection in Patients Hospitalized in 2005–2011: The St. Lukas District Hospital in Tarnów. Przegl Epidemiol 66 (2012): 617-621.
- Agodi A, Barchitta M. Epidemiology and Control of Urinary Tract Infections in Intensive Care Patients. In: Nikibakhsh A, editor. Clinical Management of Complicated Urinary Tract Infection. InTech (2011): 1-18.
- Gastmeier P, Behnke M, Schwab F, et al. Benchmarking of Urinary Tract Infection Rates: Experiences from the Intensive Care Unit Component of the German National Nosocomial Infections Surveillance System. J Hosp Infect 78 (2011): 41-44.
- Liedberg H, Lundeberg T. Silver Alloy Coated Catheters Reduce Catheter-Associated Bacteriuria. Br J Urol 65 (1990): 379-381.
- Karchmer TB, Giannetta ET, Muto CA, et al. A Randomized Crossover Study of Silver-Coated Urinary Catheters in Hospitalized Patients. Arch Intern Med 160 (2000): 3294-3298.
- Bharathi Santhose N, Mythily N, Ashok Kumar C. Study on Biofilm Producing Bacterial Isolates in Catheter-Associated Urinary Tract Infection. IOSR J Dent Med Sci 17 (2018): 50-53.
- Koves B, Magyar A, Tenke P. Spectrum and Antibiotic Resistance of Catheter-Associated Urinary Tract Infections. GMS Infect Dis 5 (2017): 6.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 