Comparison of Video Laryngoscopy versus Direct Laryngoscopy during Elective Endotracheal Intubation at Orotta and Halibet National Referral Hospitals Asmara, Eritrea 2022
Betiel Yihdego Kidanemariam1*, Micheal Beraki Mengistu1, Biniam Rezene1, Hermon Teklebrhan Abraha1, Mustofa Abdel Bari1, Omer Osman1, Samuel Fikremariam1, Henok Afewerki Kidane2
1Orotta College of Medicine and Health Sciences, Qohayto St, Asmara, Eritrea
2The Guardian Group, History Editor and Medical Assistant, Asmara, Eritrea
*Corresponding Author: Betiel Yihdego Kidanemariam, Orotta College of Medicine and Health Sciences, Qohayto St, Asmara, Eritrea.
Received: 16 August 2025; Accepted: 22 August 2025; Published: 22 September 2025
Article Information
Citation: Betiel Yihdego Kidanemariam, Micheal Beraki Mengistu, Biniam Rezene, Hermon Teklebrhan Abraha, Mustofa Abdel Bari, Omer Osman, Samuel Fikremariam, Henok Afewerki Kidane. Comparison of Video Laryngoscopy versus Direct Laryngoscopy during Elective Endotracheal Intubation at Orotta and Halibet National Referral Hospitals Asmara, Eritrea 2022. Anesthesia and Critical care 7 (2025): 91-97.
View / Download Pdf Share at FacebookAbstract
Introduction: Airway management plays an essential role in anesthesia during elective and emergency situations. Despite the necessity of extensive training and personal skills, direct laryngoscope stays the most widely used method of intubation. Video laryngoscope provides a better visualization of the airway, ease of use and short learning curve. However, with all its advantages, Video laryngoscope was less used as routine practice.
Aim: The aim of the study was to compare C- MAC video laryngoscope and direct laryngoscope during endotracheal intubation in Orotta and Halibet National Referral Hospitals. Methods: This was an interventional comparative study conducted between November and February 2022. Patients undergoing elective surgery were randomly allocated to one of two Groups comprising of 48 patients in each as: Group I direct laryngoscope and Group II video laryngoscope. Time of intubation, hemodynamic changes, ease of intubation, oesophageal intubation, airway trauma and postoperative throat pain were assessed after patients were intubated in each group. Descriptive statistics for demographic data, Pearson’s chi-square test, Fisher’s exact test, independent samples t-test or Mann-Whitney U were computed. Factors affecting first attempt success was determined using logistic regression.
Results: The overall mean age of the patients was 48.7 (14.09). The median time of intubation under DL (Md=40 seconds, IQR=24 seconds) was significantly greater (P<0.01) as compared to VL (Md= 28 seconds, IQR =17 seconds). Post-operative throat pain was high in DL group in comparison VL group with statistical significance (p=0.001). VL reduced the esophageal intubation rate from 14.6 % with DL to 0% (P = 0.012) but there was no difference in hemodynamic changes. The results also revealed at bivariate logistic regression that duration of intubation (p=0.006), ease of intubation (p=0.001), and Cormack Lehane grade (p<0.001) were significant determinants of first attempt success during video laryngoscope.
Conclusion: use of video laryngoscope improves duration of intubation, reduces postoperative throat pain and esophageal intubation. Nevertheless, there was no differences on first attempt success. Video laryngoscope proves to be superior.
Keywords
<p>Endotracheal intubation; Video and direct laryngoscopy; Airway management</p>
Article Details
1. Background
Endotracheal intubation remains the gold standard for securing airway during emergency situations, elective surgeries and is a vital skill for anesthesiologists to master in daily practice [1,2]. Intubating the trachea and securing the airway remains a challenge, although it is a routine practice for the anesthesiologist [3]. Since its introduction in the 1940s, direct laryngoscopy has become the standard device and technique to facilitate tracheal intubation with visualization of the glottic entrance [4]. A laryngoscope is an instrument used to examine the larynx and to facilitate intubation of the trachea. The handle usually contains batteries to light a bulb on the blade tip. The Macintosh and Miller blades are the most popular curved and straight designs, respectively. The choice of blade depends on personal preference and patient anatomy [5].
The viewing angle of the direct laryngoscope has been measured at 15 degree and is restricted by oropharyngeal structures and position of the patient this makes intubation difficult with increased failure rate (ref). Despite rapid improvements in medical technology and the above restrictions, direct laryngoscope remains the main stay of intubation around the world. Intubation using direct laryngoscopy can be a challenging task during difficult airway (e.g. patients with cervical spine immobilisation) and when confined spaces are encountered. The introduction of video laryngoscopy had provided a better approach and visualization of airway intubation [1].
Video laryngoscope was introduced into clinical practice to ease endotracheal intubation and facilitate intubation in less experienced practitioners. Video laryngoscopes are equipped with a camera on the tip of the blade, enabling better visualization of the airway anatomy and ultimately making it easier to visualize the entrance to the larynx [6]. Video laryngoscope allows a wider viewing angle and makes alignment of the oral, pharyngeal and tracheal axes unnecessary [7]. Moreover, ease of use, short learning curves and flexibility makes video laryngoscope potential substitutes to conventional direct laryngoscope.
The CMAC® video laryngoscope (Karl Storz GmbH & Co. KG, Tuttlingen Germany) evaluated in this study uses Macintosh-shaped blades, with two approaches to visualize the glottis: first, the direct view of the glottis; and second, an indirect view by means of a miniature camera on the screen of the monitoring unit [8]. Several studies have shown the successful use of the C- MAC® in the operating room and in prehospital emergency medicine seem promising for airway management. Video laryngoscopes contain a small camera and a light source at the distal third of the blade. The video picture is transferred to a monitor [8]. Entrance of Laryngoscope and endotracheal tube through the larynx can lead to sympathetic stimulation (hemodynamic changes), which mainly resulted to the degree of manipulation. Hence the use of video laryngoscope needs less manipulation and leads to minimum hemodynamic stress [3].
In Eritrea conventional laryngoscope are dominantly practiced for almost all procedures, whereas video laryngoscopes is reserved for difficult intubation. Some studies found out routine airway intubation by using video laryngoscope is significantly faster than direct laryngoscopy. The focus of this study was to use Video Laryngoscopy as routine instrument for all surgery requires general anesthesia. Since it has many advantages such as first attempt success, high success rate, fast response time, reduced airway trauma, hemodynamic stability and decreased number of attempts [9].
The aim of the study was to compare Video Laryngoscopy and Direct Laryngoscopy Endotracheal Intubation during elective at the two National Referral Hospitals in Eritrea.
2. Methods
2.1 Study Design
A comparative interventional study design was conducted from November to February, 2022.
2.2 Study Area
The study was carried out in the two National Referral Hospitals (HNRH and ONRH) which are situated in Asmara, Eritrea.
Orotta National Medical Surgical Referral Hospital is the primary largest public hospital built in 2004 and comprises 517 beds with 385 clinical staff members. According to the compiled results from the Orotta archive, the hospital provides service to an estimated 169,204 people annually who are referred from all over the country. Out of these 3,081 patients are expected to go through surgeries. The department conducts general surgeries, urologic surgeries, and emergency surgeries. In addition, ENT, dental and obstetric gynaecological surgeries are also conducted in their respective specialty departments. Per year around 891 patients are taking general anaesthesia.
Halibet National Referral Hospital is situated southeast of Asmara and is the second largest hospital in Asmara which provides medical and surgical service to all patients. It comprises three surgical departments general, orthopaedic and burn, which provides service to all age groups. According to the Halibet archive annual report a total of 236 inpatient beds are accommodated with 194 staff. On the (HMIS) report 3617 surgeries were done on 2020, in which 959 patients had general anaesthesia out of this 250 belongs to burn 433 orthopaedic and 392 for general OR.
2.3 Study population
Elective adult patient’s ≥ 18 years of age, ASA I and II who underwent general anaesthesia during the study period were included. While patents who were intubated before arrival to operation theatre decline to participate in the study, with hemodynamic instability and known history of difficult intubation were excluded from the study. The total number of surgeries from the hospitals was accessed from the previous records and also from the flow of patients. From the previous records, the estimated three months’ numbers of surgeries done in the two hospitals were 200 collectively.
2.4 Sample size and Sampling Technique
Sample size is calculated using G-power software. The parameters used include the effect size (f=0.30), type I error (α=0.05), type II error (power=0.80) and number of groups (g=2). The sample size which will be included was found 90 subjects. Taking 5% non-response; the final sample size was 96, with F test family statistical tool; of ANOVA, fixed effects and one way, and a-prior power analysis. Systematic random sampling was used on those elective patients who took general anaesthesia, in which every 2nd subject was selected. Participants were allocated to either of the 2 groups using lottery.
2.5 Data collection tools and methods
Data was collected using a questionnaire. The questionnaire includes two portions: socio demographic variables and clinical variables. Socio demographic variables include age, gender, marital status, occupational status. The clinical variables included preoperative and intraoperative factors. Pre-operatively patients were assessed for the following criteria: Neck mobility, Mallampati grade, TMD in cm, HMD in cm, mouth opening in cm, ASA classification and type of surgery. Intra operative included: duration of intubation, vital signs before induction, 1 min after induction and 5 min after induction, number of attempts, ease of intubation, Cormack lehane grade, airway trauma, esophageal intubation, and postoperative throat pain.
2.6 Data Collection Method and Procedure
After getting permission from OCMHS and MOH scientific research and ethical committee, a written informed consent was taken from each participant. Then a researcher-based questionnaire was taken to document pertinent patient’s socio-demographic and clinical variables. Then the participants were divided into two groups randomly, 48 patients on each group. All laryngoscopy and intubation procedures, and preoperatively recorded patient’s characteristics and airway assessments were performed by the main researcher. Inclusion criteria included elective, ASA grade I and grade II, all Mallampati grades, age greater than 18. Patients in both groups were monitored using standard anesthesia monitors including oxygen saturation, pulse, blood pressure, mean arterial pressure and respiratory rate. After preoxygenation, anesthesia was induced intravenously using fentanyl 1 μg.kg-1 and propofol 2 mg.kg-1. After confirmation of adequate bag mask ventilation, neuromuscular relaxation was introduced using 1-1.5 mg.kg-1 of succinylcholine. The first group was intubated using video laryngoscope (VL) and the second group using direct laryngoscope (DL). An independent observer recorded the duration, numbers of attempts for intubation, Cormack lehane visuality, and hemodynamic status, ease of intubation, airway trauma, esophageal intubation and postoperative throat pain. Tracheal intubation duration was defined as the time between introductions of the device between the two incisors until the entry of the tube to the vocal cords. If the first attempt failed, then the patient was ventilated using bag and mask and 100% oxygen to avoid desaturation, and the duration of subsequent attempt added to the time required to secure the airway. Eventually airway trauma was noted and was as summed when the blade of the intubating aid was stained with blood.
2.7 Ethical consideration
This study protocol for this research project was approved by the Research and Ethical Clearance Committee of the Orotta College of medicine and Health Sciences (OCMHS), and the Ministry of Health (MOH) Research Ethical Approval Committee. Furthermore, additional approval was sought from the hospital director to conduct the study. The aim, methods, and procedures of the study and the affiliations of the researchers were explained to the study participants in detail. Only competent adult patients who gave their written informed consent were included in the study. The researchers ensured that the study protocol and procedures would not cause any harm to the participants; all the procedures and medications used were in accordance with the hospital guidelines and were performed under the supervision of professionals. The privacy of participants was ensured as all data was collected anonymously. And the confidentiality of the data collected was maintained according to the college protocol, as data was only used for the purpose of the current study. All the participants had the right to withdraw from the study at any point during the data collection time.
2.8 Statistical analysis
Data was cleared, coded and entered into SPSS (version 25) for analysis. After data entry, the data was again cleaned and explored to check the normality of the continuous variables’ scores obtained from the indicators of video and direct laryngoscopy. Data was expressed as the mean (standard deviation) for normally distributed and the median (interquartile range) for non-Gaussian variables. The comparison of direct and video laryngoscope across the categories of qualitative variables was performed using Pearson’s chi-square test and Fisher’s exact test when appropriate. The comparison of quantitative variables between direct and video laryngoscope was performed using either independent samples t-test (if normal) or Mann-Whitney U test (if not normally distributed). Factors affecting first attempt success were determined using logistic regression. The odds ratio (95% CI) was computed and reported. The differences were considered statistically significant, if p < 0.05.
3. Results
All sampled (n=96) patients were willing to participate, yielding a response rate of 100 %.
3.1 Demographic characteristics
The summary of demographic characteristics of the patients under direct and video laryngoscope is shown in Table 1. The mean age of the patients who were under direct and video laryngoscope was 48.33 (SD=15.15) and 49.06 (SD=13.09) respectively. The proportion of males who were under direct (31.3%) was not significantly different (p=0.827) from those who were under video laryngoscope (33.3%). Moreover, marital status (p=0.206) and educational level (p=0.583) under direct and video laryngoscope were not significantly different. Almost one third of the employed patients were under direct laryngoscope (37.5%) and similar number of employed patients were under video laryngoscope (35.4%). Participants from Orotta hospital (ONRH) under direct laryngoscope (45.8%) and video laryngoscope (27.1%) were not significantly different.
|
Variables |
Direct Laryngoscopy n (%) |
Video Laryngoscope n (%) |
Total n (%) |
p value |
|
Gender |
||||
|
Male |
15 (31.3) |
16 (33.3) |
31 (32.3) |
0.827 |
|
Female |
33 (68.8) |
32 (66.7) |
65 (67.7) |
|
|
Marital status |
||||
|
Married |
39 (81.3) |
44 (91.7) |
83 (86.5) |
0.206 |
|
Single |
8 (16.7) |
3 (6.3) |
11 (11.5) |
|
|
Divorced |
0 (0) |
1 (2.1) |
1 (1.0) |
|
|
Widowed |
1 (2.1) |
0 (0) |
1 (1.0) |
|
|
Educational level |
||||
|
Illiterate |
12 (25.0) |
15 (31.3) |
27 (28.1) |
0.583 |
|
Elementary |
13 (27.1) |
7 (14.6) |
20 (20.8) |
|
|
Minor |
10 (20.8) |
9 (18.8) |
19 (19.8) |
|
|
Secondary |
6 (12.5) |
9 (18.8) |
15 (15.6) |
|
|
Post-secondary |
7 (14.6) |
8 (16.7) |
15 (15.6) |
|
|
Occupational status |
||||
|
Employed |
18 (37.5) |
17 (35.4) |
35 (36.5) |
0.832 |
|
Unemployed |
30 (62.5) |
31 (64.6) |
61 (63.5) |
|
|
Site (Hospital) |
||||
|
Orotta (ONRH) |
22 (45.8) |
13 (27.1) |
35 (36.5) |
0.056 |
|
Halibet (HNRH) |
26 (54.2) |
35 (72.9) |
61 (63.5) |
|
|
Direct Mean (SD) |
Video Mean (SD) |
Overall Mean (SD) |
p-value |
|
|
Age |
48.33 (15.15) |
49.06 (13.09) |
48.7 (14.09) |
0.801 |
Table 1: Demographic characteristics of the study participants.
3.2 Clinically related background characteristics
The proportion of patients under direct and video laryngoscope across the categories of clinically related background characteristics is shown in Table 2. Almost seventy percent of the patients under direct (70.8%) and video laryngoscope (68.8%) were at Mallampati grade I. The distribution of the patients by ASA classification under direct laryngoscope and video laryngoscope was perfectly the same (p=1.000). However, significant difference (p=0.037) on patients with CROM <350 under direct laryngoscope (6.3%) was observed when compared to those under video laryngoscope (20.8%). Similarly, slight difference in proportion of patients with TMD categories was observed between direct and video laryngoscope (p=0.037). However, there was homogenous number of participants across the categories of HMD (p=0.399) and MO (p=0.336) under both direct and video laryngoscope.
|
Variables |
Direct Laryngoscope n (%) |
Video Laryngoscope n (%) |
Total n (%) |
p-value |
|
Mallampati grade |
||||
|
Grade I |
34 (70.8) |
33 (68.8) |
67 (69.8) |
0.309 |
|
Grade II |
12 (25.0) |
15 (31.3) |
27 (28.1) |
|
|
Grade III |
2 (4.2) |
0 (0) |
2 (2.1) |
|
|
ASA classification |
||||
|
ASA I |
36 (75.0) |
36 (75.0) |
72 (75.0) |
1.000 |
|
ASA II |
12 (25.0) |
12 (25.0) |
24 (25.0) |
|
|
Cervical Range of Motion (CROM) |
||||
|
35o |
3 (6.3) |
10 (20.8) |
13 (13.5) |
0.037 |
|
>35o |
45 (93.8) |
38 (79.2) |
83 (86.5) |
|
|
Thyro-mental distance (TMD) |
||||
|
>=6.5 cm |
45 (93.80 |
38 (79.20 |
83 (86.5) |
0.037 |
|
6.5 cm |
3 (6.3) |
10 (20.8) |
13 (13.5) |
|
|
Hyo-mental Distance (HMD) |
||||
|
3cm |
2 (4.2) |
4 (8.3) |
6 (6.3) |
0.399 |
|
>cm |
46 (95.8) |
44 (91.7) |
90 (93.8) |
|
|
Mouth Opening (MO) |
||||
|
4cm |
44 (91.7) |
41 (85.4) |
85 (88.5) |
0.336 |
|
>4cm |
4 (8.3) |
7 (14.6) |
11 (11.5) |
|
Table 2: Percentage distribution of the patients according to their clinical characteristics.
3.3 Comparison of vital signs and duration of intubation between DL and VL
Comparison of the vital signs and duration of intubation was performed between DL and VL using independent samples T-test or Mann-Whitney U test, depending on the normality of the data as shown in Table 3.
|
Variable |
Md/SD, Md/IQR |
M/SD, Md/IQR |
Min, Max |
Min, Max |
t/Z-value |
p-value |
|
Direct |
Video |
Direct |
Video |
|||
|
Duration of intubations |
40 (24) |
28 (17) |
21, 160 |
10, 120 |
-4.5 |
<0.001 |
|
SPO2 at baselinen |
97 (2.06) |
96.67 (1.86) |
92, 100 |
93, 100 |
0.831 |
0.408 |
|
SPO2 after inductions |
100 (1) |
100 (1) |
94, 100 |
89, 100 |
-0.505 |
0.614 |
|
SPO2 after 1 minutes |
100 (1) |
99 (2) |
96, 100 |
94, 100 |
-0.679 |
0.497 |
|
SPO2 after 5 minutess |
96 (100) |
99.5 (2) |
96, 100 |
94, 100 |
-1..085 |
0.278 |
|
PR at baselinen |
94.63 (18.49) |
88 (17.82) |
59, 144 |
51, 121 |
1.759 |
0.082 |
|
PR after inductionn |
92.50 (17.12) |
92.13 (15.47) |
56, 140 |
57, 134 |
0.113 |
0.911 |
|
PR after 1 minuten |
95.25 (18.41) |
92.44 (17.90) |
50, 138 |
59, 135 |
0.759 |
0.45 |
|
PR after 5 minutess |
90 (15) |
90 (18) |
60, 145 |
55, 129 |
-0.084 |
0.933 |
|
MAP at baselines |
99 (16) |
98 (24) |
60, 163 |
62, 124 |
-0.084 |
0.933 |
|
MAP after inductions |
86.5 (27) |
88 (18) |
52, 132 |
62, 164 |
-1.092 |
0.275 |
|
MAP after 1 minuten |
94.35 (24.88) |
89.95 (19.02) |
43, 153 |
62, 137 |
0.996 |
0.322 |
|
MAP after 5 minutess |
89.5 (25) |
86.5 (22) |
44, 167 |
55, 128 |
-0.509 |
0.61 |
Table 3: Vital signs and duration of intubation comparison between DL and VL.
The median time to intubation under DL (Md=40 seconds, IQR=24 seconds) was significantly greater (P<0.01) as compared to that of VL (Md= 28 seconds, IQR =17 seconds). However, there was no significant difference between DL and VL across the change in vital signs.
3.4 Comparison of DL and VDL during intubation
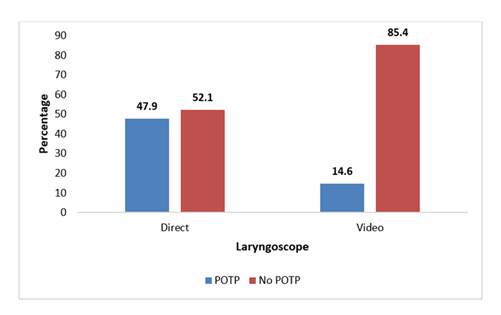
The potential variables that might have association with the use of direct and video laryngoscope during intubation were assessed using Fisher’s exact test and presented in Table 4. The result showed that the presence of post-operative throat pain under direct laryngoscope (47.9%) was significantly greater (p=0.001) than those under video laryngoscope (14.6%).
Moreover, significantly higher proportion of esophageal intubation (p=0.012) were observed under DL (14.6%) as compared to VL (0%). However, there was no significant difference between usage of DL or VL across the categories of ease of intubation (p=0.311), presence of airway trauma (p=0.238), Cormack Lehane grade (p=0.577), success of intubation (p=1.000), and drug type (p=0.292) (Figure 1).
|
Variables |
Laryngoscope |
Chi-square value |
Fisher's p-value |
|
|
Direct n (%) |
Video n (%) |
|||
|
Ease of intubation |
||||
|
Easy |
29 (60.4) |
35 (72.9) |
2.805 |
0.311 |
|
Satisfactory |
15 (31.3) |
8 (16.7) |
||
|
Difficult |
4 (8.3) |
5 (10.4) |
||
|
Presence of airway trauma |
||||
|
Yes |
15 (31.3) |
9 (18.8) |
- |
0.238 |
|
No |
33 (68.8) |
39 (81.3) |
||
|
Cormack Lehane grade |
||||
|
Grade I |
32 (66.7) |
37 (77.1) |
1.346 |
0.577 |
|
Grade II |
13 (27.1) |
9 (18.80 |
||
|
Grade III |
3 (6.3) |
2 (4.2) |
||
|
Success of intubation |
||||
|
First attempt |
37 (77.1) |
37 (77.1) |
0.352 |
1.000 |
|
Second attempt |
8 (16.70 |
9 (18.8) |
||
|
>=3 Attempt |
3 (6.3) |
2 (4.2) |
||
|
Post-operative throat pain |
||||
|
Yes |
23 (47.9) |
7 (14.6) |
- |
0.001 |
|
No |
25 (52.1) |
41 (85.4) |
||
|
Drug type |
||||
|
Propofol |
27 (56.3) |
33 (68.8) |
- |
0.292 |
|
Thiopental |
21 (43.8) |
15 (31.3) |
||
|
Esophageal intubation |
||||
|
Yes |
7 (14.6) |
0 (0) |
- |
0.012 |
|
No |
41 (85.4) |
48 (100) |
||
Table 4: Differences in DL or VL across the categories of the variables during intubation.
3.5 Factors affecting the first attempt success
Factors affecting the first attempt success were assessed using bivariate logistic regression as shown in Table 5. The results revealed that duration of intubation (p=0.006), ease of intubation (p=0.001), and Cormack Lehane grade (p<0.001) were significant determinants of first attempt success. With unit increase in duration of intubation, the odds of first attempt success decreases by 3%. The odds of first attempt success was observed to increase with increase in easiness of intubation (p=0.001). Similarly, with increase in Cormack Lehane grade, there was significant decrement in first attempt success (p<0.001).
However, the variables age (p=0.747), gender (p=0.137), and laryngoscope used (p=1.000) were not significant determinants of the first attempt success.
Even though three variables were found to be significantly associated with first attempt success, multivariable logistic regression could not be conducted for the sample size was not modest enough to run the model.
|
Variable |
Odds Ratio |
95% CI |
p-value |
|
Age |
0.99 |
0.96, 1.03 |
0.747 |
|
Gender |
|||
|
Male |
0.48 |
0.18, 1.27 |
0.137 |
|
Female |
Reference |
||
|
Mallampati grade |
|||
|
Grade I |
3.19 |
0.19, 53.91 |
0.588 |
|
Grade II |
4.4 |
0.23, 82.98 |
|
|
Grade III |
Reference |
||
|
Sauration of intubation |
0.97 |
0.96, 0.99 |
0.006 |
|
Ease of intubation |
|||
|
Easy |
Reference |
0.001 |
|
|
Satisfactory |
0.02 |
0.002, 0.12 |
|
|
Difficult |
0 |
0 |
|
|
Cormack lehane grade |
|||
|
G-I |
Reference |
<0.001 |
|
|
G-II |
0.11 |
0.04, 0.33 |
|
|
G-III |
0.2 |
0.03, 1.36 |
|
|
Laryngoscope |
|||
|
Direct |
1 |
0.39, 2.59 |
1.000 |
|
Video |
Reference |
||
Table 5: Factors affecting first attempt success using bivariate logistic regression.
4. Discussion
This study discusses comparison of video versus direct laryngoscope during endotracheal intubation. The parameters compared were duration of intubation, first attempt success, hemodynamic statues, easy of intubation, esophageal intubation and airway trauma. Since the study was conducted in the major hospitals, it gave an informative picture on the differences of the devices.
In this study on the demographic characteristics, females accounted 67% with mean age of 48.7. There was no statical differences observed across the demographic statues and clinical variables. Similarly study done in Germany found out no differences in their demographic variables [8]. The median time to intubation was 40 seconds (IQR = 24 seconds) using DL and 28 seconds (IQR =17 seconds) for VL (P<0.01) in this study. A similar study done by Vanderbilt et al. [10] found out the median time to intubations was 25 seconds (interquartile range [IQR] = 16–44 seconds) using DL and 20 seconds (IQR =12–35 seconds) for VL (P<0.01) [10]. Similarly, a study done in is Israel reported the time to intubation was 218 seconds in the DL group and 120 seconds in the GVL group (p < 0.01). Congruent with the above findings a study done in turkey among elective pediatric patients found out the mean intubation time were significantly shorter with video C Mac D-Blade (p<0.001) [11]. Similarly, Mosier et al. [9] reported ultimate success rate was greater in VL (98.35) in comparison to DL (91.2%) [9]. Incongruent, a study done by Panwar et al. [3] reported the time of intubation was statistically significant longer in the (VL) Glide Scope (15.96.7 seconds) than in the Macintosh with a P value of < 0.05 (P value=0.000) [3]. A study done in the USA revealed that there was no statistical difference on the duration of intubation among VL and DL (P= 0.341) [1]. Regarding the hemodynamic statues, there was no significant difference between DL and VL across the change in vital signs. Similarly, studies done in India and turkey reported no changes on haemodynamic statues [3,11]. Inconsistent, a study done by Abdelgadir et al. [12] found out changes on oxygen saturation and heart rate after 5min after intubation (p=0.007) [12]. Incongruent to current findings, a study done in USA reported desaturation in oxygenation and hypotension.
In this study there was no significant difference between DL and VL at the first attempt success (p=1.00). However, duration of intubation, ease of intubation, and Cormack Lehane grade were significant determinants of first attempt success. Congruently, a study done in Poland found out the first-pass success rate in McGrath MAC video laryngoscope did not change when compared with Macintosh laryngoscope [6]. Incongruent to this finding’s studies done in USA, Germany, Japan and India reported that video laryngoscope had a higher first attempt success [1,3,4,7,8].
In this study there was no statistically significant in ease of intubation, airway trauma and drug used. Incongruent to this findings, a study done in India reported there was statistical significance on the ease of intubation (P= 0.000) [3]. Esophageal intubation was higher in DL (14.6%) compared to VL (0%) with (p=0.012). Similar with these findings studies done in USA stated less esophageal intubation with the use VL [4,7,9].
The incidence of post-operative throat pain under direct laryngoscope (47.9%) was significantly greater (P=0.001) than video laryngoscope (14.6%). This could be due to the curvature of C-MAC Blade and the presence of camera, which leads to less force during laryngoscopy, hence this leads to less tissue trauma. Congruent to this finding, a study done by Panwar et al, found out that (74%) patients had throat pain with DL in comparison to (26%) in VL [3].
5. Conclusion and Recommendation
The overall findings observed VL proven to have less time of intubation, reduced post- operative throat pain and fewer esophageal intubations in comparison to DL. However, first attempt success rate, Presence of airway trauma, Cormack Lehane grade, drug type, ease of intubation, and haemodynamic status was found to be statistically insignificant. Overall, these findings demonstrate the efficacy and superiority of VL. Provision of training and workshops regarding VL would improve the current practice.
References
- Su Y-C, Chen C-C, Lee Y-K, et al. Comparison of video laryngoscopes with direct laryngoscopy for tracheal intubation: a meta-analysis of randomised trials. Eur J Anaesthesiol 28 (2011): 788-95.
- Ecker H, Kolvenbach S, Stranz S, et al. Comparison of the novel VieScope with conventional and video laryngoscope in a difficult airway scenario–a randomized, controlled simulation trial. BMC Emerg Med 21 (2021): 1-6.
- Panwar N, Vanjare H, Kumari M, et al. Comparison of video laryngoscopy and direct laryngoscopy during endotracheal intubation–A prospective comparative randomized study. Indian Journal of Clinical Anaesthesia 7 (2020): 438-43.
- Sakles JC, Mosier J, Chiu S, et al. A comparison of the C-MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Ann Emerg Med 60 (2012): 739-48.
- Miller RD, Eriksson LI, Fleisher LA, et al. Miller's anesthesia e-book: Elsevier Health Sciences (2014).
- Ruetzler K, Szarpak L, Smereka J, et al. Comparison of direct and video laryngoscopes during different airway scenarios performed by experienced paramedics: a randomized cross-over manikin study. Biomed Res Int (2020): 5382739.
- Mosier J, Chiu S, Patanwala AE, et al. A comparison of the GlideScope video laryngoscope to the C-MAC video laryngoscope for intubation in the emergency department. Ann Emerg Med 61 (2013): 414-20. e1.
- Noppens RR, Geimer S, Eisel N, et al. Endotracheal intubation using the C-MAC® video laryngoscope or the Macintosh laryngoscope: a prospective, comparative study in the ICU. Crit Care 16 (2012): 1-8.
- Mosier JM, Whitmore SP, Bloom JW, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care 17 (2013): 1-9.
- Vanderbilt AA, Mayglothling J, Pastis NJ, et al. A review of the literature: direct and video laryngoscopy with simulation as educational intervention. Adv Med Educ Pract 5 (2014): 15-23.
- Hajiyeva K, Can ÖS, Baytaş V, et al. Comparison of the C-MAC D-Blade videolaryngoscope and direct laryngoscope in pediatric patients: Randomized controlled trial. Ulus Travma Acil Cerrahi Derg 27 (2021): 421-6.
- Abdelgadir IS, Phillips RS, Singh D, et al. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev 5 (2017): CD011413.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 