Effect of Inspiratory Muscle Training on Respiratory Muscle in Patients Undergoing Open Heart Surgery
Chitima Kulchanarat1*, Suphannee Choeirod1, Supattra Thadatheerapat1, Dusarkorn Piathip2, Opas Satdhabudha3, Kornanong Yuenyongchaiwat4,5
1Department of physical Therapy, Thammasat University Hospital, Pathum Thani, Thailand
2Cardiovascular Thoracic Surgery (CVT) unit, Thammasat Medical Hospital
3Division of Cardiovascular Thoracic Surgery, Department of surgery, Thammasat University Hospital, Thailand
4Department of physiotherapy, Faculty of Allied Health Sciences, Thammasat University, Pathum Thani, Thailand
5Thammasat University research unit in physical therapy in cardiovascular and respiratory systems, Thailand
*Corresponding Author: Chitima Kulchanarat, Department of physical Therapy, Thammasat University Hospital, Pathum Thani, Thailand.
Received: 27 March 2024; Accepted: 05 April 2024; Published: 12 April 2024
Article Information
Citation:
Chitima Kulchanarat, Suphannee Choeirod, Supattra Thadatheerapat, Dusarkorn Piathip, Opas Satdhabudha, Kornanong Yuenyongchaiwat. Effect of Inspiratory Muscle Training on Respiratory Muscle in Patients Undergoing Open Heart Surgery. Archives of Physiotherapy and Rehabilitation 7 (2024): 01-10.
View / Download Pdf Share at FacebookAbstract
Background: Patients undergoing open-heart surgery (OHS) are at risk of postoperative pulmonary complications and decreased functional capacity (FC) of the lungs. Respiratory muscle training (RMT) is reported to be effective in improving respiratory muscles strengthening (RMS) and FC. Aim: To investigate the effects of RMT on the respiratory muscles of patients undergoing OHS. Design: A randomized controlled trial Setting: Thammasat University Hospital Population: Patients undergoing OHS. Methods: Fifty-eight patients who underwent OHS were randomly assigned to two groups: 29 in the control group (CG) and 29 in the training group (TG). The patients in the TG underwent physical therapy program and RMT using a breath trainer. Patients in the CG underwent physical therapy only. The maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP) and 6-minute walk test (6MWT) were assessed pre- and post-operatively. Results: The TG had significant increase in MIP (46.70±24.98 vs. 61.40±28.46 cmH2O, P<0.001), MEP (40.06±22.83 vs. 62.30±22.64 cmH2O, P<0.001) and 6-MWT (172.73±88.11 vs. 208.26±89.42 m, P=0.013). The CG had significant decrease in MIP (42.23±20.26 vs. 23.46±9.94 cmH2O, P<0.001), MEP (35.90±24.35 vs. 23.10±15.03 cmH2O, P=0.002) and 6MWT (150.83±91.79 vs. 76.6±67.67 m, P<0.001). Conclusion: RMT effectively improved RMS and FC in patients undergoing OHS.
Keywords
<p>Respiratory muscle; Heart surgery; Inspiratory muscle training; Functional capacity</p>
Article Details
Introduction
Coronary artery bypass grafting (CABG) and heart valve surgery are the most commonly performed cardiac surgical procedures worldwide. [1] CABG is used to treat myocardial perfusion in coronary artery disease (CAD) which is caused by plaque or cholesterol deposition on the walls of the coronary arteries. Consequently, this restricts blood flow of the coronary arteries, which deliver the blood vessels that supply nutrients and oxygen to the heart muscle. This leads to abnormal heart rhythms, heart failure, chest pain and shortness of breath [2,3,4,5]. In cardiac surgery, the use of narcotic drugs, anesthetics and the discontinuation of ventilation during cardiopulmonary bypass (CPB) are associated with post-cardiac surgery pain, which lead to decreased ciliary function, dysfunction of the respiratory muscles and deteriorated effectiveness of cough. [9] CPB is responsible for oxidative stress, leading to pulmonary ischemic reperfusion, which induces lung injury and a systemic inflammatory response. [6,7] This respiratory dysfunction leads to pulmonary complications such as atelectasis, prolonged mechanical ventilation, pneumonia, pulmonary congestion, in addition to systemic infections, perioperative stroke, upper gastrointestinal bleeding, diabetes mellitus, renal failure and hemodynamic complications. [8,9] This leads to reduced muscle strength, functional capacity, insulin sensitivity and mortality. Respiratory muscle training is one of the procedures used to promote maximum inspiratory pressure, maximum expiratory pressure and functional capacity. [10] The recommendation for physiotherapy treatment consists of breathing techniques, coughing techniques, incentive spirometry, continuous positive airway pressure, intermittent positive pressure, positioning, early mobilization and RMT. [10,11] Several studies have reported that RMT is effective in the recovery of maximum inspiratory pressure, maximum expiratory pressure and functional capacity. For example, Cordeiro et al. examined an RMT of 40% of the maximum inspiratory pressure, performing three sets with 10 repetitions. They revealed that RMT led to improved RMS, and enhanced walking distance, which also resulted in increased maximum inspiratory pressure and 6MWT scores. Various RMT methods, techniques, devices, and protocols are available. Inspiratory pressure threshold loading such as breathing via a device, is the most widely used method for improving RMS. Based on the results of previous studies, RMS can be increased by using a TU-BT through which users breathe while attached to the lower costal margin [16,30]. Therefore, this study aimed to investigate the effects of RMT on the respiratory muscles of patients who underwent open heart surgery.
Material and Methods
This randomized controlled trial was conducted between January 2023 and January 2025, at the Intensive Care Unit and Surgical Department of Thammasat University Hospital. The number of patients required for the study was calculated according to Cordeiro et al. (2016) with a statistical G*Power of 0.8. The total sample size was determined to be 52 patients divided into two groups: 26 patients in each group and eight patients in case of drop-outs. The study enrolled patients aged 35-80 years, both males and females who were scheduled to undergo cardiac surgery (CABG, mitral valve, aortic valve and atrial septal defect correction), The lottery method was used to randomly divide patient into two groups (control and training). Patients who did not understand the techniques, had neurological conditions (e.g., stroke and traumatic brain injury), psychiatric problems, thoracotomy, unstable angina, uncontrolled cardiac arrhythmia, hemodynamic instability, high resting heart rate (≥ 120 beats per minute), uncontrollable blood pressure or blood glucose levels were excluded from the study. This study was approved by the Ethics Human Committee of Thammasat University, based on the Declaration of Helsinki, and all participating patients signed an informed consent form. The RMT was measured using a respiratory pressure meter (RPM 01, Micro Medical Ltd., United Kingdom). The maximum inspiratory pressure was measured during the maximum inspiratory effort from the residual volume and the maximum expiratory pressure was measured during the maximum expiratory effort from the total lung capacity. Measurements were taken with each participant seated on a chair and wearing a nose clip. Patients were asked to breathe as much as possible for at least 1 second. The evaluation was repeated until no further improvements were obtained, and three satisfactory attempts that differed by < 20% were used for the analysis. The highest value was recorded in centimeters of water (cmH 2O). The American Thoracic Society/European Respiratory Society recommends a standard testing protocol for RMS. [15] Patients who underwent OHS were asked to perform RMS before the heart operation and before discharge.
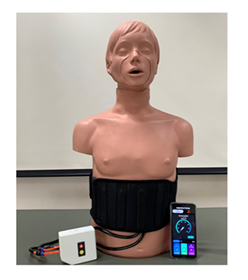
Functional capacity was measured using the 6-MWT. The patients were instructed to walk as fast as possible along a 30 m straight, flat hospital corridor for 6 min. The total distance walked was measured to the nearest meter and recorded. Before and after the test, all patients were monitored for resting heart rate, respiratory rate, peripheral oxygen saturation and blood pressure in the sitting position. All patients received the standard cardiac rehabilitation program pre- and post-operatively (i.e., cardiac rehabilitation program phase I). RMT was performed using a TU-BT device. Patients wore a device attached to a chest strap at the lower costal margin (Figure 1). All the patients were asked to sit on a chair and take a deep breath for 10 min, performing three sets of 15 repetitions. The training group was performed twice daily until hospital discharge, according to the study protocol. The CG continued the cardiac rehabilitation program during phase I. The principle of this device has been described in detail elsewhere [30]
Statistical analysis
The collected data were analyzed using the SPSS statistical software version 20. Normality of distribution was assessed using the Kolmogorov-Smirnov test. Descriptive statistics were used to explain the features of the sample population and are reported as frequencies and percentages. Chi-squared tests were used to assess the existence of associations between qualitative variables. The maximum inspiratory pressure, maximum expiratory pressure and 6MWT were compared using factor analysis of variance (ANOVA).
Results
From to January 2023 until January 2025 ,60 patients were included, the mean age was 62.92 ±8.49 years. The patients underwent CABG (n =40), valve surgery (n =15) or CABG plus valve surgery (n =5). Two participants did not complete the study due to cardiac arrest post-surgery. Therefore, patients who underwent OHS were randomly assigned randomly to two groups: 29 in the CG and 29 in the TG, (Figure 1).
There were no significant differences in the characteristics of patients included in each
group (Table 1). Patients in the TG underwent a physical therapy program and RMT using a TU-BT device whereas those in the CG underwent the physical therapy program only.
|
Total (N=60) Mean (SD) |
Intervention group (N=30) Mean (SD) |
Control group (N=30) Mean (SD) |
P value |
|
|
Sex |
0.190 |
|||
|
Female (%) |
25(41.6) |
10(33.3) |
15(50) |
|
|
Male (%) |
35(58.4) |
20(66.7) |
15(50) |
|
|
Age (year) |
62.92(8.49) |
61(8.61) |
64.83(8.08) |
0.77 |
|
Comorbidities |
||||
|
Diabetes mellitus (%) |
0.28 |
|||
|
Underlying of diabetes mellitus |
38(63.3) |
17(28.3) |
21(35) |
|
|
No history of diabetes mellitus |
22(36.7) |
13(21.7) |
9(15) |
|
|
Dyslipidemia (%) |
0.78 |
|||
|
Underlying of dyslipidemia |
41(68.3) |
20(33.3) |
21(35) |
|
|
No history of dyslipidemia |
19(31.7) |
10(16.7) |
9(15) |
|
|
Hypertension (%) |
1.00 |
|||
|
Underlying of hypertension |
12(20) |
24(40) |
24(40) |
|
|
No history of hypertension |
48(80) |
6(10) |
6(10) |
|
|
Surgical procedures |
0.55 |
|||
|
CABG |
40 (66.7) |
22(36.7) |
18(30) |
|
|
Valve surgery |
15(25) |
6(10) |
9(15) |
|
|
CABG plus valve surgery |
5(8.3) |
2(3.3) |
3(5) |
|
|
Classification of NYHA class |
0.201 |
|||
|
I |
22(36.7) |
14(23.3) |
8(13.3) |
|
|
II |
31(51.7) |
14(23.3) |
17(28.3) |
|
|
III |
7(11.7) |
2(3.3) |
5(8.3) |
|
|
LVEF (%) |
46.37(15.2) |
48.85(14.7) |
43.9(15.5) |
0.07 |
|
MIP (cmH2O) |
44.47(22.7) |
46.70 (24.98) |
42.23(20.26) |
0.45 |
|
MEP (cmH2O) |
37.98(23.5) |
40.06(22.83) |
35.90(24.35) |
0.49 |
|
6MWD (meters) |
161.78(89.9) |
172.73(88.11) |
150.83(91.79) |
0.35 |
|
CABG: Coronary Artery Bypass Graft; NYHA; New York Heart Association, LVEF; left ventricular ejection fraction; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure; 6 minute walk distance *Analyzed by χ2 test. |
||||
Table 1: Baselines characterize data.
Respiratory muscle strength
Table 2 shows the TG had significant increases in maximum inspiratory pressure (46.70±24.98 vs. 61.40±28.46 cmH2O, P<0.001) and maximum expiratory pressure (40.06±22.83 vs. 62.30±22.64 cmH2O, P<0.001) whereas the CG had significant decreases in maximum inspiratory pressure (42.23±20.26 vs. 23.46±9.94 cmH2O, P<0.001), and MEP (35.90±24.35 vs. 23.10±15.03 cmH2 O, P=0.002).
Functional capacity
Table 2 shows the differences in values of the 6MWT for the TG (172.73±88.11 vs. 208.26±89.42 m, P=0.013). and the CG (150.83±91.79 vs. 76.6±67.67 m, P<0.001).
|
Variable |
Group |
Mean difference (SE) Intervention-control |
P value between Groups |
||
|
Intervention (N=30) |
Control (N=30) |
||||
|
MIP (cmH2O) |
|||||
|
Before mean (SD) |
46.70 (24.98) |
42.23(20.26) |
4.46(5.87) |
0.45 |
|
|
After mean (SD) |
61.40(28.46) |
23.46(9.94) |
37.93(5.51) |
<0.001 |
|
|
Mean difference (before-after) (SE) |
-14.7(3.39) |
18.7(3.39) |
|||
|
P value within group |
<0.001 |
<0.001 |
|||
|
MEP (cmH2O) |
|||||
|
Before mean (SD) |
40.06(22.83) |
35.90(24.35) |
4.17(6.09) |
0.49 |
|
|
After mean (SD) |
62.30(22.64) |
23.10(15.03) |
39.2(4.96) |
<0.001 |
|
|
Mean difference (before-after) (SE) |
-22.23(4.02) |
12.8(4.02) |
|||
|
P value within group |
<0.001 |
0.002 |
|||
|
6 MWD (meters) |
|||||
|
Before mean (SD) |
172.73(88.11) |
150.83(91.79) |
21.9 (23.2) |
0.35 |
|
|
After mean (SD) |
208.26(89.42) |
76.6(67.67) |
131.67(20.47) |
<0.001 |
|
|
Mean difference (before-after) (SE) |
-35.53(13.85) |
74.23(13.85) |
|||
|
P value within group |
0.013 |
<0.001 |
|||
|
SD: standard deviation; SE: standard error of mean; 6 MWD: minute walking distance; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure. |
|||||
Table 2: Respiratory muscle strength and functional capacity before and after intervention program.
Discussion
We found a significant improvement in the RMS and functional capacity in the TG using the TU-BT device. RMT is widely performed using threshold loading devices such as the Powerbreathe electronic device [27,29] and the Threshold Inspiratory Muscle Trainer spring-loaded devices [10,11,23], as well recommendations from the American Thoracic Society and European Respiratory Society. [16] Moreover, threshold loading devices incorporate mouthpieces and utilize accessory muscles such as the sternocleidomastoid, trapezius, rhomboid and scalene muscle. We believe that the use of the TU-BT device in post-cardiac surgery is harmless, improves the RMS (the device can be attached to the lower costal margin) and promotes clinical benefits as well as quality of life. Cardiac surgery with CPB determines the systemic inflammatory response, which emphasizes the pulmonary origin. Blood flow in the CPB circuit releases inflammatory cytokines that cause pulmonary damage. The systemic inflammatory response is characterized by changes in pulmonary function, decreased pulmonary compliance, pulmonary edema, reduced functional residual capacity and increased respiratory effort [18]. Additionally, CABG and valve surgery are associated with pulmonary complications (atelectasis, respiratory function, poor pulmonary ventilation and impairment of gas exchange) [11]. Pulmonary dysfunction leads to increased breathing effort, which is associated with impaired pulmonary complacency of the chest wall and rib cage reduction in maximum inspiratory pressure [19]. Diaphragmatic dysfunction and weakness are associated with phrenic nerve injury post cardiac surgery [20]. Decreased lung expansion is often caused by immobilization, ineffective coughing and muscle fatigue.
Improvement in maximum inspiratory pressure and 6MWT were observed in the TG. RMT improves the size of type (IIa) muscle fibers (oxidative and white), leading to an increase in the shortening velocity of muscles, a change in the length-tension relationship on which force-generating mechanics of the respiratory system occur and a reduction in pulmonary hyperinflation. [25] RMT improves blood flow to the limb muscles, promote muscle oxygenation and reduce lactate production in the respiratory muscles. [26] Menezes et al., reported that the RMT associated with an increased period of pulmonary function recovery. Reduced RMS is associated with a decrease in functional capacity. Hence, RMT improves functional capacity and increases 6 MWT distance. The increases in maximum inspiratory pressure (18.18 cmH2O) and 6-MWT (36 m) after the RMT in our study were higher than that reported in previous studies (Cordeiro et al.2016 ; Elmarakby et al.2016).A systematic review of the effect of RMT in patients undergoing cardiac surgery reported mean differences of 4.70 cmH2O (95%CI,-4.00 to 13.4) for maximum inspiratory pressure and 78.05 m (95%CI,60.92 to 95.18) for 6MWD.[29] Differences in threshold devices, intensity ,duration ,type of intervention and sample size may explain the differences in maximum inspiratory pressure and 6MWD. We choose to follow the “ATS/ERS Statement on RMT which defines respiratory muscle weakness as maximum inspiratory pressure <80 cmH2O.In our study, the mean maximum inspiratory pressure before cardiac surgery was 47 cmH2O and mean maximum expiratory pressure was 40 cmH2O, which can be considered to indicate respiratory muscle weakness. Thus, the adequate level of RMS for counteracting postoperative pulmonary dysfunction remains unpredictable.
Conclusion
RMT can be performed using maximum pressure resistors such as TU- BT devices and is an important strategy for RMS and functional capacity in patients undergoing OHS.
Limitations
Our had several limitations. First, we did not evaluate pulmonary function or pain assessment of the incision. Second, we did not analyzed variables such as quality of life or anxiety and depression levels in the patients.
Data Availability
Data available on request.
Conflicts of interest
They have no competing interest in this study
Funding statement
The study was fully supported by a research grant number TUFT14/2566 from Thammasat University.
Acknowledgments
The authors would like to thank all the participants who participated in this study. In addition, we would also like to thank all staff from at Thammasat University Hospital.
References
- Melly L, G Torregrossa, T Lee, et al. Fifty years of coronary artery bypass grafting. J Thorac Dis 10 (2018):1960-1967.
- Sellke FW, JM.DiMaio, LR Caplan, et al. Comparing on-pump and off-pump coronary artery bypass grafting: numerous studies but few conclusions: a scientific statement from the American Heart Association council on cardiovascular surgery and anesthesia in collaboration with the interdisciplinary working group on quality of care and outcomes research. Circulation 111 (2005): 2858-2864.
- Hillis LD, PK Smith, JL Anderson, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 124 (2011): 2610-2642.
- He GW. Arterial grafts for coronary artery bypass grafting: biological characteristics, functional classification, and clinical choice. Ann Thorac Surg 67 (1999): 277-284.
- Naseer BA, AM Al-Shenqiti, ARH Ali, et al. Effect of cardiac surgery on respiratory muscle strength. J Taibah Univ Med Sci 14 (2019): 337-342.
- Jensen L, dL Yang. Risk factors for postoperative pulmonary complications in coronary artery bypass graft surgery patients. Eur J Cardiovasc Nurs 6 (2007): 241-246.
- Sasseron AB, LC Figueiredo, K Trova, et al. Does the pain disturb the respiratory function after open heart surgery?. Rev Bras Cir Cardiovasc 24 (2009): 490-496.
- Alwardt CM, D Redford, DF Larson. General anesthesia in cardiac surgery: a review of drugs and practices. J Extra Corpor Technol 37 (2005): 227-235.
- Cordeiro AL, TA de Melo, D Neves, et al. Inspiratory Muscle Training and Functional Capacity in Patients Undergoing Cardiac Surgery. Braz J Cardiovasc Surg 31 (2016):140-144.
- Savci S, B Degirmenci, M Saglam, et al. Short-term effects of inspiratory muscle training in coronary artery bypass graft surgery: a randomized controlled trial. Scand Cardiovasc J 45 (2011): 286-293.
- Barros GF, S Santos Cda, FB Granado, et al. Respiratory muscle training in patients submitted to coronary arterial bypass graft. Rev Bras Cir Cardiovasc 25 (2010): 483-490.
- Songsorn, Preeyaphorn, Sasipa Buranapuntalug. Effects of inspiratory muscle training on activity ability in patients after open heart surgery. Journal of Physical Therapy 36 (2014): 89-96.
- Winkelmann ER, F Dallazen, AB Bronzatti, et al. Analysis of steps adapted protocol in cardiac rehabilitation in the hospital phase. Rev Bras Cir Cardiovasc 30 (2015): 40-48.
- Moreno AM, RR Castro, PP Sorares, et al. Longitudinal evaluation the pulmonary function of the pre and postoperative periods in the coronary artery bypass graft surgery of patients treated with a physiotherapy protocol. J Cardiothorac Surg 6 (2011): 62.
- Green M, Road J, Sieck GC, et al. Tests of respiratory muscle strength2002: ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 166 (2002): 518-624.
- Yuenyongchaiwat, Kornanong, Sasipa Buranapuntalug, et al. Walking Performance in the 6-Min Walk Test and Gait Speed in Patients Undergoing Open Heart Surgery: A Preliminary Cohort Study. 8 (2019): 19-22.
- Bignami E, F Saglietti, A Di Lullo. Mechanical ventilation management during cardiothoracic surgery: an open challenge. Ann Transl Med 6 (2018): 380.
- Renault JA, R Costa-Val, MB Rossetti. Respiratory physiotherapy in the pulmonary dysfunction after cardiac surgery. Rev Bras Cir Cardiovasc 23 (2008): 562-569.
- Mehta Y, M Vats, A Singh, et al. Incidence and management of diaphragmatic palsy in patients after cardiac surgery. Indian J Crit Care Med 12 (2008): 91-9
- Stein R, CP Maia, AD Silveira, et al. Inspiratory muscle strength as a determinant of functional capacity early after coronary artery bypass graft surgery. Arch Phys Med Rehabil 90 (2009): 1685-1691.
- Zanini M, RM Nery, JB de Lima, et al. Effects of Different Rehabilitation Protocols in Inpatient Cardiac Rehabilitation After Coronary Artery Bypass Graft Surgery: A RANDOMIZED CLINICAL TRIAL. J Cardiopulm Rehabil Prev 39 (2019): E19-e25.
- Elmarakby, Ashraf. Effect of Threshold Inspiratory Muscle Training on Maximal Inspiratory Pressure and Pulmonary Gas Exchange in Patients Undergoing Coronary Artery Bypass Graft Surgery. Critical Reviews in Physical and Rehabilitation Medicine 28 (2017).
- Menezes TC, D Bassi, RC Cavalcanti, et al. Comparisons and correlations of pain intensity and respiratory and peripheral muscle strength in the pre- and postoperative periods of cardiac surgery. Rev Bras Ter Intensiva 30 (2018): 479-486.
- Hulzebos EH, NL van Meeteren, BJ van den Buijs, et al. Feasibility of preoperative inspiratory muscle training in patients undergoing coronary artery bypass surgery with a high risk of postoperative pulmonary complications: a randomized controlled pilot study. Clin Rehabil 20 (2006): 949-959.
- Chiappa GR, BT Roseguini, PJ Vieira, et al. Inspiratory muscle training improves blood flow to resting and exercising limbs in patients with chronic heart failure. J Am Coll Cardiol 51 (2008): 1663-1671.
- Fortes, João Vyctor Silva, Mayara Gabrielle Barbosa Borges, et al. Effects of Inspiratory Muscle Training Using an Electronic Device on Patients Undergoing Cardiac Surgery: A Randomized Controlled Trial %J International Journal of Cardiovascular Sciences. 34 (2020): 44-52.
- Kkp Menzes, Lucas Rodrigues Nascimento, Patrick Roberto Avelino, Janaíne Cunha Polese, et al. A Review on Respiratory Muscle Training Devices 8 (2018): 1-7.
- Cargnin C, M Karsten, Jcvdc Guaragna, et al. Inspiratory Muscle Training After Heart Valve Replacement Surgery Improves Inspiratory Muscle Strength, Lung Function, and Functional Capacity: A RANDOMIZED CONTROLLED TRIAL. J Cardiopulm Rehabil Prev 39 (2019): E1-e7.
- Dsouza FV, SK Amaravadi, SR Samuel, et al. Effectiveness of Inspiratory Muscle Training on Respiratory Muscle Strength in Patients Undergoing Cardiac Surgeries: A Systematic Review With Meta-Analysis. Ann Rehabil Med 45 (2021): 264-273.
- Yuenyongchaiwat, Kornanong, Chusak Thanawattano, et al. Efficiency of the Respiratory Training Prototype for Application in Hemodialysis Patients: a Preliminary Study. Philippine Journal of Science (2021).

 Impact Factor: * 1.3
Impact Factor: * 1.3 Acceptance Rate: 73.39%
Acceptance Rate: 73.39%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 