Management of Malnutrition in Adult Patients in Intensive Care Units in Cameroon Using an Enteral Nutrition Formula Based on Local Ingredients
Njall Pouth Clotilde¹*, Dissongo Jean II1, Mbiatat Hilaire de Goethe2, Kenne Wando Achile3, Solle Jeremie4, Nso Emmanuel3, Eboumbou Else Carole1
1Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Carrefour Ange Raphaël, Douala, Cameroon
2Douala General Hospital, Cameroon
3 National Higher School of Agro-Industrial Sciences, University of Ngaoundéré, Cameroon
4Douala Laquintinie Hospital, Cameroon
*Corresponding Author: Dr. Njall Pouth Clotilde, Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon.
Received: 26 July 2025; Accepted: 07 August 2025; Published: 18 August 2025
Article Information
Citation: Njall Pouth Clotilde, Dissongo Jean II, Mbiatat Hilaire de Goethe, Kenne Wando Achile, Solle Jeremie, Nso Emmanuel, Eboumbou Else Carole. Management of Malnutrition in Adult Patients in Intensive Care Units in Cameroon Using an Enteral Nutrition Formula Based on Local Ingredients. Anesthesia and Critical care 7 (2025): 53-57.
View / Download Pdf Share at FacebookAbstract
Background: Hospital malnutrition is often overlooked in developing countries, although adequate nutritional support is essential for optimizing patient care. This study aimed to develop and evaluate the effectiveness of an enteral nutrition formulation prepared from local ingredients.
Methods: A prospective study was conducted on 77 adult patients admitted to intensive care. Protein, energy, and immune markers were assessed upon admission, and an enteral diet capable of meeting energy requirements was formulated using local ingredients (corn flour, soybean flour, powdered milk, soybean oil, whole egg, mineral water, sugar, and cocoa powder). This diet was administered within 48 hours of admission. Nutritional reassessment was performed after seven days of enteral feeding. Data were analyzed using R software and GraphPad.
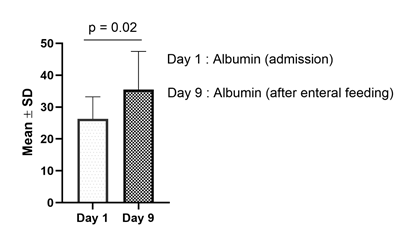
Results: Upon admission, 18%, 13%, and 49% of patients had mild, moderate, and severe protein reserve deficiencies, respectively. Regarding energy reserves, 23% of patients had mild deficiencies, 29% moderate deficiencies, and 22% severe deficiencies. For immune defense loss, the proportions were 3% for mild deficits, 5% for moderate deficits, and 13% for severe deficits. Enteral feeding significantly improved mean albumin concentrations between admission and nutritional reassessment (p = 0.02).
Conclusion: Our formulation provides an effective means of nutritional support for indigent patients in hospital settings.
Keywords
<p>Nutritional management; Food formulation; Enteral feeding; Intensive care; Local ingredients</p>
Article Details
1. Introduction
Malnutrition in hospitalized adult patients is characterized by an insufficient intake of nutrients compared to the body's actual needs. It can result, among other factors, from reduced food absorption or increased metabolic stress [1,2]. Its consequences are numerous: it worsens clinical outcomes, prolongs hospital stays, increases infectious complications, and raises healthcare costs, while also compromising vital prognosis [3].
From an epidemiological perspective, malnutrition affects hospitalized patients worldwide: in Europe, nearly 50% of patients are reportedly affected [4,5]. In Africa, particularly in Cameroon, a study conducted in 2024 at Douala General Hospital found a prevalence of 82.7% of malnutrition among adult patients in intensive care units [6]. This high prevalence in critical care services is explained by the intensity of metabolic stress related to severe illnesses, mechanical ventilation, and surgical interventions, which significantly increase nutritional requirements [7,8].
In this context, several solutions have been proposed to combat malnutrition in intensive care. The American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) recommends the integration of artificial nutrition, particularly enteral nutrition [5]. This approach is considered more physiological, as it preserves intestinal trophicity and limits infectious complications [9,10]. The guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN) confirm the importance of early enteral nutrition in reducing morbidity and mortality [11]. However, the implementation of enteral nutrition often faces repeated interruptions (examinations, digestive intolerances, mechanical issues), leading to nutrient intakes below recommended levels [12].
In Cameroon, the use of enteral formulations based on local products such as maize, soy, or cocoa offers a promising approach adapted to the socio-economic context. These foods, rich in complex carbohydrates, high-quality proteins, and micronutrients, could cover a significant portion of patients' energy and protein needs while remaining financially accessible [6]. Therefore, the objective of this study is to develop and evaluate the effectiveness of an enteral formulation prepared from local ingredients for hospitalized patients in intensive care units.
2. Materials and Methods
2.1 Study Type, Site, and Period
This was a prospective study conducted in the intensive care unit of Laquintinie Hospital in Douala over a period of three months, from April 1 to July 28, 2013.
2.2 Study population
Using a non-probabilistic sampling method, the source population of this study included all patients aged at least 18 years who were admitted to the intensive care unit during the study period and who provided their consent to participate. However, patients with contraindications to enteral nutrition or those able to eat orally were excluded from the study.
2.3 Data collection procedure
Data collection was carried out using a questionnaire that gathered patients’ sociodemographic data, anthropometric measurements, biochemical test results, and clinical evaluations. Additionally, nutritional status assessment was performed through anthropometric measurements (height, ideal weight, mid-upper arm circumference) and biochemical markers analysis (serum albumin, total cholesterol, total lymphocyte count).
Regarding patient nutrition, enteral feeding was administered via bolus through a nasogastric tube, starting 48 hours after admission. The initial feeding phase was characterized by a gradual increase in intake, adjusted according to the degree of malnutrition, the underlying disease, and clinical tolerance. Enteral nutrition was progressively increased in volume and concentration over three days until it reached the required stable intake volume. The nutritional intake was matched to the estimated energy needs for adults.
2.4 Enteral feeding formulation using local ingredients and preparation method
A hypercaloric solution of 1.5 kcal/mL was prepared according to the recipe (Table 1) and the preparation method (Table 2) outlined below.
|
Ingredients |
Quantities |
Measure |
|
Corn flour (Germaïs) |
200g |
2 packets of 100g |
|
Soy flour (Gersoja) |
100g |
1 packet of 100g |
|
Whole milk powder |
45g |
3 tablespoons |
|
Soybean oil |
40g |
3 tablespoons |
|
Whole egg |
180g |
3 medium eggs |
|
Mineral water |
1300g (1.3l) |
|
|
Sugar |
60g |
12 squares |
|
Cocoa powder |
5g |
1 teaspoon |
Table 1: Recipe Composition for 2000 Kcal.
|
Steps |
Procedure to Follow |
|
1 |
Heat 0.5 L of mineral water with 45g of milk powder in a pot for 3 minutes, stirring to obtain a homogeneous mixture |
|
2 |
In a clean bowl, mix 3 whole eggs and 60g of powdered sugar until a homogeneous mixture is obtained. Then, gradually add the required amounts of soy flour and corn flour while stirring vigorously. |
|
3 |
Pour the solution obtained in step 2 into the pot on the heat while stirring to ensure the mixture becomes homogeneous. |
|
4 |
Let the mixture cook over low heat for 5 minutes after adding 40g of soybean oil and a teaspoon of cocoa powder |
|
5 |
Using a fine-mesh sieve, strain the solution for administration. |
Table 2: Preparation Method.
2.5 Ethical considerations and administrative authorizations
The research protocol was submitted to the National Ethics Committee and the University of Douala for approval. Prior authorizations were obtained from the hospital director and the head of the department where the study was conducted. Patients were fully informed about all aspects of the study and were included only after providing their informed consent.
2.6 Statistical analysis
The data were recorded in an Excel spreadsheet and analyzed using R software version 4.4.2 and GraphPad version 8.3.4 for Windows. Qualitative variables were presented as frequencies and percentages, while quantitative variables were expressed as mean ± standard deviation. The Shapiro normality test was performed on all quantitative variables, and the choice of statistical test depended on the distribution of these variables. Fisher’s or Pearson’s chi-square independence tests, as well as the non-parametric Mann-Whitney test, were conducted to compare nutritional status at admission and after enteral feeding. For these tests, the confidence interval for the null hypothesis was set at 95%, and the margin of error was 5% (the p-value was considered significant if and only if it was less than 0.05).
3. Results
3.1 Sociodemographic characteristics and medical history
The average age of participants was 47.16 ± 1.98 years. The majority of participants were male (68%), while females represented 32%. Regarding occupations, 43% were unemployed, 39% were self-employed, 9% were salaried workers, 5% were farmers, and 4% were students. In terms of medical history, 38% of participants had infections or a septic condition, 26% had suffered polytrauma, 25% had a history of stroke (cerebrovascular accident - CVA), and 12% had other conditions such as diabetes or cancer (Table 3).
|
Sociodemagraphics factors |
Frequency (n) |
Percentage (%) |
|
Mean age (years) |
47.16 ± 1.98 |
|
|
Gender |
||
|
Male |
52 |
68 |
|
Female |
25 |
32 |
|
Occupations |
||
|
Unemployed |
33 |
43 |
|
Self-employed |
30 |
39 |
|
Salaried |
7 |
9 |
|
Farmer |
4 |
5 |
|
Student |
3 |
4 |
|
Medical history |
||
|
Septic state/Infectious disease |
29 |
38 |
|
Polytrauma |
20 |
26 |
|
Stroke (CVA) |
19 |
25 |
|
Others (diabetes, cancer) |
9 |
12 |
Table 3: Sociodemographic Characteristics of the Study Population.
|
Evaluated Markers |
|||
|
Nutritional Deficit |
Protein Reserves Loss n(%) |
Energy Reserves Loss n(%) |
Immune Defense Loss n(%) |
|
No Deficit |
15 (19%) |
19 (25%) |
62 (81%) |
|
Mild |
14 (18%) |
18 (23%) |
2 (3%) |
|
Moderate |
10 (13%) |
22 (29%) |
4 (5%) |
|
Severe |
38 (49%) |
17 (22%) |
10 (13%) |
|
P-value |
<0.001*** |
<0.001*** |
<0.001*** |
|
The data are presented as frequencies (n) and percentages (%). P-value: The Pearson Chi-Square Test was performed to compare the proportions of different categories of nutritional deficits for each marker. The confidence interval for the null hypothesis of this test was set at 95%, and the margin of error at 5% (p is significant if p < 0.05). |
|||
Table 4: Distribution of Nutritional Deficiency Markers.
3.2 Assessment of nutritional deficiency at admission
Regarding the loss of protein reserves, 19% of patients had no deficiency, while 18%, 13%, and 49% had mild, moderate, and severe deficiencies, respectively. For the loss of energy reserves, 25% of patients had no deficiency, whereas 23%, 29%, and 22% exhibited mild, moderate, and severe deficiencies, respectively. Concerning the loss of immune defense, 81% of patients showed no deficiency, while 3%, 5%, and 13% had mild, moderate, and severe deficiencies, respectively. The Chi-square test revealed a statistically significant difference for each of the evaluated markers (p < 0.001).
3.3 Assessment of Patients' Nutritional Status After Enteral Feeding
We observed a significant increase in the mean albumin concentration from admission to the post-enteral feeding period (P = 0.02), reflecting an improvement in the nutritional status of patients after enteral feeding (Figure 1).
4. Discussion
The results of our study highlight the significant prevalence of nutritional deficiencies among adult patients admitted to intensive care. Upon admission, nearly half of the patients presented with severe protein deficiency, and more than one-fifth had severe energy deficiency. These findings align with previous studies showing that critically ill patients are particularly vulnerable to nutritional imbalances, primarily due to disease-related hypercatabolism and reduced food intake [2,13]. Metabolic stress, dependence on mechanical ventilation, and multiple examinations and interventions can further delay the initiation of enteral nutrition, exacerbating the situation. In this context, the presence of immune deficiency in some patients (up to 13% severe cases) is not surprising, as protein and micronutrient deficiencies directly impair immune response and increase infection risk [8].
The significant improvement in albumin levels observed after seven days of nutritional management demonstrates the effectiveness of the proposed enteral formulation. Although albumin is an imperfect indicator, as it is sensitive to inflammation and hydration status, its elevation remains an encouraging sign of improved protein intake coverage [14]. The approach adopted, based on the use of local ingredients (maize, soy, eggs, cocoa, etc.), offers several advantages. It ensures adequate energy and protein intake at a moderate cost while considering the dietary habits of the local population. This strategy aligns with scientific society recommendations, which emphasize adapting nutritional management to available resources to maintain intestinal trophicity and prevent infectious complications [11,15].
From a clinical perspective, the systematic implementation of such a formulation within 48 hours of admission could help reduce infectious morbidity and hospital stay duration, as suggested by other studies demonstrating the positive impact of early enteral nutrition [16]. However, certain limitations of the study must be considered. The relatively small sample size (77 patients) and the short follow-up period of only seven days do not allow for a comprehensive assessment of long-term outcomes or for establishing a direct link with robust clinical endpoints such as mortality or mechanical ventilation duration. Additionally, the heterogeneity of pathologies encountered in intensive care (trauma, sepsis, organ failure) may influence the consistency of the results. The inflammatory state, characteristic of the critical phase, is also a major confounding factor when interpreting biological markers such as albumin.
Despite these limitations, the present study provides important insights for clinical practice in Cameroon. It demonstrates that the use of an affordable enteral formulation made from local ingredients can significantly improve the nutritional status of patients. Moving forward, it would be relevant to expand the patient sample, extend the follow-up duration, and measure additional biological parameters (such as prealbumin, C-reactive protein (CRP), or transferrin) to refine the evaluation of the nutritional and clinical impact. Such an initiative would fit into a public health strategy aimed at reducing hospital malnutrition prevalence in intensive care units and improving the prognosis of these highly vulnerable patients.
5. Conclusion
Our study illustrates the importance of early detection and treatment of malnutrition in adult intensive care patients. The enteral formulation based on local ingredients, initiated within 48 hours of admission, resulted in a significant improvement in protein reserves, as evidenced by the increase in albumin levels. The observed benefits—economic accessibility, availability, and adequate nutritional intake—suggest that this enteral feeding protocol could be integrated into national recommendations for the management of critically ill patients in Cameroon. Further research, including a larger sample size and a longer follow-up period, will be necessary to better assess the long-term impact of this approach on morbidity, mortality, and patient quality of life.
6. Ethical Approval and Consent to Participate
Studies involving human participants were reviewed and approved by the National Ethics Committee for Health Research and the Institutional Ethics Committee of the University of Douala. Written informed consent to participate in this study was obtained from the legal guardian/closest relative of the participants.
Data Availability
The raw data supporting the conclusions of this article will be made available by the authors without any undue restrictions.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
The authors confirm that this research was conducted without any external funding.
References
- Soeters PB, Reijven PLM, van Bokhorst-de van der Schueren MAE, et al. A rational approach to nutritional assessment. Clin Nutr 27 (2008): 706-16.
- DiMaria-Ghalili RA. Changes in Nutritional Status and Postoperative Outcomes in Elderly CABG Patients. Biol Res Nurs 4 (2002): 73-84.
- Cynober L. Nutritional support at the hospital: diagnosis of malnutrition and its associated risks for better prevention and treatment. Bull Acad Natl Med 195 (2011): 645-56.
- Kyle UG, Schneider SM, Pirlich M, et al. Does nutritional risk, as assessed by Nutritional Risk Index, increase during hospital stay? A multinational population-based study. Clin Nutr Edinb Scotl 24 (2005): 516-24.
- Kyle UG, Pirlich M, Lochs H, et al. Increased length of hospital stay in underweight and overweight patients at hospital admission: a controlled population study. Clin Nutr Edinb Scotl 24 (2005): 133-42.
- Nga WTB, Bengono JAM, Roger NNG, et al. Prevalence and clinical and para-clinical aspects of malnutrition in the medical-surgical care unit: A case series from Douala General Hospital in Cameroon. Ann Afr Med 17 (2024): e5660-7.
- Kyle UG, Genton L, Heidegger CP, et al. Hospitalized mechanically ventilated patients are at higher risk of enteral underfeeding than non-ventilated patients. Clin Nutr Edinb Scotl 25 (2006): 727-35.
- Giner M, Laviano A, Meguid MM, et al. In 1995 a correlation between malnutrition and poor outcome in critically ill patients still exists. Nutr Burbank Los Angel Cty Calif 12 (1996): 23-9.
- Lewis SJ, Egger M, Sylvester PA, et al. Early enteral feeding versus ‘nil by mouth’ after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ 323 (2001): 773-6.
- G N, R C, X L. Nutrition artificielle de l’adulte en reanimation. Reanimation 6 (2002): 450.
- Kreymann KG, Berger MM, Deutz NEP, et al. ESPEN Guidelines on Enteral Nutrition: Intensive care. Clin Nutr Edinb Scotl 25 (2006): 210-23.
- McClave SA, Sexton LK, Spain DA, et al. Enteral tube feeding in the intensive care unit: factors impeding adequate delivery. Crit Care Med 27 (1999): 1252-6.
- Soeters PB, Reijven PLM, van Bokhorst-de van der Schueren MAE, et al. A rational approach to nutritional assessment. Clin Nutr Edinb Scotl 27 (2008): 706-16.
- Hébuterne X, Filippi J, Schneider SM. Nutrition entérale: techniques. In: Cano N, Barnoud D, Schneider SM, Vasson MP, Hasselmann M, Leverve X, editors. Traité de nutrition artificielle de l’adulte. Paris: Springer (2007): pp: 567-80.
- Fuhrman MP, Winkler M, Biesemeier C, et al. The American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Standards of Practice for nutrition support dietitians. J Am Diet Assoc 101 (2001): 825-32.
- Lewis SJ, Egger M, Sylvester PA, et al. Early enteral feeding versus ‘nil by mouth’ after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ 323 (2001): 773-6.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 