Massive Subcutaneous Emphysema and Bilateral Pneumothorax after TISSEEL Spray in Laparoscopic Surgery
Weu-Che Hsu1*, Yu-Ting Lin2
1Anesthesia department, Chung Shan Medical University and Hospital, Taichung, Taiwan
2Chung Shan Medical University and Hospital, Taichung, Taiwan
*Corresponding Author: Dr. Weu-Che Hsu, Anesthesia Department, Chung Shan Medical University and Hospital, Taichung, Taiwan
Received: 22 October 2019; Accepted: 08 November 2019; Published: 12 November 2019
Article Information
Citation: Weu-Che Hsu, Yu-Ting Lin. Massive Subcutaneous Emphysema and Bilateral Pneumothorax after TISSEEL Spray in Laparoscopic Surgery. Anesthesia and Critical Care 1 (2019): 37-38.
View / Download Pdf Share at FacebookKeywords
Massive Subcutaneous Emphysema; Laparoscopic Surgery
Laparoscopic Surgery articles Laparoscopic Surgery Research articles Laparoscopic Surgery review articles Laparoscopic Surgery PubMed articles Laparoscopic Surgery PubMed Central articles Laparoscopic Surgery 2023 articles Laparoscopic Surgery 2024 articles Laparoscopic Surgery Scopus articles Laparoscopic Surgery impact factor journals Laparoscopic Surgery Scopus journals Laparoscopic Surgery PubMed journals Laparoscopic Surgery medical journals Laparoscopic Surgery free journals Laparoscopic Surgery best journals Laparoscopic Surgery top journals Laparoscopic Surgery free medical journals Laparoscopic Surgery famous journals Laparoscopic Surgery Google Scholar indexed journals Massive Subcutaneous Emphysema articles Massive Subcutaneous Emphysema Research articles Massive Subcutaneous Emphysema review articles Massive Subcutaneous Emphysema PubMed articles Massive Subcutaneous Emphysema PubMed Central articles Massive Subcutaneous Emphysema 2023 articles Massive Subcutaneous Emphysema 2024 articles Massive Subcutaneous Emphysema Scopus articles Massive Subcutaneous Emphysema impact factor journals Massive Subcutaneous Emphysema Scopus journals Massive Subcutaneous Emphysema PubMed journals Massive Subcutaneous Emphysema medical journals Massive Subcutaneous Emphysema free journals Massive Subcutaneous Emphysema best journals Massive Subcutaneous Emphysema top journals Massive Subcutaneous Emphysema free medical journals Massive Subcutaneous Emphysema famous journals Massive Subcutaneous Emphysema Google Scholar indexed journals TISSEEL Spray articles TISSEEL Spray Research articles TISSEEL Spray review articles TISSEEL Spray PubMed articles TISSEEL Spray PubMed Central articles TISSEEL Spray 2023 articles TISSEEL Spray 2024 articles TISSEEL Spray Scopus articles TISSEEL Spray impact factor journals TISSEEL Spray Scopus journals TISSEEL Spray PubMed journals TISSEEL Spray medical journals TISSEEL Spray free journals TISSEEL Spray best journals TISSEEL Spray top journals TISSEEL Spray free medical journals TISSEEL Spray famous journals TISSEEL Spray Google Scholar indexed journals
Article Details
1. Case Report
A 33 years old female without systemic disease received laparoscopic ovarian cystectomy and chromotubation. The operation time was 60 minutes. During the surgery, the intraabdominal pressure was limited between 12 and 15 mm Hg. The ETCO2 was about 35 mmHg and the airway pressure was about 22 cm H2O. At the end of operation, TISSEEL [Fibrin Sealant] was delivered by TISSEEL spray set with piped air. The intraabdominal pressure suddenly rose above 20 mmHg, and the peek airway pressure exceeded 40 mmHg. Massive emphysema extending to the face and neck were noted, and bilateral pneumothorax were also found (Figure 1) There were some petechia over her chest. She was transferred to SICU and the condition was relatively stable. She was discharged uneventually after one week.
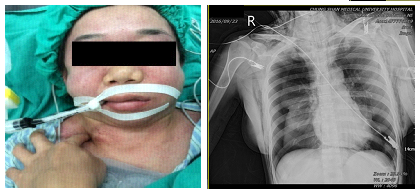
Figure 1: Massive emphysema extending to the face and neck.
2. Discussion
Subcutaneous emphysema, and pneumothorax are documented complications of laparoscopic techniques. Murdock et al. found incidence rates of 2.3% for significant subcutaneous emphysema, and 1.9% for pneumothorax/ pneumomediastinum following laparoscopic approach [1]. Asymptom subcutaneous emphysema can even be detected in up to 56% cases received laparoscopic surgery [2]. The risk factors for subcutaneous emphysema are improperly placed trocar, surgical time longer than 200 minutes, six or more surgical ports, and high intraabdominal pressure [3]. Hypercarbia was noted due to increased CO2 absorption from the subcutaneous layer. Usually, it will resolves spontaneously with conservative treatment and oxygen therapy.
Pneumothorax is a rare but much vital complication during laparoscopic surgery. It may occur in case of barotrauma from positive pressure mechanical ventilation, direct injury to the diaphragm, defects of the diaphragm, congenital weak points of the diaphragm, or through anatomical pathways, i.e. aortic and esophageal hiatuses of the diaphragm [4]. Increased airway pressure and end tidal CO2, unexplained hypoxia, hypercarbia, or hemodynamic instability may ensue [5].
In our case, misuse of TISSEEL spray set leaded to an abrupt increase in abdominal pressure. It caused barotrauma and thence severe pneumothorax. In order to avoid complications, tightly following device instruction is needed. Close monitoring the change of intra-abdominal and airway pressure could help us to detect the development of pneumothorax earlier. In conclusion, we should always beware of the possibility of serious complications like this case during or after the laparoscopic surgery.
References
- Murdock CM, Wolff AJ, Van Geem T. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax, and pneumomediastinum during laparoscopy. Obstet Gynecol 95 (2000): 704-709.
- McAllister JD, D’Altorio RA, Snyder A. CT findings afteruncomplicated percutaneous laparoscopic cholecystectomy. J Comput Assist Tomogr 15 (1991): 770-772.
- Murdock CM, Wolff AJ, Van Geem T. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax, and pneumomediastinum during laparoscopy. Obstet Gynecol 95 (2000): 704-709.
- Mami? I, Danoli? D, Puljiz M, et al. Pneumithorax and pneumomediastinum as a rare complication of laparoscopic surgery. Acta Clin Croat 55 (2016): 501-504.
- Machairiotis N, Kougioumtzi I, Dryllis G, et al. Laparoscopy inducedpneumothorax. J Thorac Dis 6 (2014): 404-406.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 