Mortality of Immediate Postpartum Hemorrahges in the University Clinic of Anesthesia and Intensive Care at the National University Hospital Hubert Koutoukou Maga (CNHU-HKM) of Cotonou-Benin
Hounkpè Pierre Claver1*, Aboukari Baoua Mahamadou2, Houénon Martin Semevo1, Oke Luc3, Chobli Martin4
1Anesthesia and Critical Care Service, National University Hospital Hubert Koutoukou Maga (CNHU-HKM) of Cotonou-Benin Republic
2Anesthesia resuscitation service of the Niamey National Hospital Niamey-Niger
3Heart consultants, Howard University College of medicine department of physiology, 520 W st NW Washington DC 20059, 8630 Fenton suite 720 Silver Spring MD 20910 USA
4Anesthesia resuscitation department, Faculty of Health Sciences, University of Abomey-Calavi, Benin Republic
*Corresponding Author: Hounkpè Pierre Claver, Anesthesia and Critical Care Service, National University Hospital Hubert Koutoukou Maga (CNHU-HKM) of Cotonou-Benin Republic
Received: 16 January 2022; Accepted: 21 January 2022; Published: 11 February 2022
Article Information
Citation: Hounkpè Pierre Claver, Aboukari Baoua Mahamadou, Houénon Martin Semevo, Oke Luc, Chobli Martin. Mortality of Immediate Postpartum Hemorrahges in the University Clinic of Anesthesia and Intensive Care at the National University Hospital Hubert Koutoukou Maga (CNHU-HKM) of Cotonou-Benin. Anesthesia and Critical Care 4 (2022): 33-42.
View / Download Pdf Share at FacebookAbstract
Introduction
Obstetric hemorrhage remains the leading cause of maternal mortality worldwide, both in developed and resource-limited developing countries. The aim of this study was to determine the etiologies of immediate postpartum hemorrhages in relation to the mortality.
Materials and methods
This was a descriptive and analytical retrospective study on immediate postpartum hemorrhage (PPH) in the intensive care unit of the National University Hospital Hubert Koutoukou Maga(CNHU-HKM) of Cotonou.
Results
A total of 37 cases of immediate PPH were collected during the study period. The mean age of the patients was 25 years with a predominance of the age group of 20-30 years. The main etiologies were uterine atony, coagulopathy, soft tissue tears, uterine rupture and placental retention. Mortality was heavy at 37.87%.
Conclusion
The development and implementation of an adequate management protocol will significantly reduce this mortality.
Keywords
<p>Immediate PPH, Epidemiology, Etiologies, Uterine atony, Mortality, Management protocol implementation</p>
Article Details
1. Introduction
Obstetric hemorrhages remain a leading cause of maternal mortality worldwide, in both developed and resource-limited countries. They are the cause of at least 50% of the 500,000 maternal deaths estimated each year in the world [1]. These hemorrhages include antepartum and postpartum bleeding. Postpartum hemorrhage (PPH) complicates 5% of all deliveries and is the consequence of one or a combination of the four following main processes: uterine atony, placental retention, lesions of the genital tract or even coagulation disorders [2,3]. In France, from 2007 to 2009, the maternal mortality rate was 10.3 per 100,000 live births [4]. Obstetric hemorrhages were the leading direct causes of mortality and represented 18% of deaths, followed by pulmonary embolisms (11%) and complications from hypertension (9%). Among the deaths related to obstetric hemorrhages, the percentage of PPH, even if it has halved, still represented 8% of deaths (1.9/100,000) versus 16% (2.5/100,000) in 2004-2006 [5]. In Benin republic, a 2006 Demographic Health Survey leaded by the ministry of health [6] showed 397 maternal deaths for 100,000 live births versus 498 in 1996. The aim of the authors was to assess the etiologies of immediate postpartum hemorrhages in relation to the mortality.
2. Materials and Methods
2.1. Type nature and period of study.
It was a descriptive and analytical retrospective study running from January 2012 through December 2018 on immediate postpartum hemorrhages in the intensive care unit of the Hubert Koutoukou Maga national university teaching hospital (CNHU-HKM) of Cotonou.
2.2. Study population
All women who have given birth at the hospital clinic of gynecology and obstetrics(CUGO) and those from other health facilities admitted to intensive care of the university clinic of anesthesia and critical care(CUPAR) for hemorrhage occurring in the immediate postpartum period, for all causes and every age from January 2012 to December 2018.
2.2.1 Inclusion criteria: The inclusion criteria were:
- Admission to CUPAR from January 2012 to December
- Single or multifetal
- Significant blood loss, quantified or not, during delivery or the 24 hours following childbirth, whether or not
Non-inclusion criteria: Is as below
- Any bleeding that occurs after the 24 hours following
- Any shock from extra genital
2.3. Data collection source
To collect the cases of our study population, we used:
- Hospitalization registers;
- The files of patients hospitalized in the anesthesia and intensive care clinic (CUPAR).
Data collection methods: For the data collection, we proceeded by steps:
- First, we consulted the CUPAR hospitalization registers for listing all cases of immediate postpartum
- Secondly, we used all the files found in the archives, according to the study period. The information collected was then transferred to the data collection sheets developed for this Patients whose diagnosis of immediate postpartum hemorrhage was not confirmed after hospitalization were not taken into account.
Data processing tools: Data collected was processed and organized into simple and crossed tables by Epi-info software version 7 and Microsoft Excel
2.4. Ethical consideration
The study was carried out in the confidentiality of patients identity.
Strict security measures have been applied to ensure this confidentiality.
2.5. Difficulties encountered
- Several patient files were not
- Some files were unusable because the record were incomplete or in poor
3. Results
3.1. Sociodemographic characteristics
Prevalence: 37 cases of immediate PPH were collected during the study period among 4627
patients admitted in intensive care, that corresponds to a prevalence of 0.8%.
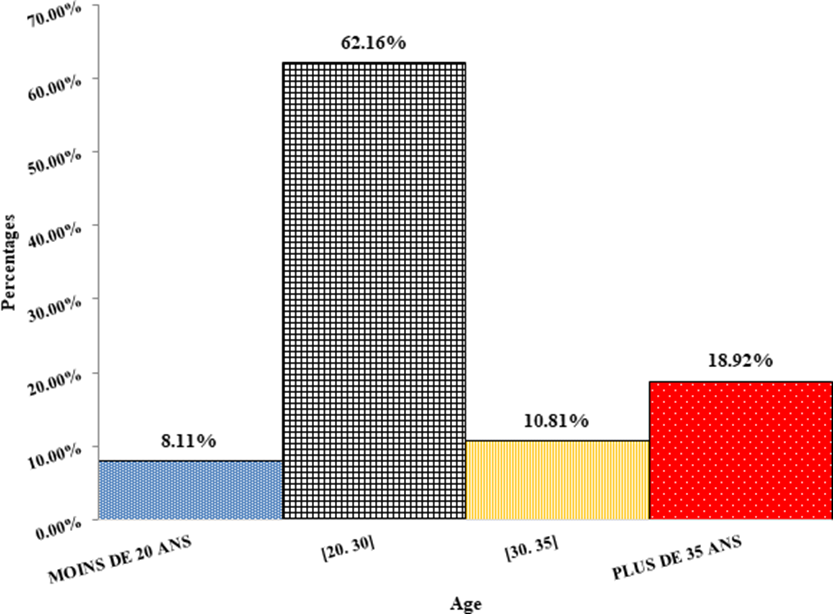
Age: The mean age was 25 years and the age group of 20 to 30 years represented 62.16% (Figure 1).
Depending on the level of education, out-of-school women represented 64.86%. As for the profession, the retailers and housewives were respectively 27.03% and 24.32%.
3.2. Clinical data
Type of delivery: the women having benefited from a directed delivery represented 62.16% and the ones from artificial deliveries were 35.14%.
Hemorrhagic shock: it was present in 35% of childbirth and absent in 60%.
State of consciousness on admission: 26 women (70.27%) had altered consciousness on admission.
3.3. Etiologic data
Etiologies: Table 1 shows that uterine atony was the leading cause of PPH with 24.32%. It was followed by mixed etiologies 18.92%, coagulopathies 16.22%, tears of the soft tissue 13.51%, uterine rupture and placental retention 8.11% for each one.
3.4. Evolution
The mortality rate was 37.84% which corresponds to 14 cases. Table 2 shows the prognosis relative to etiologies.
Table 3 shows the prognosis realative to delivery mode. Mortality rate is higher in vaginal delivery than in caesarean section.
|
Size |
Percentage (%) |
|
|
Uterine atony |
9 |
24,32 |
|
Mixte etiology |
7 |
18,92 |
|
Coagulopathy |
6 |
16,22 |
|
Tears of soft tissue |
5 |
13,51 |
|
Uterine rupture |
3 |
8,11 |
|
Placental retention |
3 |
8,11 |
|
RPH |
2 |
5,41 |
|
Unspecified |
1 |
2,70 |
|
Placenta previa |
1 |
2,70 |
|
Total |
37 |
100,00 |
Table 1: Etiologies of immediate PPH in intensive care at CNHU-HKM of Cotonou
|
Cured |
Deceased |
Total |
|
|
Uterine atony |
6 |
3 |
9 |
|
Uterine atony and tears tissue |
1 |
1 |
2 |
|
Uterine atony and placental retention |
2 |
0 |
2 |
|
Coagulopathy |
1 |
5 |
6 |
|
Tears of soft tissue |
4 |
1 |
5 |
|
RPH |
2 |
0 |
2 |
|
Unspecified |
0 |
1 |
1 |
|
Placenta previa |
1 |
0 |
1 |
|
Placenta previa and Coagulopathy |
1 |
0 |
1 |
|
Placental retention |
2 |
1 |
3 |
|
Uterine rupture |
3 |
0 |
3 |
|
Uterine rupture and Coagulopathy |
0 |
1 |
1 |
|
Uterine rupture and tears of soft tissue |
0 |
1 |
1 |
|
Total |
23 |
14 |
37 |
Table 2: Maternal prognosis of immediate PPH in intensive care at CNHU-HKM of Cotonou relative to etiology
|
Cured |
Deceased |
Total |
|
|
Caesarean section |
10 |
1 |
11 |
|
Vaginal delivery |
13 |
13 |
26 |
|
Total |
23 |
14 |
37 |
Table 3: Maternal prognosis relative to delivery mode at CNHU-HKM of Cotonou
4. Discussion
4.1. Sociodemographic characteristics
Prevalence: The prevalence of 0.8% is lower than many others. In Benin, de SOUZA got 2.25%, BAËTA et al got 6.89% in Togo [7], in Cameroon SANGO got in 2008 a prevalence of 1.68%. In France, MERCIER published in 2016 a prevalence of 5% for bleeding less than 500 ml and 2% for severe PPH [8].
Age: With the age of 25 years, our patients are younger than those of the series of LAINI whose mean age is 33 years [9]. This age is close to those of DUCARME and TARIK [10,11] who found 33.2 and 31 years respectively. The most interested age group in our series is 20-30 years old and constitutes 62.16%. This slice is younger in comparison to the series of LAINI [9] where the patients were aged 31- 40 years and constituted 57%.
4.2. Clinical data
In our series, most of the immediate PPH occurred during a directed delivery in a proportion of 62.16% versus 31.14% during an artificial delivery. These figures are higher than those of GANI KARATCHI series which found the proportions of 37.01% and 19.06% respectively.
4.3. Etiologic data
Uterine atony is the most common cause of immediate PPH with 24.32%. The following authors also found uterine atony at the top of the etiologies. They are SANGO [12], DREYFUS [13], REYAL et al [14], NNADI [15], DUCARME [16] and
AKPADZA [17]. In difference to the results of the above-mentioned authors, GANI KARATCHI [18] rather found placental retention in first place which corresponds to 48.07%. For MERCIER, placenta previa was found at the top of the series [19].
Immediate PPH and maternal vital prognosis The mortality in our group was high: 87% (n = 14). Thirteen of the women had given birth vaginally versus only one who benefited from caesarean section. Nine of the deceased postpartum hemorrhages were complicated by shock. Six of the deceased patients presented a coagulopathy (16,22%), four with uterine atony and three with torn soft tissue. OSSE L [3] in his article on obstetric haemorrhages mentions: among the deaths due to obstetric haemorrhages, the percentage of PPH, even if it has halved, still represented 8% of deaths (1.9/100 000) versus 16% (2.5/100,000) in 2004- 2006 [5]. LAINI MC [11] found a mortality of 28.57%. MAHAMADOU B [20], during his study recorded 13.9% of deaths or 19 cases out of 137 cases. This death rate remains high in other reported studies: BAYO AI [21] reports 3 out of 7 deaths as a result of severe obstetric haemorrhages, 57.11% in a study on uterine ruptures. DIALLO MS et al [22] found 58.4%. ABDULLAH SA et al [23] revealed 31.5%. LEKE RJ [24] found 58.4%. This rate difference could be explained by the management improvement of obstetric complications in Mali as part of the national policy to control maternal mortality. The high mortality could be explained by the delay in referral, poor evacuation conditions, shortage of blood and its derivatives especially fresh frozen plasma and red blood cells. DENEUX-THARAUX C et al. argue in one of its articles [25] that uterine atony is the main cause of PPH. According to the same article, maternal mortality from obstetric hemorrhage has decreased in France (currently 1.6 deaths/100,000 live births), but it remains the leading cause of maternal death (16%), and the most preventable (80%); in developed countries as a whole, PPH is the leading cause of severe acute maternal morbidity and ICU admission in pregnant women. The main risk factors for PPH are uterine atony factors, but overall they are not very predictive. M. SAUCEDO [5] in his epidemiological survey on maternal mortality in France states: “From 2007 to 2009, 254 maternal deaths were identified, bearing the maternal mortality rate to 10.3 per 100,000 live births. Maternal age of death is associated with mortality. Hemorrhages occupy the first place; their rate is 1.9 per 100,000 births, compared to 2.5 previously; this decrease is due to the decrease in deaths from hemorrhages due to uterine atony. Suboptimal care remains frequent, 60% of all deaths, slightly declining and the frequency of maternal mortality is generally stable. That reduction seems possible since progress has been done in reduction deaths of hemorrhage from uterine atony and reduction in suboptimal care". LAIDI BN et al. [26], in the Anesthesia-Resuscitation Service, at the Faculty of Medicine of Tunis (Tunis El Manar University) affirmed: the annual rate of death by PPH in our unit varies between 2.4 and 6.3%; at the Maternity and Neonatal Center in Tunis, severe peripartum hemorrhage is the second leading cause of maternal mortality (28.1%) after sepsis; in our series, a statistically significant association was found between the occurrence of death and massive transfusion, the use of catecholamines, the occurrence of acute renal failure requiring hemodialysis, sepsis, disseminated intravascular coagulation (DIC), acute pulmonary edema , multiple organ failure, shock, and severe neurological impairment. Few studies have looked for predictive complications of maternal mortality following the management of severe PPH in intensive care. AGBESSY et al found a mortality rate of 28.85% in 1990 in Benin [27] while ADETORO got 33.5% in Nigeria in 1992 [28]. PAMBOU et al had found 39.53% in 1996 in Congo [29] while DUCARME et al had found any deceased during surgical treatment of PPH [18]. SHAISTA et al. found in 2009 a PPH mortality rate of 9.4% [30], higher than WAFA in 2011 in Marrakech [31] who found 8.3% and lower
than LAINI 2017 in Morocco with 18,9% [11].
5. Conclusion
Mortality due to PPH is high in the university clinic of anesthesia and intensive care of the national university teaching hospital (CNHU-HKM) of Cotonou. The main etiologies are uterine atony, coagulopathy, soft tissue tears, uterine rupture and placental retention. The development and implementation of an adequate management protocol will significantly reduce this mortality.
References
- Cantwell R, Clutton-Brock T, Cooper Saving mothers' lives: reviewing maternal deaths to make motherhood safer: 2006- 2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom BJOG 118 (2011): 1-203.
- Royal college of Obstetricians and Antepartum haemorrhage. Green-top guidelines (2011) 63.
- Sentilhes L, Vayssiere C, Mercier Postpartum hemorrhage: guidelines for clinical practice - text of the guidelines (short text). J Gynecol Obstet Biol Reprod 43 (2014): 1170-1179.
- Ossé L, Nebout S, Filippov J, et Hémorragies obstétricales. EMC - Anesthésie-Réanimation 14 (2017): 1-7.
- Saucedo M, Deneux-Tharaux C, Bouvier- Colle Maternal mortality in France, 2007-2009 J Gynecol Obstet Biol Reprod 42 (2013): 613-627.
- Ministère de la sante; Service de Statistique de la documentation et de la recherche opérationnelle; Statistiques sanitaires année (2006).
- .Baëta S, Kolani K, Nyame AT, et al. Prise en charge des hémorragies du postpartum immédiat au H.U. Tokoin [Mémoire Méd.]. CHU Tokoin; Bamako/Mali. (2003)
- Mercier Hémorragie du post-partum (HPP): stratégie de prise en charge en 2016. CNGOF 33 (2005): 268-274.
- Sitti Prévention et prise en charge de l’hémorragie du post-partum au CHU Sylvanus Olympio de Lomé au Togo. Gynécologie et obstétrique (2014).
- Faye dieme ME, Gassama O, Diouf AA, et Prise en charge et pronostic des hémorragies du post-partum immédiat dans un centre de santé de niveau II de dakar (Sénégal). Journal de la SAGO 18 (2017): 27-34.
- Laini MC. Les hémorragies du postpartum prise en charge en réanimation [Mémoire de Spécialisation en anesthésie réanimation]. Université Sidi Mohamed Ben Faculté de médecine et de pharmacie du Maroc (2017)
- Tarik Y. Maternal and perinatal outcome of massive postpartum hemorrhage. A review of 33 cases. Ann Saudi Med 23 (2003): 135-
- Dreyfus M, Beucher G, Mignon A, et Prise en charge obstétricale initiale en cas d'hémorragie du postpartum Immédiat In J. Gynécol Obst Biol Reprod 33 (2004): 4S103-4S119.
- Gani Hémorragies du post-partum immédiat: facteurs de risque, qualité de la prise en charge et pronostic maternel. [Thèse de doctorat] Cotonou: Université d’Abomey-Calavi- Faculté des Sciences de la Santé (2009).
- Reyal F, Deffarge J, Luton D, et Hémorragie grave du postpartum. Etude descriptive à la maternité de Hopital Robert-Debre. J Gynécol obstét Biol Reprod 31 (2002): 358-364.
- Atrede LR, Nnadi DC. The of the condom- catheter foor the treatment of postpartum The sokoto experience. Trop Doct. 38 (2008): 84-86.
- Akpadza K, Kotor K, Baeta S, et al. Les hémorragies de la délivrance à la clinique de gynécologie obstétrique de CHU Tokoin- Lomé (TOGO) de 1988-1992.
- Ducarme G, Bargy S, Grossettia B, et al. Prise en charge chirurgicale de l’hémorragie de la délivrance. Gynecol Obstet Fertil Senol 35 (2007): 1209-1214.
- Mercier FJ, Van de velde Major Obstetric Hemorrhage. Am Anesthesiol Clin. 26 (2008): 53-66.
- Mahamadou Hémorragies obstétricales graves: prise en charge anesthésiologique au CHU du point G Bamako (Mali). [Thèse de doctorat] Bamako: Université des Sciences, des Techniques et des TechnologiesFaculté de médecine et d’odontostomatologie (2014): 104.
- Bayo AI. Les ruptures utérines à propos de 58 cas recensés à l’hôpital Gabriel Touré. [Thèse de doctorat] Bamako: Ecole de médecine et de pharmacie du Mali (1991):
- Diallo MS, Sidibe M, Keita [Maternal mortality. Apropos of 212 instances in 7 years (1980-1986) at the Ignace-Deen Maternity Hospital in Conakry (Guinea)]. Rev Fr Gynecol Obstet 84 (1989): 419-422.
- Abdullah SA, Fathalla MF, Abdel AAM, et Maternal mortality in upper Egypt. Paper presented at the WHO Inter-regional meeting on prevention of maternal mortality; Geneva, November (1985): 11-15.
- Leke Outcome pregnancy and delivery at the central maternity of the center hospital of Yaoundé. Ann Univ Santé Yaoundé 4 (1984): 322-330.
- Jean Prise en charge de l’hémorragie grave du postpartum. Impact des recommandations nationales de 2004 dans une maternité de niveau II. [Thèse de doctorat] Nancy: université Henri Poincare- Faculté de médecine (2011): 109.
- Laidi BN, Sofiene BM, Mehdi K, et L'hemorragie grave du peripartum en milieu de reanimation dans un centre universitaire tunisien de niveau 3: épidémiologie et facteurs de risque de mortalité maternelle. Pan Afr Med J. 21 (2015): 277.
- Agbessy, Alihonou E. Les hémorragies de la délivrance: étude statistique et étiologique (à propos de 151 cas recensés en 5 ans). Publications Médicales Africaines 2 (1990):
- Adetoro Primary post-partum heamorrhage at a university in Nigeria. West Afr J Med 11 (1992): 172-178.
- Pambou O, Ekoundzola JR, Yoca G, et al. Les hémorragies graves de la délivrance au CHU de Médecine d'Afrique Noire 43 (1997): 418-422.
- Shaista T, Kashif F, Shaikh S, Baloch Postpartum haemorrhage-a major killer of mothers Gynae Obstetrics 15 (2009): 4.
- Wafa Les hémorragies graves de la délivrance étude rétrospective à propos de 72 cas. [Thèse de doctorat] Marrakech: Université Cadi AyyadFaculté de médecine et de pharmacie (2011).


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 