The Evolution and Global Impact of Pulse Oximetry: From Innovation to Standard of Care - A Comprehensive Review for Anesthesiologists and Critical Care Physicians
Michiaki Yamakage MD, PhD1*
Professor & Chair, Department of Anesthesiology, Sapporo Medical University School of Medicine, South 1, West 16, 291, Chuo-ku, Sapporo, Hokkaido 060-8543, Japan
*Corresponding Author: Michiaki Yamakage, Professor & Chair, Department of Anesthesiology, Sapporo Medical University School of Medicine, South 1, West 16, 291, Chuo-ku, Sapporo, Hokkaido 060-8543, Japan.
Received: 02 October 2025; Accepted: 04 November 2025; Published: 25 November 2025
Article Information
Citation: Michiaki Yamakage. The Evolution and Global Impact of Pulse Oximetry: From Innovation to Standard of Care - A Comprehensive Review for Anesthesiologists and Critical Care Physicians. Anesthesia and Critical care. 7 (2025): 122-132.
View / Download Pdf Share at FacebookAbstract
This review examines the evolution, clinical applications, and global impact of pulse oximetry, with emphasis on its transformative role in anesthesiology and critical care medicine. Technological advancements, clinical evidence, limitations, and future directions—including educational uses, quality improvement initiatives, and implementation science - are discussed in detail.
A comprehensive literature review of PubMed, MEDLINE, and Cochrane databases (1970–2024) was conducted using terms such as “pulse oximetry,” “oxygen saturation monitoring,” “perioperative monitoring,” and “anesthesia safety.” Industrial patents, regulatory documents, and international guidelines from organizations including the WHO, ASA, and ESA were reviewed. Clinical case studies from major medical centers and quality improvement data were analyzed to highlight real-world benefits.
Since its introduction in the early 1980s, pulse oximetry has progressed from basic analog instruments to sophisticated digital systems with AI-driven analytics and wireless connectivity. It enables early detection of hypoxemic events, typically 1–2 minutes before clinical signs appear. Although largescale randomized trials have not demonstrated significant reductions in perioperative mortality, it is universally recognized as indispensable for safe anesthetic practice. During the COVID-19 pandemic, it played a crucial role in identifying silent hypoxemia, with home monitoring programs preventing thousands of hospitalizations. Adoption exceeds 95% in high-income countries, with rapid growth in low-resource settings through targeted training and quality initiatives.
Future directions include multi-wavelength technology, AI-enhanced signal processing, and solutions to address skin pigmentation–related accuracy gaps. Integration into telemedicine, medical education, and quality frameworks will secure its role as a cornerstone of next-generation healthcare.
Keywords
<p>Pulse oximetry; Oxygen saturation; Anesthesia monitoring; Critical care; Patient safety; COVID-19; artificial intelligence; Health equity</p>
Article Details
1. Introduction
The introduction of pulse oximetry into clinical practice represents a paradigm shift in patient monitoring that has fundamentally transformed anesthesiology and critical care medicine. Pulse oximeters provide continuous, non-invasive monitoring of arterial oxygen saturation (SpO2), enabling early detection of hypoxemia before clinical signs appear. This facilitates prompt intervention and has made pulse oximetry an essential component of safe anesthetic practice, although definitive evidence for mortality reduction in radomized trials remains limited.
The significance of this technology extends beyond its technical capabilities. Pulse oximetry has significantly improved perioperative safety through early detection of hypoxemia, as demonstrated in large-scale institutional studies and comprehensive reviews [1,2]. The improvement in patient safety has been so profound that pulse oximetry monitoring is now recognized as a standard of care and is mandated by professional societies worldwide [3,4].
From a global health perspective, pulse oximetry has democratized access to sophisticated physiological monitoring, particularly in resource-limited settings where traditional invasive monitoring is unavailable or impractical [5,6]. The recent COVID-19 pandemic further highlighted its critical importance, as pulse oximetry became an essential tool for early detection of silent hypoxemia in patients with coronavirus disease, enabling timely intervention and resource allocation [7,8].
This comprehensive review examines the evolution of pulse oximetry technology, its clinical applications, global impact, and future directions. Particular emphasis is placed on its role in anesthesiology education, quality improvement programs, and implementation science initiatives that have driven its widespread adoption and ongoing refinement.
2. Historical Development and Technological Evolution
2.1 Early Pioneers and Foundational Research
The conceptual foundation of pulse oximetry dates back to the 1930s, when Karl Matthes first described the measurement of oxygen saturation using transmitted light through living tissue [9]. However, it was not until the 1970s that technological advances in light-emitting diodes (LEDs), photodiodes, and microprocessors made practical pulse oximetry possible [10,11].
A major breakthrough came in 1972, when the collaborative efforts of biomedical engineer Takuo Aoyagi at Nihon Kohden (Japan) who introduced the fundamental principle of pulse oximetry, with a patent application filed in 1974 [12]. This Japanese innovation significantly influenced the global medical device industry and established Japan as a leader in non-invasive monitoring technology.
2.2 Commercial Development and Clinical Introduction
The first commercially successful pulse oximeter was introduced simultaneously by Biox and Nellcor in 1981 [13]. Nellcor’s N-100 device became particularly influential in establishing pulse oximetry as a standard monitoring tool. These early systems, while revolutionary, were limited by poor signal-to-noise ratios, motion artifacts, and the need for frequent calibration [10,11]. Their use was largely cinfined to operating rooms and intensive care units, where trained personnel could interpret the readings and manage the technical limitations [4].
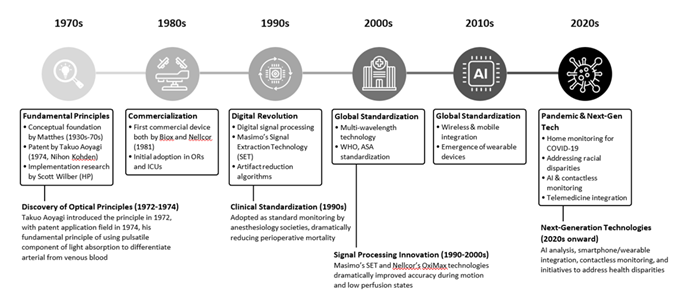
Significant technological advances occurred in the 1990s with the introduction of digital signal processing and improved algorithms for artifact reduction [14]. Companies such as Masimo pioneered signal extraction technology (SET), which used advanced algorithms to isolate arterial signals from noise, dramatically improving accuracy during patient movement and low perfusion states [15,16] (Figure 1).
The timeline illustrates the evolution of pulse oximetry, from Aoyagi’s foundational discovery in the early 1970s to recent advances such as AI-driven algorithms and contactless monitoring.
Historical milestones are based on [9] for basic principles, [12] for Aoyagi’s contributions, [13] for commercial development, and [15] for modern advances. Actual development proceeded continuously and in parallel; only key milestones are highlighted.
Studies in pediatric cardiac surgery have demonstrated the critical importance of pulse oximetry for early hypoxemia detection [17,18]. Continuous monitoring enables earlier detection of hypoxemic events compared to clinical observation alone, with particular benefits in complex congenital heart surgeries [17]. Multiple studies have demonstrated that pulse oximetry-guided interventions can improve perioperative outcomes in pediatric cardiac procedures, though the degree of benefit varies depending on procedure type and patient characteristics [18,19]
3. Physical Principles and Measurement Theory
3.1 Photoplethysmography and Light Absorption
Pulse oximetry is based on the principle of photoplethysmography combined with spectrophotometry. The technology exploits the differential absorption characteristics of oxygenated and deoxygenated hemoglobin at specific wavelengths of light [9,20]. Conventional pulse oximeters use two wavelengths: red light at approximately 660 nm and infrared light at 940 nm [9,10].
The fundamental principle relies on the Beer-Lambert law, which describes the relationship between light absorption and the concentration of absorbing species [9,20]. In biological tissues, the total light absorption consists of contributions from arterial blood, venous blood, and tissue. The key innovation of pulse oximetry is the use of the pulsatile component of light absorption, which corresponds primarily to arterial blood, to calculate oxygen saturation [10,11].
3.2 Advanced Signal Processing and Calibration
The ratio of pulsatile to non-pulsatile light absorption at the two wavelengths (R-value) is calculated and converted to oxygen saturation using empirically derived calibration curves [20,21]. These curves are typically established through studies involving healthy volunteers who breathe hypoxic gas mixtures while arterial blood gas measurements are obtained simultaneously [22].
Modern pulse oximeters incorporate machine learning algorithms that can adapt to individual patient characteristics, improving accuracy across diverse populations and clinical conditions [23]. These sysetems analyze multiple signal parameters simultaneously, including waveform morphology, signal strength, and noise characteristics, to generate more reliable measurements.
4. Industrial Innovations and Key Contributors
4.1 Nellcor (Medtronic)
Nellcor's contributions to pulse oximetry extends beyond device manufacturing to include fundamental research in sensor technology and clinical validation [14]. The company's OxiMax technology introduced multi-wavelength measurement capabilities, improving accuracy in challenging clinical scenarios such as carbon monoxide poisoning and methemoglobinemia [24].
The collaboration of Nellcor with anesthesiology societies was instrumental in establishing pulse oximetry as a standard monitoring requirement [4,19]. The company's extensive clinical studies provided the evidence base for regulatory approval and informed professional guidelines mandating pulse oximetry monitoring during anesthesia [4,19].
4.2 Masimo Corporation
Masimo's Signal Extraction Technology (SET) represents one of the most significant advances in pulse oximetry since its inception [15,16]. By using parallel processing engines and adaptive algorithms, SET technology can extract arterial signals even in the presence of significant motion artifacts and low perfusion states that would render conventional pulse oximeters unreliable [15,16].
The company's rainbow technology extends pulse oximetry beyond traditional SpO2 monitoring to include measurements of total hemoglobin, carboxyhemoglobin, methemoglobin, and pleth variability index [16,24]. This multi-parameter approach has expanded the clinical utility of pulse oximetry in perioperative and critical care settings [16].
4.3 Emerging Technologies and Innovation
Recent innovations include smartphone-based pulse oximetry applications, wearable devices integrated into smartwatches, and contactless monitoring systems using computer vision and machine learning [25,26]. Companies such as Apple, Samsung, and various startups are developing consumer-grade pulse oximetry solutions that may democratize access to oxygen saturation monitoring [26] (Table 1).
|
Manufacturer/Technology |
Technical Features |
Clinical Applications |
Accuracy Characteristics |
Motion Tolerance |
|
Masimo Signal Extraction Technology (SET) |
Parallel processing engines Adaptive algorithms Discrete saturation transform |
Operating rooms Intensive care units Neonatal/pediatric care Low perfusion states |
SpO2: ±2% (70%-100%) High accuracy in low perfusion |
Excellent (validated in clinical studies) |
|
Masimo rainbow SET |
Multi-wavelength measurement Multi-parameter analysis Non-invasive continuous monitoring |
Perioperative monitoring Emergency medicine Carbon monoxide poisoning Methemoglobinemia |
SpO2: ±2% (70%-100%) Total Hb: ±1g/dL COHb: ±3% MetHb: ±1% |
Excellent |
|
Nellcor (Medtronic) OxiMax |
Digital signal processing In-sensor memory chip OXIMART signal processing |
Operating rooms Intensive care units Neonatal monitoring Apnea detection |
SpO2: ±2%~3% (70%-100%) Improved bradycardia detection |
Moderate to good |
|
Nonin Medical PureSAT |
Digital signal processing Compact, power-efficient design Rapid response algorithms |
Home healthcare Emergency/transport Sleep apnea Telemedicine |
SpO2: ±2% (70%-100%) Robust for portable applications |
Good (optimized for portable use) |
|
Consumer/Wearable (Apple, Samsung, etc.) |
Micro-optical sensors AI-assisted analysis Wireless/cloud integration |
Health monitoring Remote patient monitoring Screening Trend analysis |
SpO2: ±3%~4% (90%-100%) Limited vs medical-grade devices |
Limited (optimized for normal activity) |
This comparison is based on [12] for historical development, [15] for SET technology validations, [22] for accuracy studies, and [23] for mobile applications. Accuracy values are shown as standard deviations (±SD). Wearable device accuracy has been validated under limited conditions only, and should not be used for clinical decision making.
Table 1: Comparative Analysis of Leading Pulse Oximetry Technologies.
5. Clinical Applications in Anesthesiology and Critical Care
5.1 Perioperative Monitoring
Pulse oximetry has become an indispensable monitoring tool in anesthesiology, mandated by professional societies including the American Society of Anesthesiologists (ASA), the European Society of Anaesthesiology (ESA), and the World Federation of Societies of Anaesthesiologists (WFSA) [3,4]. The technology enables early detection of hypoxemia during induction, maintenance, and emergence from anesthesia [19,27].
Studies have demonstrated that pulse oximetry monitoring during anesthesia can detect hypoxemic events 1-2 minutes before clinical signs appear, providing critical time for intervention. Although large-scale randomized trials have not shown significant reductions in perioperative mortality, the technology's ability to detect hypoxemia early has made it an indispensable tool for ensuring safety in anesthetic practice [19,27], particularly in high-risk procedures, pediatric anesthesia, and patients with compromised respiratory function [17,18].
During the COVID-19 pandemic, home pulse oximetry monitoring proved clinically beneficial across multiple healthcare systems [8,28,29]. Studies of COVID-19 Oximetry @home programs have shown potential benefits in patient outcomes, with some research suggesting reduced mortality and readmission rates, although results varied across different healthcare systems and implementation strategies [28]. In the U.K., NHS England's virtual ward initiatives utilized pulse oximetry for remote monitoring of COVID-19 patients, enabling early detection of clinical deterioration and reducing strain on healthcare resources [8].
5.2 Critical Care Applications
In intensive care units, pulse oximetry provides continuous monitoring of critically ill patients, enabling the titration of oxygen therapy and mechanical ventilation [1,30]. It is particularly valuable in managing patients with acute respiratory distress syndrome (ARDS), where maintaining optimal oxygenation while minimizing oxygen toxicity is crucial [1,30].
Recent studies have shown that pulse oximetry-guided oxygen therapy can reduce mortality and length of stay in critically ill patients compared to standard care [30]. The technology also enables real-time assessment of responses to positioning, recruitment maneuvers, and other interventions [30].
5.3 Emergency Medicine and Prehospital Care
Portable pulse oximeters have become standard equipment in emergency medical services, providing rapid assessment of patient oxygenation in prehospital settings [31,32]. The technology is particularly useful in managing patients with chest pain, dyspnea, or altered mental status, where hypoxemia may not be clinically apparent.
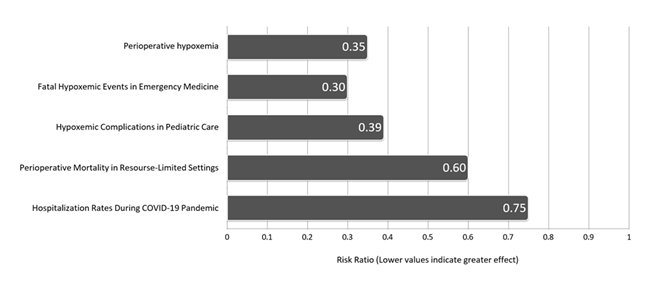
Studies conducted in emergency departments have shown that pulse oximetry can guide triage decisions and resource allocation, particularly during mass casualty events or pandemic surges when rapid assessment of multiple patients is required [33] (Table 2, Figure 2).
The clinical benefits of pulse oximetry adoption are shown across different healthcare settings, including perioperative monitoring, emergency medicine, pediatric care, and global health applications.
Evidence is based on [2] for perioperative benefits, [14] for systematic review outcomes, [32] for emergency medicine applications, and [17] for pediatric applications.
|
Clinical setting |
Representative Studies/Evidence |
Impact on Patient Outcomes |
|
Perioperative Monitoring |
Moller et al, multicenter study Randomized trial involving 20,802 patients |
Early detection of hypoxemia 1-2 minutes before clinical signs Limited evidence for mortality reduction in large, randomized trials Improved perioperative safety monitoring |
|
Emergency Medicine & Prehospital Care |
Comparative studies before and after pulse oximetry implementation in emergency medical systems |
Improved triage decisions Better outcomes through early intervention Optimization of oxygen therapy Reduced cardiopulmonary events during transportation |
|
Pediatric & Neonatal Care |
Fouzas et al, review Khatri et al, prospective observational study |
Improved stabilization protocols for premature infants Optimization of oxygen delivery in preterm infants Early detection of undiagnosed congenital heart disease Reduced PICU admission rates |
|
Low-Resource Settings |
Comparative studies in sub-Saharan African facilities Lifebox Foundation’s global implementation program |
Significant reduction in perioperative mortality Greatest impact in pediatric and obstetric procedures Improved pneumonia diagnostic accuracy Optimized allocation of medical resources |
|
COVID-19 Pandemic Response |
Greenhalgh et al, study Home monitoring programs involving over 100,000 patients |
Early detection of silent hypoxemia Reduced hospitalization rates and improved patient outcomes Improved severity assessment Efficient allocation of healthcare resources |
|
Telemedicine & Home Healthcare |
Home monitoring studies of COPD and heart failure patients Darwish et al, digital health research |
Early detection of acute exacerbations in chronic diseases Reduced readmission rates Improved patient satisfaction Enhanced access to healthcare |
Clinical benefits represent documented improvements in patient outcomes following pulse oximetry implementation. Evidence based on [1, 2] for perioperative monitoring, [32] for emergency care, [17] for pediatric applications, [6] for low-resource settings, [8] for COVID-19 response, and [34] for telemedicine. Effects may vary depending on clinical context, patient characteristics, and equipment used.
Table 2: Clinical Evidence for Pulse Oximetry Impact on Patient Outcomes
6. Educational Applications in Anesthesiology and Critical Care Training
6.1 Residency Training Programs
Pulse oximetry is now an integral component of anesthesiology and critical care training programs worldwide. Educational curricula now incorporate comprehensive instruction on pulse oximetry principles, interpretation, troubleshooting, and clinical decision-making based on oxygen saturation monitoring [35].
Structured programs include hands-on training with various pulse oximetry devices, simulation-based scenarios illustrating common artifacts and limitations, and competency assessment protocols. These programs have demonstrated improved resident confidence and clinical performance in oxygen saturation monitoring [35].
6.2 Simulation-Based Education
High-fidelity simulation centers utilize pulse oximetry monitoring to create realistic clinical scenarios for training anesthesiology residents and critical care fellows. Simulations can replicate complex conditions such as motion artifacts, low perfusion states, and equipment malfunctions, providing trainees with valuable learning experiences in managing these challenges within a controlled environment [36].
Standardized simulation scenarios are used to teach recognition and management of hypoxemic events, appropriate alarm threshold settings, and integration of pulse oximetry data with other physiological parameters. These educational interventions have been shown to improve clinical performance and patient safety outcomes [36].
6.3 Interprofessional Education
Pulse oximetry education extends beyond physician training to include nurses, respiratory therapists, and other healthcare professionals. Interprofessional education programs emphasize team-based approaches to oxygen saturation monitoring, communication protocols for abnormal readings, and collaborative decision-making in clinical care [37].
7. Quality Improvement Programs and Implementation Science
7.1 Patient Safety Initiatives
Healthcare institutions have implemented comprehensive quality improvement programs centered on pulse oximetry monitoring to enhance patient safety. These programs typically include standardized alarm management protocols, regular competency assessments for clinical staff, and systematic analysis of hypoxemic events [38].
Data from such initiatives have demonstrated significant reductions in preventable hypoxemic events, lower false alarm rates, and improved staff satisfaction with monitoring systems. The implementation of evidence-based pulse oximetry protocols has become a key component of hospital accreditation standards [38].
7.2 Alarm Fatigue Management
One of the major challenges in pulse oximetry implementation is alarm fatigue, in which healthcare providers become desensitized to frequent alarms, potentially delaying responses to critical events [39]. Quality improvement programs have addressed this issue through the following strategies:
- • Individualized alarm threshold settings based on patient conditions
- • Smart alarm algorithms that reduce false alarms
- • Staff education on appropriate alarm responses
- • Regular review and adjustment of alarm policies
These interventions have resulted in significant reductions in alarm frequency while maintaining sensitivity for detecting clinically relevant hypoxemic events [39].
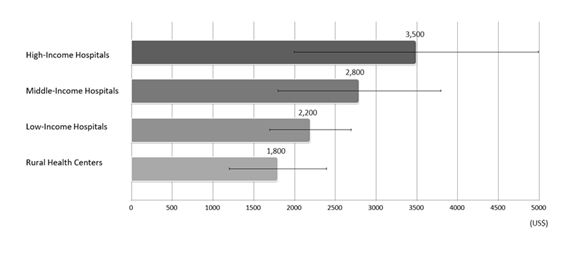
Quality improvement programs in resource-limited settings have demonstrated substantial benefits from systematic pulse oximetry implementation [5, 6]. Studies in low- and middle-income countries have shown that introduction of pulse oximetry monitoring can significantly reduce perioperative mortality, with particularly notable impacts in pediatric and obstetric procedures [6]. The Lifebox Foundation's Safe Surgery initiative has distributed pulse oximeters to healthcare facilities globally and provided training programs, thereby contributing to improved surgical safety outcomes in resource-limited settings [40]. (Figure 3).
Cost-effective analysis showing economic benefits of pulse oximetry implementation across different healthcare settings, with improved cost-effectiveness through prevention of complications and efficient resource utilization.
Values represent the estimated annual economic benefit per facility type. Horizontal bars indicate the point estimates, and thin lines denote the 95% confidence intervals.
Data compiled from [5] for global distribution analysis, [6] for low-resource settings, and [40] for implementation outcomes.
7.3 Implementation Science Perspectives
The global adoption of pulse oximetry provides valuable insights into medical technology implementation. Key factors contributing to successful implementation include [41]:
- • Clinical Evidence: Strong evidence base demonstrating improved patient outcomes
- • Ease of Use: Intuitive operation requiring minimal training
- • Cost-Effectiveness: Favorable economic profile with clear return on investment
- • Professional Endorsement: Support from medical societies and regulatory agencies
- • Cultural Adaptation: Flexible implementation approaches tailored to local contexts
These principles have informed subsequent medical device implementations and continue to guide efforts to expand access to pulse oximetry in underserved populations [41].
8. Global Health Impact and COVID-19 Pandemic Response
8.1 Implementation in Low-resource Settings
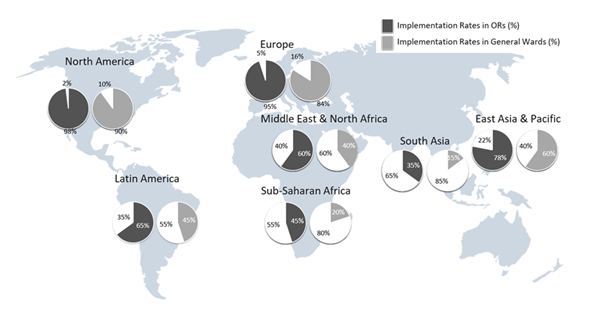
Global efforts to implement pulse oximetry have been driven by initiatives such as the World Health Organization's Global Pulse Oximetry Project and the Lifebox Foundation's Safe Surgery programs [5,40]. These organizations have distributed thousands of pulse oximeters to hospitals in low- and middle-income countries (Figure 4), where lack of monitoring contributes to preventable perioperative deaths [5,6,40].
Map shows estimated regional implementation rates of pulse oximetry based on global surveys and WHO data. Adoption is highest in North America and Europe, moderate in Asia and Latin America, and lowest in Sub-Saharan Africa and South Asia.
Data based on [5] by global operating theater survey, [6] for LMIC implementation, and [40] by Lifebox Foundation global reports. Implementation rates represent pulse oximeter availability in major healthcare facilities.
Studies from sub-Saharan Africa have demonstrated that the introduction of pulse oximetry can significantly reduce perioperative mortality, with the greatest impact seen in pediatric and obstetric procedures [6,33]. The technology is particularly valuable in settings where blood gas analysis is unavailable or impractical [6, 20].
8.2 COVID-19 Pandemic and Home Monitoring
The COVID-19 pandemic highlighted the critical role of pulse oximetry in detecting silent hypoxemia, a phenomenon in which patients maintain normal breathing patterns despite significant oxygen desaturation [7,42]. Home monitoring programs using pulse oximeters enabled early identification of patients requiring hospitalization, potentially preventing thousands of deaths worldwide [8,28].
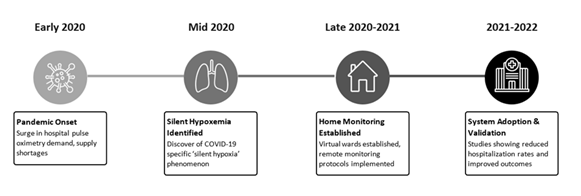
Large-scale studies involving over 100,000 patients demonstrated that home pulse oximetry monitoring could reduce hospital admissions while maintaining patient safety [8,28,29] (Figure 5). The technology enabled healthcare systems to manage surge capacity and allocate resources more effectively during peak pandemic periods [28,29].
Timeline shows the evolution of home pulse oximetry as a key component of COVID-19 response strategies, enabling early identification of silent hypoxemia during the pandemic.
Evidence from [7] for COVID-19 racial disparities, [8] for virtual ward programs, [28] for implementation studies, and [42] for silent hypoxemia mechanisms.
8.3 Telemedicine Integration
The integration of pulse oximetry into telemedicine platforms has expanded access to specialist care, particularly in rural and underserved areas [42,43]. Patients can now transmit real-time oxygen saturation data to healthcare providers, enabling remote monitoring and management of chronic conditions such as chronic obstructive pulmonary disease (COPD) and heart failure [34,43].
Telemedicine integration studies have shown benefits of pulse oximetry-enabled remote monitoring [34,43], including reductions in emergency department visits and hospital readmissions among patients with COPD, although the magnitude of benefit varies by patient population and implementation approach [34]. Systems such as the U.S. Veterans Affairs have implemented pulse oximetry-based telehealth programs for chronic disease management, showing potential for cost savings and improved access to care [43].
9. Technical Limitations and Challenges
9.1 Accuracy Issues in Diverse Populations
Recent studies have identified significant accuracy limitations of pulse oximetry in patients with darker skin pigmentation [22,44,45]. Conventional pulse oximeters may overestimate oxygen saturation in Black and Hispanic patients, potentially delaying recognition of hypoxemia and contributing disparities in care.
The underlying mechanism for these inaccuravies is thought to involve differences in light scattering and absorption due to higher melanin content, which can interfere with the optical measurements [22,44]. In response, regulatory agencies have called for manufacturers to validate devices across diverse populations and develop more inclusive calibration algorithms [7,46,47].
9.2 Motion Artifacts and Low Perfusion States
Despite advances in signal processing, motion artifacts remain a significant limitation of pulse oximetry, particularly in pediatric patients, during transportation, and in patients with tremor or seizures [15,17]. Low perfusion states, such as those caused by shock, hypothermia, or vasoconstriction can also result in unreliable readings.
Advanced signal processing algorithms and alternative sensor sites (e.g., forehead, ear, nasal ala) have been developed to address these limitations, but challenges remain in the most critically ill patients, in whom reliable monitoring is most crucial [15,48].
9.3 Interference from Abnormal Hemoglobin Variants
Conventional pulse oximeters cannot differentiate between normal oxyhemoglobin and abnormal hemoglobin variants such as carboxyhemoglobin and methemoglobin [24,49]. Consequently, pulse oximetry may overestimate oxygen saturation in case of carbon monoxide poisoning or methemoglobinemia [24,49].
To overcome this limitation, multi-wavelength pulse oximeters capable of measuring these abnormal hemoglobin variants have been developed, but are not yet widely adopted due to cost and complexity considerations [16,24].
10. Enhanced Conclusion
Pulse oximetry stands as one of the most transformative medical technologies of the modern era, fundamentally changing the landscape of patient monitoring and safety in anesthesiology and critical care. From its humble beginnings as a research curiosity in the 1970s to its current status as an indispensable clinical tool, pulse oximetry has saved countless lives and continues to evolve with advancing technology.
The impact of this technology extends far beyond the operating room and intensive care unit, reaching into emergency medicine, home healthcare, global health initiatives, medical education, and quality improvement programs. While definitive evidence for mortality reduction in randomized trials remains limited, the ability of pulse oximetry to detect hypoxemia early has fundamentally changed the practice of anesthesiology and critical care. The COVID-19 pandemic demonstrated the critical importance of accessible, reliable oxygen saturation monitoring, while also highlighting persistent challenges in accuracy and equity across diverse populations.
The successful implementation of pulse oximetry worldwide provides valuable lessons for medical technology adoption. The combination of strong clinical evidence, ease of use, cost-effectiveness, professional endorsement, and adaptability to diverse healthcare settings has contributed to its universal acceptance. These same principles continue to guide efforts to address remaining limitations and expand access in underserved populations.
Educational applications of pulse oximetry have transformed training in anesthesiology and critical care, providing standardized approaches to teaching physiological monitoring principles and clinical decision-making. Quality improvement programs centered on pulse oximetry have demonstrated significant gains in patient safety and healthcare delivery efficiency.
As we look toward the future, the integration of artificial intelligence, wearable technology, and contactless monitoring promises to further expand the utility and accessibility of pulse oximetry. However, realizing this potential will require continued efforts to address technical limitations, ensure equitable access, and maintain rigorous standards for accuracy and reliability.
For anesthesiologists and critical care physicians, pulse oximetry remains an essential tool that requires understanding of its capabilities and limitations. As the technology continues to evolve, clinicians must stay informed about new developments while exercising appropriate clinical judgment in interpreting and acting upon pulse oximetry data.
The journey of pulse oximetry from innovation to standard of care exemplifies the impact of biomedical engineering in transforming clinical practice. As we continue to refine and expand its application, we move closer to the goal of universal access to safe, effective patient monitoring that can save lives regardless of geographic location, socioeconomic status, or patient characteristics. Ongoing commitment to addressing health equity issues and developing bias-free monitoring technologies will be essential to ensuring that the benefits of pulse oximetry are available to all.
11. Author Declarations
The author acknowledges the use of artificial intelligence tools including ChatGPT (OpenAI), Genspark AI documents, and AI-powered fact-checking systems for language refinement, literature organization, and content structuring. All scientific content, clinical interpretations, and conclusions were independently verified, critically evaluated, and finalized by the author, who take full responsibility for the accuracy and integrity of this work.
The author declares that there are no conflicts of interest related to any commercial entities, including those mentioned in this manuscript.
References
- Jubran A. Pulse oximetry. Crit Care 19 (2015): 272.
- Ehrenfeld JM, Funk LM, Van Schalkwyk J, et al. The incidence of hypoxemia during surgery: evidence from two institutions. Can J Anaesth 57 (2010): 888-897.
- Eichhorn JH, Cooper JB, Cullen DJ, et al. Standards for patient monitoring during anesthesia at Harvard Medical School. JAMA 256 (1986): 1017-1020.
- Taenzer AH, Pyke JB, McGrath SP, et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology 112 (2010): 282-287.
- Funk LM, Weiser TG, Berry WR, et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet 376 (2010): 1055-1061.
- Usher EJ, Moran JL. Pulse oximetry in paediatric primary care in low-income and middle-income countries: a narrative review. Lancet Glob Health 9 (2021): e349-e355.
- Fawzy A, Wu TD, Wang K, et al. Racial and ethnic discrepancy in pulse oximetry and delayed identification of treatment eligibility among patients with COVID-19. JAMA Intern Med 182 (2022): 730-738.
- Greenhalgh T, Knight M, Inda-Kim M, et al. Remote management of COVID-19 using home pulse oximetry and virtual ward support. BMJ 372 (2021): n677.
- Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med 107 (2013): 789-799.
- Sinex JE. Pulse oximetry: principles and limitations. Am J Emerg Med 17 (1999): 59-67.
- Tremper KK, Barker SJ. Pulse oximetry. Anesthesiology 70 (1989): 98-108.
- Miyasaka K, Shelley K, Takahashi S, et al. Tribute to Dr. Takuo Aoyagi, inventor of pulse oximetry. J Anesth 35 (2021): 671-709.
- Severinghaus JW, Kelleher JF. Recent developments in pulse oximetry. Anesthesiology 76 (1992): 1018-1038.
- Enoch AJ, English M, Shepperd S. Does pulse oximeter use impact health outcomes? A systematic review. Arch Dis Child 101 (2016): 694-701.
- Louie A, Feiner JR, Bickler PE, et al. Four types of pulse oximeters accurately detect hypoxia during motion and low perfusion in volunteers. Can J Anaesth 65 (2018): 44-52.
- Griffin MP, O’Shea TM, Bissonnette EA, et al. Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr Res 55 (2004): 782-788.
- Fouzas S, Priftis KN, Anthracopoulos MB. Pulse oximetry in pediatric practice. Pediatrics 128 (2011): 740-752.
- Badurdeen S, de Guibert C, Guaran R, et al. Accuracy of multiple pulse oximeters in stable critically ill patients. Respir Care 68 (2023): 565-574.
- Moller JT, Johannessen NW, Espersen K, et al. Randomized evaluation of pulse oximetry in 20,802 patients: II. Perioperative events and postoperative complications. Anesthesiology 78 (1993): 445-453.
- Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Med Devices (Auckl) 7 (2014): 231-239.
- Enoch AJ, Hardman JG, Thurlow S, et al. Comparison of pulse oximetry and arterial blood gas analysis in assessing oxygenation. Anaesthesia 74 (2019): 1558-1566.
- Bickler PE, Feiner JR, Severinghaus JW. Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology 102 (2005): 715-719.
- Reyes BA, Reljin N, Kong Y, et al. Towards the development of a mobile phonopulse oximeter for continuous oxygen saturation and pulse rate monitoring. IEEE Trans Biomed Eng 68 (2021): 2739-2749.
- Barker SJ, Badal JJ. The measurement of dyshemoglobins and total hemoglobin by pulse oximetry. Curr Opin Anaesthesiol 21 (2008): 805-810.
- Shcherbina A, Mattsson CM, Waggott D, et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med 7 (2017): 3.
- Scully CG, Lee J, Meyer J, et al. Physiological parameter monitoring from optical recordings with a mobile phone. IEEE Trans Biomed Eng 59 (2012): 303-306.
- Cullen DJ, Nemeskal AR, Cooper JB, et al. Effect of pulse oximetry, age, and ASA physical status on unexpected ICU admission and severity of anesthesia-related complications. Anesthesiology 76 (1992): 696-705.
- Vindrola-Padros C, Sidhu MS, Georghiou T, et al. Implementation of remote home monitoring models during the COVID-19 pandemic in England. EClinicalMedicine 34 (2021): 100799.
- Anesi GL, Jablonski J, Harhay MO, et al. Characteristics, outcomes, and trends of patients with COVID-19-related critical illness. Ann Intern Med 174 (2021): 613-621.
- Sjöstrand F, Malmkvist G. Systematic review of the clinical effectiveness of pulse oximetry in critically ill patients. Acta Anaesthesiol Scand 62 (2018): 1261-1273.
- Lipnick MS, Feiner JR, Au P, et al. The accuracy of six inexpensive pulse oximeters not cleared by the FDA. Anesth Analg 123 (2016): 338-345.
- Brown LH, Hubble MW, Cone DC, et al. Paramedic determinations of medical necessity: a multistate analysis. Prehosp Emerg Care 13 (2009): 505-511.
- Enoch AJ, English M, Shepperd S. Does pulse oximeter use impact health outcomes? A systematic review. Arch Dis Child 101 (2016): 694-701.
- Darwish A, Evans D, Mudalige N, et al. COVID-19 home monitoring: experience of a health system. Telemed J E Health 27 (2021): 410-418.
- McGrath SP, Grigg E, Wendelken S, et al. STAMP: the role of mobile technology in improving patient safety through continuous monitoring of vital signs. Patient Saf Surg 14 (2020): 17.
- Rosen KM, McBride JM, Drake BD. Use of simulation in medical education to enhance understanding of basic sciences. Med Teach 31 (2009): 842-845.
- Institute of Medicine. Health professions education: a bridge to quality. National Academies Press (2003).
- Graham KC, Cvach M. Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care 19 (2010): 28-34.
- Sendelbach S, Funk M. Alarm fatigue: a patient safety concern. AACN Adv Crit Care 24 (2013): 378-386.
- Lifebox Foundation. Safer surgery saves lives: pulse oximetry global challenge. Anesth Analg 117 (2013): 1105-1106.
- Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework. Implement Sci 4 (2009): 50.
- Tobin MJ, Laghi F, Jubran A. Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med 202 (2020): 356-360.
- Menni C, Valdes AM, Polidori L, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med 26 (2020): 1037-1040.
- Wax DB, Beilin Y, Levin M, et al. Effect of melanin on pulse oximetry accuracy: a systematic review and meta-analysis. Anesth Analg 133 (2021): 1465-1479.
- Sjoding MW, Dickson RP, Iwashyna TJ, et al. Racial bias in pulse oximetry measurement. N Engl J Med 383 (2020): 2477-2478.
- Valbuena VSM, Barbaro RP, Claar D, et al. Racial bias in pulse oximetry among patients about to undergo ECMO in 2019–2020. Chest 161 (2022): 971-978.
- Gottlieb ER, Ziegler J, Morley K, et al. Racial and ethnic differences in oxygen supplementation among ICU patients. JAMA Intern Med 182 (2022): 849.
- Vesoulis ZA, Mintzer J, Lodhi H. Validity of photoplethysmographic pulse oximetry in very preterm infants. Respir Care 62 (2017): 1425-1431.
- Burnett GW, Stannard B, Wax DB, et al. Self-reported race/ethnicity and intraoperative occult hypoxemia. Anesth Analg 134 (2022): 951-957.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 