Ultrasound-Guided Midline Catheters in Patients with Difficult Intravenous Access Retrospective Observational Single-Center Study
Hakem Alomani1,5*, Abdullah Muhamed Fahleh1,10, Hayfa Ibnouf1,5 Abdo Saleh Hamdon1,10, Nora Ahmed1,3, Basim Felemban1,6, Hani Redwan1,7, Khaled Masaud1,8, Claudine Neff1,9, Saira Rafiq1,9, Gamal Mohamed2,11, Luluah Althukhaifi2,11, Emad Mohammad Khadawardi1,4,5, Elsaid MY1,5
1King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
2King Faisal Specialist Hospital and Research Centre - Riyadh, Saudi Arabia
3Sidra Medical and Research Center, Al Gharrafa St, Ar-Rayyan, Qatar
4AL Faisal University, Riyadh, Saudi Arabia 5Department of Pediatric, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
6Department of Radiology, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
7Department of Surgery, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
8Department of Anesthesiology, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
9Department of Nursing, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
10Department of Medicine, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
11Department of Biostatistics, Epidemiology and Scientific Computing, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia
* Corresponding author: Hakem Alomani, King Faisal Specialist Hospital and Research Centre - Madinah, Saudi Arabia.
Received: October 02, 2025; Accepted: October 21, 2025; Published: October 27, 2025
Article Information
Citation: Hakem Alomani, Abdullah Muhamed Fahleh, Hayfa Ibnouf, Abdo Saleh Hamdon, Nora Ahmed, Basim Felemban, Hani Redwan, Khaled Masaud, Claudine Neff, Saira Rafiq, Gamal Mohamed, Luluah Althukhaifi, Emad Mohammad Khadawardi, Elsaid MY. Ultrasound-Guided Midline Catheters in Patients with Difficult Intravenous Access Retrospective Observational Single-Center Study. 7 (2025): 109-116.
View / Download Pdf Share at FacebookAbstract
Background: Difficult intravenous access (DIVA) in inpatients is a common problem that impacts patient satisfaction and exhausts resources. A crucial operational goal is to establish a clear and cost-effective process that minimizes the number of pricks to patients, enhances patient satisfaction, and reduces costs. We aim to share our experience and the challenges with difficult IV insertions, highlighting our use of ultrasound-guided midline catheters and a nurse-led program as a novel solution for addressing this problem. To the best of our knowledge, this is the first study in our region.
Materials and Methods: The study is an observational, retrospective analysis. The Midline refers to a peripheral venous access device (PVAD), and data are collected using electronically designed templates for such procedures. We retrieved all Midline-related procedure data from our Health Technology Information Affairs (HITA) from October 01, 2021, to December 31, 2023. Inclusion criteria: all patients (adult or pediatric) with a Midline procedure note by one of (DIVA) program instructors, exclusion criteria: venous access that is non-Midline catheter procedure, Midline procedure done by a non- DIVA member.
Result: A total of 326 lines were inserted into 245 patients. 207 (64.7%) were female, and 113 (74.8%) were adults. The Successful insertion rate was 314 (96.3%), the average number of attempts was 2, and the average dwelling time was 17 days. Physicians inserted 166 (51%) of the Midlines, and nurses inserted 160 (49%). The veins that were commonly used for Midlines were as follows: Right Basilic 104 (32.7%), 97 (30.5%), left basilic, right brachial 25 (7.9%), right cephalic 29 (9.1%), left brachial 128 (8.8%), and left cephalic 32 (10.1%). Indications for Midline insertion were as follows: difficult IV access 206 (63.4%), frequent blood extraction 35 (10.8%), home care 34 (10.5%), palliative care 29 (8.9%), prolonged infusion 9 (2.8%), new oncology diagnosis 6 (1.8%), chemotherapy administration 4 (1.2%) and 2 (0.6%) were missing data. Reasons for removal were complete therapy 207 (65.8%), malfunction 44 (14%), diseased 32 (10.10%), accidental removal 22 (7%), pain and swelling 1 (0.3%), superficial vein thrombosis 8 (2.2%), and other 2 (0.60%).
Conclusion: We found that ultrasound-guided Midline catheters are feasible, relatively safe and cost-effective when used as PVAD in DIVA cases compared with the alternative central venous access devices (CVAD) at our center. The Nurse-Led, US-guided Midline catheter training program appeared to be achievable, reducing the need for rescue expert referral for PICC or CVC.
Keywords
<p>Midline; Difficut IV access; Peripheral venous access</p>
Article Details
Introduction
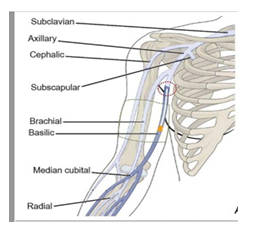
The midline catheter (MC) is a type of peripheral venous access device (PVAD) that falls between central venous access and traditional “short” peripheral venous access, serving as a midway access catheter targeting the deep venous vessels in the upper arm (see Figure 1) [1-3]. However, for precise nomenclature, the authors adopted the recently published position statement called the NAVIGATE project, created by the Global Vascular Access Network (GloVANet), in collaboration with the World Congress of Vascular Access (WoCoVA), which provides nomenclature for vascular access devices [4]. In this document, they classify PVADs based on their length: short peripheral cannulas (SPC) if less than 6 cm, long peripheral catheters (LPC) if 6-15 cm (also known as “mini-midlines” or “short midlines”), and midline catheters (MC) if greater than 15 cm 4. At our institution, all MCs used to fall into the long peripheral catheter category, measuring 8-10 cm. For clarity and brevity, in this document, we will refer to our midline devices as MC and traditional PVADs as short peripheral catheters (SPC). By definition, the MC is considered PVAD, where its tip doesn't end up in the superior vena cava (SVC) or the right atrium, unlike central venous access devices (CVAD) such as the peripherally inserted central catheter (PICC) or the conventional central venous catheter, where their tips are usually positioned in the superior vena cava (SVC) or the right atrium [4]. The invention of midline catheters dates to the 1950s, when they were used as peripheral lines; however, due to numerous reported side effects and complications related to hypersensitivity reactions, they fell out of favor [5]. Following significant redesign changes in both production materials and insertion methods by manufacturing companies, midline catheter use re-emerged. It was advocated for its cost-effectiveness, simplicity, and positive impact on patient satisfaction [6-8].
(source: The longer the catheter, the lower the risk of complications: Results of the HERITAGE study comparing long peripheral and midline catheters Fabiani, Adam et al.)
The SPC remains the primary choice worldwide for venous access due to its low-cost and low-risk nature [9,10]. However, SPC catheters have many inherent limitations, including but not limited to high first-attempt failure rates (26% in adults, 54% in pediatrics), very short dwell times (averaging 44 hours), and the necessity for repeated venipuncture for either placing new SPCs or blood extraction which lead to decrease patients’ satisfaction and increase length of stay in difficult IV access patients [11-14]. PICC line catheters are commonly used for central venous access in inpatients and outpatients who require long-term IV access, prolonged IV infusions, or as a rescue line for patients with DIVA and expected prolonged hospitalization. Although PICC lines can be inserted at the bedside in most centers, at our center, the procedure is performed by an interventional radiology specialist in the interventional suite (IR) and falls entirely under IR jurisdiction. Furthermore, PICC devices are associated with lower risks and complications, including a lower rate of central-line associated blood-stream infection (CLABSI) compared to other CVCs [15-18]. However, PICC lines are costly, requiring specialized trained operators and personnel, and radiological imaging to confirm the location of the tip of the line, and sterile sets are necessary as per the guidelines of the American Society of Anesthesiology for Central Venous Access [19]. On the other hand, the new generation of midline catheters is cheaper than PICC catheters, where the price of one PICC catheter is roughly equivalent to four Midline catheters at our institution for cases of DIVA, and this notion is supported by a recent review from France that compared the costs of different PVADs and PICC lines [20]. (see supplement 1: price comparison at our center between PICC vs MC catheter at our center). Midline catheters can be inserted at the bedside by a single operator under US guidance, with minimal sterility, a longer dwelling time of up to 28 days, and no need for radiological imaging or blood gas to confirm line position [15,21-23]. Furthermore, multicenter studies and systematic reviews have vouched for the safety of Midline catheters compared to PICC in terms of complications, including CLABSI; however, the risk of superficial vein thrombosis (SVT) is found to be higher with Midline catheters compared to PICC catheters [24-27].
Facing patients with difficult IV access (DIVA) who, by definition, have difficulty visualizing and/or palpating their superficial veins or who have failed at least two PIV attempts by expert staff constitutes a frequent problem for inpatient services. Most hospitals have a mitigation plan in place for this problem, which typically includes a rescue venous access type, such as an invasive venous line, like a PICC line or other CVC catheters. Even in the absence of a DIVA situation, anticipating the need for PVAD with an extended dwell time or the need for frequent blood extraction should prompt the healthcare provider to look for an alternative IV access other than the SPC given the known and previously stated facts about the short-dwell time for the SPC cannula resulting in increased usage of many PIV cannula and many venipunctures, which can be inconvenient for the patients and not cost-effective [20]. Furthermore, the Centers for Disease Control and Prevention (CDC) and many other organizations recommend a Midline catheter as an alternative to the SPC in cases of DIVA or anticipated need for IV access for more than 5 days [12,13]. Moreover, midline catheters were found to reduce the need for an extra four PIV cannulas and the need for CVC [14].
Materials and Methods
Ethical consideration:
This study is an observational, retrospective study with prospectively collected data. The study was approved by our Research Ethics Committee in KFSHRC-M (RAC/M2024- 01). The committee waived consent, given the nature of the study, the precautions taken to remove any patient identifiers from data collected by study number, and the link between the study number and patient was maintained with the principal investigator.
Study setting and background:
The hospital has a 400-bed capacity and is a referral tertiary hospital that officially started operating in late 2021 as an extension and third branch of the well-known, internationally recognized King Faisal Specialized Hospital and Research Center (KFSHRC) in Saudi Arabia. Following the successful commissioning and planned operational phases, and with the bed capacity and services expansion, we observed a recurring concern regarding frequent failed SPC attempts, which led to low patient satisfaction and overuse of critical care services (anesthesiology, ICU staff, and interventional radiology) for central venous catheter (such as traditional CVC or PICC) as rescue access.
Difficult IV access team (DIVA team):
We created an initiative that defines a potentially difficult IV access event called a (DIVA case) based on pre-specified criteria (Table 1: criteria of potential DIVA case). It limits the number of PIV attempts by bedside nurses to a maximum of two, with an escalation process to call the DIVA team and use a Midline catheter when SPC fails. Most importantly, it introduces a Nurse-Led US-guided training program for Midline insertion as a long-term mitigation strategy to improve patient satisfaction and avoid overutilization of anesthesia and critical care staff. It also establishes policy and procedures for MC (Table 2: guidelines for Midline).
DIVA training program:
The Midline training program, known as the DIVA program, began with carefully chosen nursing staff called DIVA champions. These nurses first demonstrated mastery of SPC under supervision, completing at least 25 successful
Table 1: Criteria of a potential DIVA case:
The presence of one or more of these factors shall trigger DIVA call
|
• No visible vein after tourniquet |
|
• No palpable vein after tourniquet |
|
• Previous 2 attempts |
|
• Severe dehydration |
|
• Severe edema |
|
• Dark skin |
|
• Expert bedside nurse feels its DIVA case even with the absence of the above criteria |
|
• Family/parents concern about the IV access |
|
• Need for frequent blood extraction |
|
• Need of prolonged IVF /antibiotics for 6 days or more and not a candidate for PICC or CVC. |
Table 2: Guidelines for midlines and rescue central lines in case of
failed Midlines or lack of DIVA services
|
• These guidelines are applicable for inpatients admitted in non- critical areas |
|
• The decision to try another attempt of PIV Vs Midline VS PICC shall be made as a joint decision between the DIVA team and the primary team based on the expected LOS, and need for frequent blood work. |
|
• Midline line is not a central line and shall be used as peripheral line with precaution with max dwelling duration 28 days |
|
• PICC Lines shall be inserted in the Interventional Radiology suite whereas central lines shall be inserted in OR/ICU/PICU when indicated. |
|
• For adult patients: Central Line shall be inserted by Anaesthetist/ Adult ICU attending physician, whereas for Paediatric patients, the central line shall be inserted by PICU attending physician. |
|
• The primary physician of the patient is responsible for liaising with other departments to arrange for rescue central lines like CVC ,PICC when indicated |
PIV insertions. They then learned US fundamentals using a blue phantom through instructor-led simulation sessions. Next, they assessed Midline insertions at the bedside with a DIVA instructor, performing 5-10 insertions. Finally, they completed a check-off list requiring at least 25 supervised, UG-guided Midline insertions on actual patients (see Supplement 2: checkoff list for DIVA champions). Upon completing the program, participants are recognized as DIVA champions, with privileges to perform US-guided PIV insertions, including MC. DIVA services are available only during working hours and involve monitoring adherence to MC guidelines, staff education, data collection, and addressing bedside team concerns.
The process of insertion of the MC:
Once the DIVA case is identified (Table 1), the bedside nurse will contact the DIVA team, who will come to the bedside with the portable US and the DIVA cart (a modified regular cart containing all needed supplies for difficult IV access and Midline insertion). The DIVA champion will first screen the nondominant hand’s upper arm vessels and use a tourniquet as close to the axilla as possible, then choose the suitable vein (basilic, brachial, or cephalic) based on diameter and depth. The area will be sterilized with chlorhexidine 2% (or equivalent) and covered with a fenestrated sterile dressing. The operator will use complete sterile techniques, including standard sterile gloves, a yellow gown, a sterile probe cover, and sterile US gel. For all adult patients, Lidocaine 2%, local infiltrate, will be used, while in small children, we move them to the procedure room on the pediatric floor and mainly use IM ketamine as a moderate sedation option in the absence of SPC. Our center primarily uses the Powerglide Pro Midline Catheters from Bard Access in Salt Lake City, UT, USA, among the many available brands.These catheters employ the accelerated Seldinger technique and are known as all- in-one devices, where the wire, needle, and catheter are pre- assembled and can be advanced easily with one hand (using only the thumb). The recommended dwell time is up to 28 days. They come in sizes 18-22 gauge and lengths of 8-10 cm. In special cases, if the appropriate Powerglide size is unavailable or based on operator preference, the team opts for polyurethane catheters (Leader flex, Vyron) available in 3 Fr (8 cm) or 4 Fr (10 cm), typically used for arterial cannulation. The catheter kit includes a straight tip guide wire. (See Figure 2).
We use a hockey-stick or leaner probe with a cross- sectional view (out-of-plane) and follow the tip of the needle into the vein. Once the tip is confirmed to be inside the vein with visible backflow, the view is changed to a longitudinal (in-plane view) to visualize the deployment of the guidewire inside the vein. We use push-push-pull steps as recommended by the manufacturer, where the first push will deploy the guidewire inside the vein, the second push will deploy the catheter over the guidewire, and the last step (pull) will allow the retrieval of the guidewire and the whole device as one piece while keeping the Midline catheter in place (see figure 3). For stability and line dressing, we use the manufacturer’s recommendation with the Stat Lock stabilization device. There is no need for a chest x-ray or blood gas to confirm the Midline position or functionality.
Data collection process:
The Midline procedures are prospectively collected using auto-populated, electronically designed templates for these procedures, which include the following variables: age, gender, indication, number of attempts, size of the Midline, and immediate complications. We have retrieved all Midline procedure-related data from our Health Technology Information Affairs (HITA) for the years 2021 to 2023. Inclusion criteria: all patients (adult or pediatric) with a Midline procedure note by one of the DIVA program
instructors; exclusion criteria: venous access that is not MC, MC done by non-DIVA program instructors. Discrepancies and disagreements between data collected by data collectors and the biostatistician team were resolved by the principal investigators’ independent review of the original charts (first and last authors).
Data collectors verified the basic data in the MC procedure note. Also, they collected other relevant data not captured by the procedure notes, such as dwelling time, late complications, and basic demographic information. An independent biostatistician reviewed and analyzed the data in light of our outcomes, where our primary outcome is to evaluate the feasibility of MC in DIVA cases, and the secondary outcomes, including assessing the reliability and safety of MC in term of dewing time and pre-defined line- related complications as well as examining the feasibility of using a Nurse-Led US-guided MC training program.
Definition of Line-Related Complications:
The authors identified and defined the expected complications like venous thrombosis: with symptoms like swelling in the ipsilateral arm or difficulty in infusion which should be confirmed by Doppler US as new deep thrombosis (DVT) or superficial venous thrombosis (SVT) in the venous territory where the Midline was inserted, bleeding: active bleeding at the site (moderate to large at the best judgment of the observer that requires prolonged local compression at site or blood transfusion), and site hematoma: local skin discoloration or swelling secondary to blood collection under the skin. The team identified MC malfunction as a maintenance or bedside care problem rather than a line- related complication and defined it as the inability to infuse or withdraw blood through the midline, with no evidence of DVT or SVT, which was analyzed and reported separately.
Statistical analysis plan:
Anticipating the complication types and the need for regression analysis, we also collected more variables that we think could contribute to such complications, including laboratory values related to bleeding tendency (like platelet count, PTT level, INR level), anticoagulation usage, previous history of DVT, and body mass index (BMI). Categorical variables were presented as frequencies and percentages, while quantitative variables were summarized using the mean (SD) and median (interquartile range). Associations between categorical independent variables and complications were assessed using Pearson's chi-square test. Independent sample T-tests were conducted to compare continuous variables between the groups with and without complications. A p-value of <0.05 was considered statistically significant. Data analysis was performed using Stata version 18.
Results
A total of 326 midline catheters were inserted during the study period for 245 patients, with some patients experiencing recurrent admissions or prolonged hospitalization and requiring more than one Midline Catheter during their stay. (Table 3) .Others had more than one Midline due to malfunction or because they had exceeded the recommended indwelling time by the manufacturer (28 days) and had to undergo elective new Midline insertion, which was considered a new Midline event. In summary, sixty-two patients had two midlines, twenty patients had three midlines, seven patients had four midlines, one patient had five midlines, and one patient had six midlines. (The last 2 were long-stay patients with DNAR status on palliative care, non-candidates for invasive lines as per the primary physician).
A total of 64.7% were female, and 74.8% were adults. 59% with medical diseases, 25% with solid tumors, and 16% with hematological malignancies. The Successful insertion rate was 96.3%, the average attempts were 2, and the average dwelling time was 17 days. Physicians inserted 51% of the Midlines, and nurses inserted 49%. The veins that were commonly used for Midlines were as follows: the Right Basilic (32.7%), left basilic (30.5%), right brachial (7.9%),
Table 3: Basic demographic data:
|
N |
326 |
|
GENDER |
|
|
0. Female |
211 (64.7%) |
|
1. Male |
115 (35.3%) |
|
Diagnosis |
|
|
Medical condition |
192 (59.0%) |
|
Solid Tumour |
81 (25%.0) |
|
Haematological Malignancies |
51 (16.0%) |
|
Anticoagulant Medication |
|
|
1. Asprin |
1 (0.6%) |
|
2. Eliquis |
18 (10.5%) |
|
3. Enoxaparin |
124 (72.5%) |
|
4. Heparin |
27 (15.8%) |
|
5. Warfarin |
1 (0.6%) |
|
History of DVT |
|
|
No |
288 (90.0%) |
|
Yes |
32 (10.0%) |
|
Patient Type |
|
|
Adult |
248 (76.1%) |
|
Child |
78 (23.9%) |
|
OPERATOR DESIGNATION |
|
|
Physician |
166 (51.1%) |
|
Physician supervised RN |
56 (17.2%) |
|
RN |
51 (15.7%) |
|
RN supervised RN |
52 (16.0%) |
right cephalic (9.1%), left brachial (8.8%), and left cephalic (10.1%). Most used catheters were Powerglide Pro Midline (87.4%) and Vyron (12.6%), sizes: 20G 10cm (47.9%), 22G 8cm (22.5%), 18G 10 cm (15.1%), 18G 8cm (1.9%), 3Fr 8cm (7.1%) 4Fr 10 cm (5.5%). Indications for Midline insertion were as follows: difficult IV access (63.4%), frequent blood extraction (10.8%), home care (10.5%), palliative care (8.9%), prolonged infusion (2.8%), new oncology diagnosis (1.8%), chemotherapy administration (1.2%) and 0.6% were missing data. Reasons for removal were complete therapy (65.8%), malfunction (14%), diseased (10.10%), accidental removal (7%), pain and swelling (0.3%), superficial vein thrombosis (2.2%), and other (0.60%). Further analysis of the high malfunction rate based on patient type found to be 11% in adults and 3% in the pediatric population, with no clear apparent cause apart from those with SVT. Line insertion- related complications occurred in 10 patients (3.1%), as follows: superficial thrombosis in eight patients (2.5%), local site bleeding in one patient (0.3%), pain at the insertion site in one patient (0.3%), and zero cases of line-related infection. We did further logistic regression analysis for those patients with complications around factors like age, gender, BMI, presence of a history of DVT, usage of anticoagulant medications, and bleeding-related laboratory values (like platelet count, PTT level, INR level). We found no statistically significant association between these variables and the complications as mentioned above. (see supplement 3).
Discussion
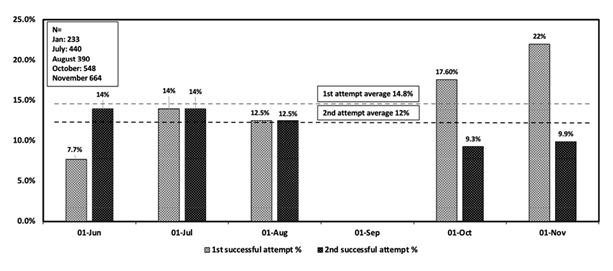
Although the SPC is an easy, safe, and low-cost method of venous access, it still has inherent limitations, including a high failure rate, short dwell time, and an unsuitable source for blood extraction [9-14]. However, our results regarding the SPC failure rate are higher than what was reported (see Figure 4).
These limitations are amplified in inpatients known to have difficult IV access, those expected to have hospitalization stay of more than 5 days, or who require frequent blood draws, which necessitate alternative venous access. Furthermore, in tertiary health systems like ours, where patients often have complex medical issues and are heavily pre-treated, the SPC has become inadequate to meet the demand. The utilization of US-guided PVAD (excluding midline), which primarily utilizes US to secure SPC, has been proposed as a solution for DIVA cases, offering promising benefits of decreasing the need for invasive venous access and improving patient satisfaction [28,29]. However, this modality still did not overcome the problems of short dwelling time and the lack of blood extraction options in these SPC. Midline catheters are a feasible and recommended alternative to PICC catheters for patients with difficult IV access or who are expected to require an infusion of medication for more than 5 days, as they frequently need more than two SPCs or more over their course [12-14]. Moreover, utilization of Midlines decreases the need for CVC associated with fewer complications compared with PICC or other CVC [15-18,24-27]. A recent RCT compared the long peripheral catheters (midlines) with SPC in pediatrics and showed the superiority of long peripheral lines in terms of catheter failure and total catheters in children31. Furthermore, the blood samples obtained by Midlines have recently been validated to be clinically equivalent to those taken in traditional venipunctures [32].
Midline catheter-related complications like bloodstream infection, occlusion rates, and DVTS are still a concern. However, they occur in similar or lower frequency compared with PICC lines, as shown in a recent large cohort study [25]. In a relatively recent systematic review, the Midline catheters had favorable results regarding dwell time and failure rate compared with other types of catheters, which is consistent with our results [33]. Our study demonstrated a
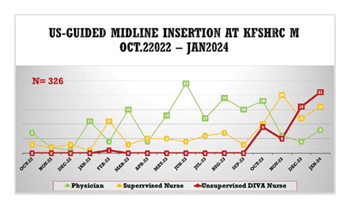
high successful insertion rate of Midline catheters under US guidance, a low complication rate, and a reasonable dwell time compared with SPC and PICC lines [11-15,21-23]. However, we noted a high rate of malfunction that requires further investigation in a larger study. Furthermore, MC at our center appears to be a cost-effective strategy in DIVA cases compared to rescue devices like PICC. Moreover, a recent study comparing the costs of PVADs and PICC devices concurs with our findings at our center [20]. Lastly, our study emphasizes the significance of empowering nurses and demonstrates the feasibility of a nurse-led MC insertion training program, which showed promising outcomes and high satisfaction levels among staff and patients at our center (Figure 5) (supplements: 4, 5). Additionally, a recent publication on MC experience, similar to ours, found that MC can reduce the need for CVADs, suggesting that training programs for such innovative devices are worth investigating as a cost-effective approach [34].
Conclusion
US-guided MC is a feasible, relatively safe, reliable, and cost-effective option when used as PVAD in DIVA cases, compared to alternatives like PICC. The Nurse-Led, US- guided Midline catheter training appeared to be achievable, reducing the need for rescue expert referral for PICC or CVC, where, in effect, most of the Midlines that were inserted during the study period were supposed to be PICC or CVC in the absence of the Midline initiative, which means we safe 245 patients as well as the hospital from 326 PICC or CVC.
Study limitation:
This is a retrospective, single-center study involving a relatively homogeneous population at a facility where oncology is a primary service. The malfunction rate was high, affecting adults more than children, with no clear pattern observed. Most malfunctions happened during routine dressing changes, usually performed by staff nurses other than DIVA champions, indicating a possible weakness in the MC maintenance process. In addition, the US-guided program requires a dedicated team of expert nurses who will be released from their core bedside duties and patient care. This could risk a shortage of essential services and may overwhelm the specialists overseeing the training. Moreover, pediatric analgesia and sedation present additional challenges. While local analgesia often suffices for adults, children typically need moderate sedation. This necessitates a recovery area staffed with airway management specialists and equipped with resuscitation resources.
References
- Adams DZ, Little A, Vinsant C, et The Midline Catheter: A clinical review. Journal of Emergency Medicine 51 (2016): 252-258.
- Alexandrov E, Ranjan L, Spencer T, et al. The use of midline catheters in the adult acute care setting - clinical implications and recommendations for practice. J Assoc Vasco Access 16 (2011): 35-41.
- Cheung E, Baerlocher MO, Asch M, et Venous access: a practical review for 2009. Can Fam Physician 55 (2009): 494-6.
- Van Rens M, Van Der Lee R, Spencer TR, et al. The NAVIGATE project: A Giovante-Wachovia position statement on the nomenclature for vascular access The Journal of Vascular Access 26 (2024): 1439-1446.
- Adverse reactions associated with midline catheters - United States, 1992-1995. From the Centers for Disease Control and JAMA 275 (1996): 749-50.
- Griffiths V. Midline catheters: indications, complications and maintenance. Nurs Stand 22 (2007): 48-58.
- Caballero C, Montealegre S, Cubero P. Medial venous catheter or midline (MVC). Rev Enform 37 (2014): 36-41.
- Schoenfeld E, Shokoohi H, Boniface Ultrasound- Guided peripheral intravenous access in the Emergency Department: Patient-Centered survey. Western Journal of Emergency Medicine 12 (2011): 475-477.
- Bernatchez S. Care of peripheral venous catheter sites: advantages of transparent film dressings over tape and J Assoc Vasc Ac- cess 19 (2014):256-61.
- González López JL, Arribi Vilela A, Fernández del Palacio E, et Indwell times, complications and costs of open vs closed safety peripheral intravenous catheters: a randomized study. J Hosp Infect 86 (2014): 117-26.
- Helm RE, Klausner JD, Klemperer JK, et Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs 38 (2015): 189-203.
- Sabri A, Szalas J, Holmes KS, et Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng 23 (2013): 93-108.
- Centers for Disease Control and Prevention (CDC). Background information - 2011 BSI guidelines - HICPAC (2016).
- Vallecoccia MS, De Pascale G, Taraschi C, et Closed vs open systems: when should short peripheral intravenous catheters be the first choice? J Hosp Infect 89 (2015): 72-73.
- Nielsen EB, Antonsen L, Mensel C, et The efficacy of midline catheters—a prospective, randomized, active- controlled study. International Journal of Infectious Diseases 102 (2020): 220-225.
- Maki DG, Kluger DM, Crnich The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 81 (2006): 1159-1171.
- Chopra V, Anand S, Krein SL, et Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med 125 (2012): 733-741.
- Chopra V, O’Horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 34 (2013): 908-918.
- Apfelbaum, Rupp S, Tung A, et al. Practice Guidelines for Central Venous Access 2020. Anesthesiology 132 (2019): 8-43.
- Meto E, Cabout E, Rosay H, et al. Cost comparison of four venous catheters: short peripheral catheter, long peripheral line, Midline, and PICC for peripheral The Journal of Vascular Access (2014).
- Elia F, Ferrari G, Molino P, et Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. Am J Emerg Med 30 (2012): 712-716.
- Bundgaard Madsen E, Sloth E, Skov Illum Bet The clinical performance of midline catheters-An observational study. Acta Anaesthesiol Scand 64 (2020): 394-339.
- Spiegel RJ, Eraso D, Leibner E, et The Utility of Midline Intravenous Catheters in Critically Ill Emergency Department Patients. Ann Emerg Med 75 (2020): 538-545.
- Chen X, Liang A Meta-Analysis of Incidence of Catheter-Related Bloodstream Infection with Midline Catheters and Peripherally Inserted Central Catheters. Journal of Healthcare Engineering (2022): 1-8.
- Swaminathan L, Flanders S, Horowitz J , et Safety and Outcomes of Midline Catheters vs Peripherally Inserted Central Catheters for Patients With Short-term Indications. JAMA Internal Medicine 182 (2021): 50.
- Lu H, Hou Y, Chen J, et Risk of catheter-related bloodstream infection associated with midline catheters compared with peripherally inserted central catheters: A meta-analysis. Nursing Open 8 (2020): 1292-1300.
- Urtecho M, Roldan VDT, Nayfeh T, et al. Comparing Complication Rates of Midline Catheter vs Peripherally Inserted Central A Systematic Review and Meta- analysis. Open Forum Infectious Diseases 10 (2023).
- Au , Rotte MJ, Grzybowski RJ, et al. Decrease in central venous catheter placement due to use of ultrasound guidance for peripheral intravenous catheters. The American Journal of Emergency Medicine 30 (2012): 1950-1954.
- Schoenfeld E, Shokoohi H, Boniface Ultrasound- Guided peripheral intravenous access in the Emergency Department: Patient-Centered survey. Western Journal of Emergency Medicine 12 (2011): 475-477.
- Dargin JM, Rebholz CM, Lowenstein RA , et Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. The American Journal of Emergency Medicine 28 (2009): 1-7.
- Qin KR, Ensor N, Barnes R, et al. Standard versus long peripheral catheters for multiday IV therapy: a randomized controlled PEDIATRICS 147 (2021).
- Minor C, Pfeiffer Blood Samples from Midline Catheters: Clinically Equivalent to Venipuncture. Journal of Infusion Nursing 47 (2024): 36-41.
- Tripathi S, Kumar S,Kaushik The Practice and Complications of midline catheters: A Systematic review. Critical Care Medicine 49 (2020): e140-e150.
- Latos M, Kosson D, Zawadka M. Poland’s first vascular access team 3-year analysis: Insights and learnings. The Journal of Vascular Access (2024).
Supplementary Information:
https://cdn.fortunejournals.com/supply/acc13564.pdf




 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 77.58%
Acceptance Rate: 77.58%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 