Accuracy of Imprint Cytology for Intraoperative Diagnosis of Sentinel Lymph Node Metastasis in Breast Cancer in BMU
Dr. Nazia Mahzabin1*, Prof. Dr. Samia Mubin2, Prof. Dr. Md. Manir Hossain Khan3, Prof. Md. Ibrahim Siddique4
1Specialist, Department of General Surgery, Bangladesh Specialized Hospital, Dhaka, Bangladesh.
2Professor, Department of Surgical Oncology, Bangladesh Medical University, Dhaka, Bangladesh.
3Professor, Department of General Surgery, Bangladesh Medical University, Dhaka, Bangladesh.
4Professor and Chairman, Department of General Surgery, Bangladesh Medical University, Dhaka, Bangladesh.
*Corresponding author: Dr. Nazia Mahzabin, Specialist, Department of General Surgery, Bangladesh Specialized Hospital, Dhaka, Bangladesh.
Received: 15 July 2025; Accepted: 21 July 2025; Published: 17 December 2025
Article Information
Citation: Dr. Nazia Mahzabin, Prof. Dr. Samia Mubin, Prof. Dr. Md. Manir Hossain Khan, Prof. Md. Ibrahim Siddique. Accuracy of Imprint Cytology for Intraoperative Diagnosis of Sentinel Lymph Node Metastasis in Breast Cancer in BMU. Obstetrics and Gynecology Research. 8 (2025): 203-207.
View / Download Pdf Share at FacebookAbstract
Background:
The prognosis of breast cancer is directly correlated with a quantitative burden, which is a continuous variable and is far more important than the simple presence or absence of nodal disease. Axillary management for patients with breast cancer is evolving, intending to maximize oncologic safety while minimizing surgical morbidity.
Objective:
This study aimed to assess the accuracy of imprint cytology for intraoperative diagnosis of sentinel lymph node metastasis in breast cancer in BMU.
Methods:
This cross-sectional study was conducted in the Department of General Surgery in Bangladesh Medical University (Previous Bangabandhu Sheikh Mujib Medical University), Dhaka, Bangladesh, from August 2022 to July 2023. A total of 24 participants, clinically and radiologically node negative early breast carcinoma patients who were operated in the mentioned hospital, were enrolled in this study appropriate statistical test (Chi-square test) was done to observe and compare intraoperative imprint cytology findings of sentinel lymph nodes with postoperative histopathology findings. Data processing was entered manually, and SPSS-24.0 was also used.
Results:
This study showed that, mean ±SD age was 41 ± 11.3 years. Twenty (83.3%) patients had negative sentinel lymph nodes by imprint cytology, and 4 (16.7%) had positive. Seventeen (70.8%) patients had negative sentinel lymph nodes by histopathology, and 7(29.2%) had positive. The sensitivity of imprint cytology was 57.1%, specificity was 83.3%, positive predictive value was 100%, negative predictive value was 85%, and diagnostic accuracy was 87.5%.
Conclusion:
Intraoperative imprint cytology is a useful method for evaluating axillary lymph node metastases in patients with breast cancer.
Keywords
<p>Accuracy; Breast cancer; Lymph node; Postmenopausal; Premenopausal; Sensitivity; Specificity</p>
Article Details
INTRODUCTION
Breast carcinoma is the most common cancer in females; it accounts for one-third of all malignancies affecting women. this cancer has high metastatic capacity, leading to high mortality. Breast cancer remains a leading dreadful cancer of women in Bangladesh. It has become a hidden burden that accounts for 69% of the deaths of women. In Bangladesh, the rate of breast cancer occurrence is estimated to be 22.5 per 100000 females of all ages. In the case of Bangladeshi women, aged between 15-44 years, breast cancer has the highest prevalence, 19.3 per 100000, compared to any other type of cancer [1]. Cancer from the breast commonly metastasizes to ipsilateral axillary lymphadenopathy. Axillary management for patients with breast cancer is evolving to maximize oncologic safety while minimizing surgical morbidity [2]. The single most important predictor of outcome for women with breast cancer is the status of regional lymph nodes [3]. Traditionally, axillary lymph node status has been evaluated by routine axillary lymph node dissection accompanying lumpectomy or mastectomy operation [4]. The role of axillary surgery is to stage the patient by sentinel lymph node biopsy and to treat the disease by axillary lymph node dissection. However, axillary dissection carries a significant risk of chronic morbidities like lymphedema, numbness, axillary web syndrome, and decreased upper-extremity range of motion [5]. To avoid such risks, the utilization of lymphatic mapping techniques for breast cancer has made intraoperative evaluation of sentinel lymph nodes attractive. Intraoperative diagnosis of metastasis to the sentinel lymph node allowed the axillary dissection to immediately follow the sentinel lymph node biopsy. This would reduce the risk of unnecessary secondary surgery; thus, the patient would have only one recovery period [6]. Currently, there is no standard recommended method for Sentinel lymph node assessment, but there are some techniques like imprint cytology, frozen section, immunohistochemistry, and infrared spectroscopy [7]. There are two main ways to evaluate the SLN status during surgery: frozen section (FS) histology and imprint cytology (IC). Most pathologists are more familiar with intraoperative FS examination; however, it is more time-consuming and expensive than IC and has the major disadvantages of nodal tissue loss and freezing artifacts [8]. Frozen section evaluation of sentinel lymph nodes has a false negative rate of 10-12%. The SLN IC interpretation had a sensitivity of 66.7 to 85.7% (pooled: 82.7%). The study showed a low false-negative rate. Imprint cytology preparation with H and E stain alone is the best (simple, fast, easily performed, inexpensive, and highly accurate) way of intraoperative sentinel lymph node diagnosis in breast cancer patients [9]. This study is to record the accuracy of the imprint cytology technique as a predictor of Metastasis seen on a single, surface hematoxylin and eosin (H&E) stained section of the sentinel lymph node.
Methodology
This was a cross-sectional study that was conducted in the Department of General Surgery, Bangladesh Medical University (Previous Bangabandhu Sheikh Mujib Medical University), Dhaka, Bangladesh, from August 2022 to July 2023. During this time, protocol development, data collection, data entry, processing, and analysis were done. A total of 24 participants, clinically and radiologically node negative early breast carcinoma patients who were operated on in the mentioned hospital, were enrolled in this study. A convenience sampling technique was applied for this study. As per the inclusion criteria of this study, female patients with histologically proven carcinoma breast with sonological node-negative axilla and FNAC-proven node-negative axilla were included. On the other hand, according to the exclusion criteria of this study, advanced inoperable carcinoma breast, inflammatory breast carcinoma, recurrent breast carcinoma, metastatic breast carcinoma, carcinoma breast in post-NACT state, and axillary lymph node metastasis proven by FNAC were excluded. The study was approved by the ethical committee of the mentioned hospital. Data processing was entered manually, and SPSS-24.0 was also used.
Result
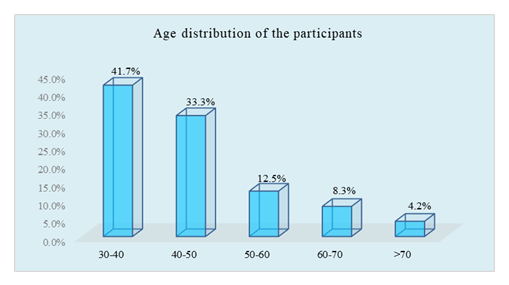
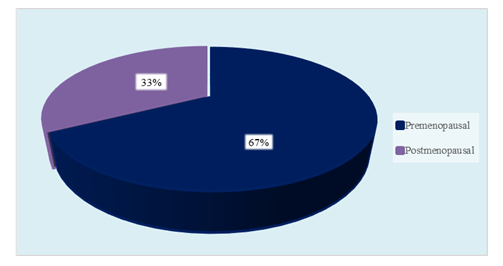
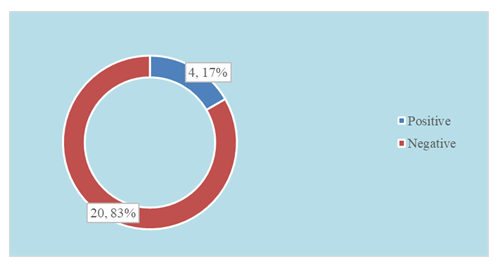
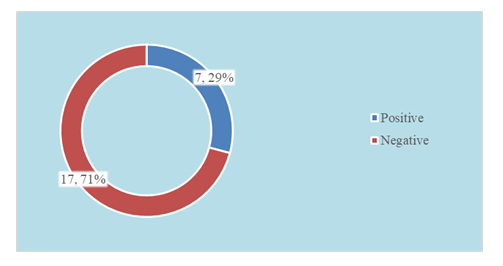
In this study, the age distribution of the respondents showed that 10 patients (41.67%) were between 30–40 years, 8 (33.3%) between 40–50 years, 3 (12.5%) between 50–60 years, 2 (8.3%) between 60–70 years, and 1 patient (4.2%) was over 70 years of age. The mean age was 41 ± 11.3 years. About menopausal status, 16 patients (66.7%) were premenopausal and 8 (33.3%) were postmenopausal. T staging was assessed using imaging findings. Among the cases, 11 patients (45.83%) had T1 tumors (<2 cm), while 13 (54.16%) had T2 tumors (2–5 cm). Sentinel lymph node (SLN) evaluation by imprint cytology revealed that 83.3% of patients had negative results, while 16.7% showed positive findings, indicating metastasis. Histopathological assessment of SLNs showed that 17 patients (70.8%) were negative, whereas 7 (29.2%) were positive for metastasis. Regarding the number of excised lymph nodes, 6–10 nodes were removed in 12 cases (50%), 10–15 nodes in 8 cases (33.33%), and 15–20 nodes in 4 cases (16.67%). Analysis of nodal metastasis showed no involvement in 16 patients (66.7%), involvement of 1–3 nodes in 6 patients (25%), and 8 positive nodes in 1 patient (4.2%). Comparative analysis between imprint cytology and histopathology revealed that all 4 imprint-positive cases were confirmed positive by histopathology. Among 20 imprint-negative cases, 3 were histopathologically positive, while 17 were negative. The calculated sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of imprint cytology were 57.1%, 83.3%, 100%, 85%, and 87.5%, respectively.
Table 1: Distribution of cases by T staging (T1<2 cm, T2 2-5 cm) by imaging findings (N=24).
|
T staging by imaging findings |
n |
% |
|
T1 |
11 |
45.80% |
|
T2 |
13 |
54.20% |
Table 2: Distribution of the respondents by axillary lymph nodes at ALND (N=24).
|
Total excised LNs |
n |
% |
|
6-10 nodes |
12 |
50.00% |
|
10-15 nodes |
8 |
33.30% |
|
15-20 nodes |
4 |
16.70% |
|
Positive LNs |
||
|
0 |
16 |
66.70% |
|
01-Mar |
6 |
25.00% |
|
8 |
1 |
4.20% |
Table 3: Comparison of imprint cytology with post-operative histopathology report (N=24)
|
Histopathology Report |
|||
|
Imprint |
HPR (+) |
HPR (-) |
Total |
|
Positive (n=4) |
4 |
0 |
4 |
|
Negative (n= 20) |
3 |
17 |
20 |
Table 4: Sensitivity and specificity of Imprint cytology (N=24).
|
Parameter |
Value |
|
Sensitivity |
57.10% |
|
Specificity |
83.30% |
|
Positive predictive value |
100% |
|
Negative predictive value |
85% |
|
Accuracy |
87.50% |
Discussion
In this study, 10 (41.67%) of the respondents were within the age group of 30-40 years, 8 (33.3%) within the 40-50. Mean ± SD age was 41 ± 11.3. Pereira et al [10]. found 210 cases of breast cancer patients submitted to an intraoperative sentinel node for imprint cytology, aged between 24 and 86 years, with a mean age of 59 years. Petropoulou et al [8] found that 60 patients were registered, and the average age was 61.3 years, with a range between 31 to 82 years. Halliley et al [11] found the mean age was 56 years with a range from 30 to 85 years. Considering our study, the early onset of breast cancer may be more addressable due to geographical variations, ethnic differences, genetic causes, and different lifestyles. Here, most of the patients, about 20 (80%), were housewives. On educational status, 10 (41.7%) were below SSC. Among the study group, 16 (66.7%) patients were Premenopausal and 8 (33.3%) were Postmenopausal. Menopausal respondents were found in 57.2% of patients in a study conducted by Rahman [12]. In this study, regarding T staging by Imaging, we found T1 (< 2 cm) was in 11 (45.83%) patients and T2 (2-5 cm) was in 13 (54.16%) patients. A previous study showed that half of the cancers were T1 (52%) and lymph node negatives (52%). Only 42 women (2.5%) had metastasis at the time of diagnosis [13]. This study shows, 20 (83.3%) patients had negative sentinel lymph nodes by imprint cytology and 4 (16.7%) had positive. Limberis et al [14]. found that of 41 sentinel nodes examined by imprint cytology, there were 16 reported as positive. In this study, 17 (70.8%) patients had negative sentinel lymph nodes by histopathology, and 7(29.2%) had positive. Another study showed that histopathologic examination on permanent sections revealed sentinel lymph node examination, metastasis in 29 of 124 cases, 23.4%, and 37 of 303 (12.2%), including 8 cases with micro-metastasis, defined as a focus less than 2 mm. There were four false negative cases, and all had only micro-metastasis [15]. Regarding total excised LNs, 6-10 nodes were excised in 12 (50%) cases, 10-15 nodes were excised in 8 (33.33%) cases, and 15-20 nodes were excised in 4 (16.67%) cases. Regarding positive LNs, no nodal metastasis in 16 (66.7%) cases, 1-3 nodes were positive in 6 (25%) cases, and 8 nodes were positive in 1 (4.2%) case. A previous study showed, Imprint cytology detects 15 of the 19 patients with metastases, enabling an immediate ALND. Hence, using TIC, only four of 100 women are likely to require delayed ALND, with none undergoing an unnecessary procedure [16]. Touch imprint identified 67% of cases requiring axillary dissection (patients with positive sentinel biopsy). Twelve patients had their axillary dissection performed immediately after the sentinel node biopsy [11]. Regarding comparison, in this current study 4 cases that were positive in imprint cytology were also positive in histopathology. Among negative 20 cases in imprint 3 cases were positive & 17 cases were negative in histopathology. Kalinganire, et al [17]. reported that in 124 cases 105 cases were negative in imprint cytology among these 94 cases were negative and 11 cases were positive in histopathology. In 19 positive imprint cytology cases 1 case was negative and 18 cases were positive in histopathology. In this current study, the results of imprint cytologic examination of sentinel nodes had sensitivity of 57.1%, specificity of 83.3%, PPV of 100%, NPV of 85% and diagnostic accuracy of 87.5%. Henry-Tillman et al. 2002 reported that the sensitivity for imprint cytology was 94% with a false-positive rate of 0.2% in 247 patients. Barranger et al. 2004 reported that imprint cytology had a sensitivity of 33%, specificity of 98%, and overall accuracy of 79%. Cox et al. 2005 reported the results of intraoperative imprint cytology in 2137 patients with T1-2 breast cancer. Chicken et al. 2006 reported that imprint cytology detected metastases with a sensitivity of 73% and a specificity of 100% in 133 breast cancer patients. Abe et al [18] reported, imprint cytology showed 50% sensitivity, 100% specificity, 100% PPV, and 60% NPV. The sensitivity & specificity of imprint cytology comparing to other studies varied in some extent may be due to various factors, including the small size of metastases that might be missed, sampling errors, issues related to the technique used during the intraoperative process, and the limited amount of tissue analyzed in the imprint cytology method, which may not cover the entire lymph node for assessment.
Limitations
The imprint cytology test was histopathology-dependent and a single dye technique.
Conclusion
Imprint cytology can be an alternative method for intraoperative analysis of sentinel nodes in patients with breast cancer, where the traditional tools for SLNB are not available.
Recommendation
In clinically and radiologically node-negative early breast cancer patients, we can employ intraoperative imprint cytology to assess axillary lymph node status. For the intraoperative assessment of sentinel node imprint cytology can be considered as a suitable alternative if the frozen section is not available.
References
- Forazy, Mohd Anisur Rahman. "Incidence of breast cancer in Bangladesh." Health Care 3.3 (2015): 53-54.
- Zaveri, Shruti, et al. "Racial disparities in time to treatment persist in the setting of a comprehensive breast center." Annals of surgical oncology 29.11 (2022): 6692-6703.
- Cools-Lartigue, Jonathan, and Sarkis Meterissian. "Accuracy of axillary ultrasound in the diagnosis of nodal metastasis in invasive breast cancer: a review." World journal of surgery 36 (2012): 46-54.
- Magnoni, Francesca, et al. "Axillary surgery in breast cancer: an updated historical perspective." Seminars in oncology. Vol. 47. No. 6. WB Saunders, (2020).
- Liu, Miao, et al. "Could axillary clearance be avoided in clinically node-negative breast cancer patients with positive nodes diagnosed by ultrasound guided biopsy in the post-ACOSOG Z0011 era?." PLoS One 14.1 (2019): e0210437.
- Gillis, Chelsia, et al. "Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer." Anesthesiology 121.5 (2014): 937-947.
- Pétursson, Hafsteinn Ingi, et al. "Evaluation of intraoperative touch imprint cytology on axillary sentinel lymph nodes in invasive breast carcinomas, a retrospective study of 1227 patients comparing sensitivity in the different tumor subtypes." PLoS One 13.4 (2018): e0195560.
- Petropoulou, Thalia, et al. "Imprint cytology versus frozen section analysis for intraoperative assessment of sentinel lymph node in breast cancer." Breast Cancer: Targets and Therapy (2017): 325-330.
- Chang, Yi-Chin, and Chi-Yuan Tzen. "Intraoperative sentinel lymph node imprint cytology diagnosis in breast cancer patients by general surgical pathologists: A single-institution experience of 4327 cases." Journal of Cytology 39.1 (2022): 20-25.
- Pereira, Talita Siemann Santos, et al. "Value of the intraoperati Ve cytology examination of sentinel lymph node in breast cancer." Mastology 28.4 (2018): 212-218.
- Halliley, Jessica L., et al. "Long-lived plasma cells are contained within the CD19− CD38hiCD138+ subset in human bone marrow." Immunity 43.1 (2015): 132-145.
- Rahman, Md Ashfikur, et al. "Trends in the prevalence and associated factors of prediabetes and diabetes in Bangladesh: Evidence from population-based cross-sectional surveys." Diabetes Research and Clinical Practice 190 (2022): 109873.
- Gomez-Acebo, Ines, et al. "Tumour characteristics and survivorship in a cohort of breast cancer." (2020).
- Limberis, V., et al. "Intraoperative estimation of sentinel lymph nodes in breast cancer by imprint cytology." Eur. J. Gynaec. Oncol. -ISSN 392 (2009): 2936.
- Nakagawa, Misako, et al. "Preoperative diagnosis of sentinel lymph node (SLN) metastasis using 3D CT lymphography (CTLG)." Breast Cancer 23 (2016): 519-524.
- Wu, Siyu, et al. "Intraoperative touch imprint cytology in targeted axillary dissection after neoadjuvant chemotherapy for breast cancer patients with initial axillary metastasis." Annals of Surgical Oncology 25 (2018): 3150-3157.
- Kalinganire, Nadia. The Utility of Imprint Cytology of Gastrointestinal Endoscopic Tissue Biopsies At Kenyatta National Hospital. Diss. University of Nairobi, (2016).
- Abe, Makoto, Tetsuya Yamada, et al. "Prospective comparison of intraoperative touch imprint cytology and frozen section histology on axillary sentinel lymph nodes in early breast cancer patients." Acta cytologica 64.5 (2020): 492-497.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 