Assessing the Accessibility and Healthcare Quality of Maternal and Child Health Services in Health Facilities of Kasai Province in the Democratic Republic of the Congo: A Cross-Sectional Study
Britou Ndela1, Philippe Ngwala1, Adrien N’siala1, Albert Kalonji1, Felix Minuku1, Nancy Ntatukidi1, Harmonie Bokole1, Jean-Jacques Masumbuku1 and Ngoma Miezi Kintaudi1 and Bien-Aimé Mandja2,3*
1SANRU Asbl, Kinshasa, Democratic Republic of the Congo
2Service of the Ecology and Control of Infectious Diseases, Faculty of Medicine, University of Kinshasa, Kinshasa, Democratic Republic of the Congo
3Faculty of Medicine, University of Bandundu, Bandundu, Democratic Republic of the Congo
*Corresponding Author: Bien-Aimé Mandja
Received: 26 June 2022; Accepted: 05 July 2022; Published: 17 September 2022
Article Information
Citation: Reema Afroza Alia, Nayeema Sadia, Nazma Parvin Shammy, Ferdous Ara Tithy, Rumana Shelim, Rukhsana Parvin. Diarrhoeal Disease in Relation to Childhood Malnutrition and Its Impact on Socioeconomic Condition in Emerging Countries Like Bangladesh. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 380-389.
View / Download Pdf Share at FacebookAbstract
Background: The Democratic Republic of the Congo (DRC) is among the five countries with the highest global maternal mortality ratio (MMR) and the highest under-five mortality rate (U5MR) worldwide. One of the 14 provinces in the DRC that have high U5MR and MMR is Kasai. Despite this overriding concern, assessment of the maternal and child situation in this province remains poorly reported.
Objectives: This study aimed to assess the accessibility, availability, and quality of maternal and child health services in Kasai province.
Methods: A total of 49 health facilities (HFs) in 18 health zones in Kasai province participated in our cross-sectional survey. To collect quantitative and qualitative data, we conducted documentary review, interviews, and direct observation of HFs. Furthermore, the relationship between variables was analyzed by Pearson’s chi-squared test.
Results: Nearly 54% of the population in surveyed HFs had geographical access to maternal and child health services, and most of the medical services were unaffordable. Only 11.8% and 7.6% of the HFs offered basic and comprehensive emergency obstetric care (EmOC), with no high-quality level of care. The low availability and quality of EmOC were caused by the insufficiency of necessary inputs and personnel for maternal and child health services in the majority of HFs.
Conclusions: The situation of maternal and child health services is extremely precarious in Kasai province in the DRC. Rehabilitation of infrastructure, dotation of equipment, regular supply of medicines, and strengthening of human resource capacity are required to improve the EmOC coverage.
Keywords
<p style="text-align:justify">Democratic Republic of the Congo; Kasai province; maternal and child health services; access; availability; quality; emergency obstetric care</p>
Article Details
Abbreviation:
DRC: Democratic Republic of the Congo; MMR: Maternal mortality ratio; U5MR: under-five mortality rate; RMNCH: reproductive, maternal, newborn and child health; LiST: Lives Saved Tool; (HF: health facilities; EmOC: emergency obstetric care; UN: United Nations; MDGs: millennium development goals; SDGs: Sustainable Development Goals; HZs: health zones; GRHs: general referral hospitals; Has: health areas; HCs: health centers; HPs: health posts, QGIS: Qantum Geographic Information System; WHO: World Health Organization; HAI: Health Action International.
1. Background
Maternal and child mortality is a major public health concern in most low-income countries. In 2015, nearly 88% of maternal deaths and 81% of under-five deaths worldwide occurred in Sub-Saharan Africa (66.3% and 49.6%, respectively) and Southern Asia (21.7% and 31.8%, respectively) [1-4].
The Democratic Republic of the Congo (DRC) is among the five countries with the highest global maternal mortality ratio (MMR) (846 deaths per 100,000 live births) and the highest under-five mortality rate (U5MR) (104 deaths per 100,000 live births) worldwide [2, 3, 5-7]. In fact, high U5MR and MMR were found in the following 14 DRC provinces: Tanganyika, Haut-Lomami, Sankuru, Maniema, Lomami, Tshuapa, Kongo Central, Sud-Kivu, Kasai-Central, Lualaba, Mongala, Sud-Ubangi, Kwango, and Kasai [5].
Maternal deaths are mainly caused by obstetric hemorrhage, infections (sepsis), unsafe abortion, hypertension (eclampsia), and prolonged and obstructed labor [1, 2]. The leading causes of neonatal mortality (0–27 days of existence) are preterm birth complications, intrapartum-related complications (birth asphyxia), congenital abnormalities, and infection (neonatal sepsis and meningitis, pneumonia, tetanus, and diarrhea) [3, 4]. Moreover, the leading causes of under-five mortality are: malaria, pneumonia, diarrhea, meningitis, acquired immune deficiency syndrome, measles, and pertussis [3, 4].
The first 24 hours after birth is an extremely critical period for the survival of both the mother and the newborn [1, 2]. Packages of reproductive, maternal, newborn and child health (RMNCH) interventions were developed in the form of the Lives Saved Tool (LiST) to reduce maternal and child mortality [8]. These evidence-based interventions are provided in the services of health facilities (HFs), commonly named emergency obstetric care (EmOC) [9, 10].
Sufficient inputs and qualified personnel for the EmOC are needed to effectively implement these intervention packages [11]. Available and accessible HFs with sustainable infrastructure, qualified and trained staff in RCMNH package, sufficient equipment, materials, essential drugs and delivery follow-up tools can properly manage potentially fatal obstetric complications and prevent maternal death [12, 13]. Basic EmOC has seven basic signal functions, such as anticonvulsant, antibiotic and oxytocin parental administration, basic neonatal resuscitation, manual placenta extraction, retained product removal, and assisted vaginal delivery. For the comprehensive EmOC, blood transfusion and cesarean section are performed in addition to the seven basic signal functions [14].
To improve the maternal and child health, the United Nations (UN) Member States committed in 2000 to achieve the millennium development goals (MDGs). MDG 4 stated a two-thirds reduction of U5MR between 1990 and 2015, whereas the MDG 5 required a three-quarters reduction of MMR during the same period [2,4]. The assessment of MDG 4 and 5 showed that the majority of Sub-Saharan African countries had not achieved the set targets [4,7]. Failure to achieve these MDGs may be due to low coverage, poor quality, and inequities of implementation of key RMNCH interventions in most Sub-Saharan Africa countries [12]. In 2016, MDGs were replaced by the Sustainable Development Goals (SDGs), which should be achieved by 2030 [1,2]. Thus, healthcare professionals of these countries must increase the coverage of each high-impact RCMNH intervention to 90% to achieve the targets of the SDGs [1, 3].
Unfortunately, the access, availability, and quality of EmOC in the DRC remain poorly evaluated. According to Casey et al., among the hospitals in five DRC provinces (Kasai Occidental, Kinshasa, Maniema, Province Orientale, and Sud-Kivu), none has provided basic nor comprehensive EmOC in 2007 [15]. A research conducted in three western provinces of the DRC in 2012 according to the old configuration (Bandundu, Bas-Congo, Kinshasa) estimated that only 6% of the health structures have EmOC [16]. A mapping interventions in maternal, neonatal, and infant health performed in all provinces of the DRC in 2011 found that nearly 60% of HF were applying active management during the third stage of labor and less than 50% of them were using partogram [17]. Furthermore, Mpunga Mukendi et al. showed that only 9.1% of HF provided basic EmOC and 2.9% of HF provided comprehensive EmOC in 2014 among surveyed HF of the DRC nationwide [18].
However, the population's affordability to these services in the DRC remains insufficiently studied, and almost no research was conducted in the central provinces of the DRC after the new administrative division, especially in those with high maternal and child mortality, such as Kasai. In 2017, the U5MR of Kasai province was approximately 169 deaths per 1,000 live births, the highest ratio in the country. This province also had a high MMR, accounting for 549 deaths per 1,000 live births [5].
This study aimed to assess the accessibility, availability, and quality of EmOC in the HFs of Kasai province in the DRC.
2. Methods
2.1. Ethics Statement
This research was reviewed and approved by DRC Protestant University ethics committee (ref: CEUPC 0059). The research team obtained informed written consent for each participant. Data were collected anonymously after obtaining authorizations from provincial health and HZ authorities prior to the survey.
2.2 Study Design
A cross-sectional survey using mixed methods was conducted in 2019, with quantitative and qualitative data collection of maternal and child health.
2.3. Setting
The study was conducted in Kasai, which is one of the 26 DRC provinces. Located in the south-central part of DRC, Kasai covers an area of 95,631 km2 (Figure 1), with approximately 5,193,271 inhabitants in 2018 [19].
(Source: The provincial Shapefile not copyrighted was obtained from the free and open website (https://data.humdata.org/dataset/drcongo-settlements), then we used this Shapefile to draw the administrative map of Kasai province using the free software QGIS 12.8.
The province is inhabited by three main ethnic groups, namely, the Luba-Kasai, Kuba, and Lunda-Tshokwe. Their main economic activities are farming, industrial and artisanal mining. Kasai is subdivided into 18 health zones (HZs) and includes 18 general referral hospitals (GRHs), 395 health areas (HAs), 448 health centers (HCs) and 703 health posts (HPs). The HZ constitutes the operational level of the DRC’s health pyramid. Each HZ has one GRH and 1–20 HCs, with a population of 100,000–300,000 [19].
2.4. Study population and sampling procedures
In the survey, we included all 18 GRHs of Kasai province as well as 31 HCs according to the follow inclusion criteria: (a) population covered more than 10,000 inhabitants; (b) a high MMR; (c) a high U5MR; and (d) postpartum high-rate of obstetric complications.
The study was conducted in only 31 HCs taking into account the resources available during the survey. However, the sampling used allowed us to ensure the representativeness of the HCs in all axes of each HZ. A total of 272 HCs (60.71%) fulfilled the criteria.
Sampling was performed in two stages. HCs were selected using a systematic random sampling. First, the sampling step was computed by dividing the number of HCs to be surveyed by the total sample size. Second, the number of first HC was selected randomly between 1 and the sampling step. Third, the remaining facilities were selected by adding the sampling step to the number of each identified HC. This procedure was followed until all HCs were selected.
Exhaustive sampling was used involving all health workers practicing activities of RMNCH present in the structure on the day of the survey.
The statistical unit for the study was the HF. Each interviewed health professional helped answer the part of the HF questionnaire that corresponded to the activity he or she was conducting in the RMNCH service.
2.5. Data collection and study procedures
Data were collected from February 23, 2019 to March 14, 2019. The survey used various methods combining quantitative and qualitative data collection. As the first quantitative approach, we directly interviewed the RMNCH heads of the selected structures, with the use of a questionnaire. This approach allowed us to perform documentary review (the annual or monthly reports of each zone and HA). For the qualitative approach, we conducted first semistructured individual interviews with the chief medical officers of HZs and the RMNCH heads of the selected structures. Then, we directly observed the HFs. During the observation, the investigators checked the condition of the medical equipment or infrastructure, whether they were old or not or whether the infrastructure were made of durable materials or not. A pilot test in HFs that were not selected in the survey was conducted before the study.
Provincial-type Shape file was downloaded from free and open website
(https://data.humdata.org/dataset/drcongo-settlements). To measure geographical accessibility of the population, we computed the distance between the patients’ residence and the HC. The population of each village and the distance between each village and the HC were collected at the central office of each HZ. The residence was considered geographically accessible if the population lived within a radius of 5 km or lived far from a natural obstacle (rivers, mountains, etc.) preventing a person from reaching the HC within 1 hour walk [20]. Moreover, affordability was assessed using the standardized and adapted methodology of World Health Organization (WHO) and Health Action International (HAI) [21]. Firstly, prices of medicines and medical services were expressed in Congolese Franc. The average exchange rate used in June 2019 was 1$ = 1675.5 Congolese Franc [22]. Secondly, affordability was calculated according to the number of days needed to pay for standard essential medicines or medical services and the populations’ lowest daily income (nearly 0.85$ per person) [19]. Medicines or medical services costing more than the daily income were considered unaffordable. The qualification and training of health professionals in the RMNCH package were determined using the annual reports of HZ. Then, health professionals were classified into the following three categories: nurses A2 level (secondary level education), nurses’ A1 level (undergraduate university level), and nurses’ L2 level (licensed nurses or completed university level). Meanwhile, the physical presence of infrastructures, equipment/healthcare materials, essential medicines and consumables in sufficient stock, and delivery and data reporting tools during the survey were used to assess HF availability. The equipment/healthcare materials, essential medicines and consumables, which were collected during the survey, were adapted from the list of interventions proposed by RMNCH experts [1, 23]. An infrastructure was considered sustainable if it had at least 11 RMNCH services (delivery room with delivery bed with newborn corner, water drainage and soakaway, incinerator, light source, labor room, space for prenatal, postnatal and preschool consultations, safe water source, or handwashing device, examining table, postpartum ward, space for sterilization/presence of the autoclave or puppinel, emergency cesarean section room and blood transfusion station) [1]. The unit price and the number of stockouts of each drug during the last 6 months were also estimated.
If the HFs provided all the seven basic signal functions during the survey or 3 months prior, the basic EmOC was considered available, but if all nine defined signal functions were provided, the comprehensive EmOC was available.
The quality of basic EmOC and comprehensive EmOC was based on the criteria used in recent research conducted in the DRC [18]. The criteria for the quality of basic EmOC were as follows: availability of essential medicines and consumables; availability of material and equipment; the presence of at least one health professional trained in basic EmOC for 2 years before the survey; and availability of delivery and data reporting tools. Meanwhile, the criteria for the quality of comprehensive EmOC were the following: diagnostic capacity to perform blood grouping and cross-tabulation tests, availability of essential medicines and consumables; availability of material and equipment; the presence of at least one health professional trained in comprehensive EmOC, anesthesia or surgery for 2 years before the survey; and availability of delivery and data reporting tools.
2.6. Data analyses
Collected data were recorded on Microsoft Excel® 2016 files [24]. All statistical data were analyzed using the R® 4.0.0 [25]. The map of Kasai Provincial Health Division was drawn using the free software QGIS 3.4 [26]. Considering that the study consisted mainly of discrete quantitative variables, they were presented as proportions (%). The relationship of the availability and quality of EmOC with the different types of HF was assessed by Pearson’s chi-squared test or chi-square independence test. We used an alpha significance level of 0.05 to test all hypotheses.
3. Results
Among the HFs (GRHs and HCs) surveyed, 32 were public (65.2%), 15 were private (30.1%), and two belonged to mission sectors. We had interviewed 247 health workers.
3.1. Access to healthcare
3.2. Geographical accessibility of the population to HCs
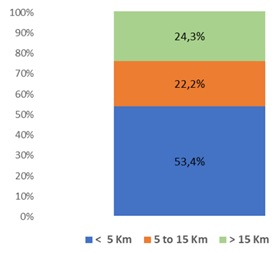
The geographical accessibility was overall insufficient. Approximately half of the population lived more than 5 km away from the HF or far from a natural obstacle (rivers, mountains, etc.) that prevented a person from reaching the HC within 1 hour walk (Figure 2), making it difficult for the population to access the HFs.
3.3. Affordability of medicines and medical services
With the exception of the admission costs and essential drugs, the prices of medical services were unaffordable for the population (Table 1).
3.4. Availability and sustainability of infrastructure with RMNCH services
3.5. Availability of infrastructure with RMNCH services
Infrastructures with RMNCH services were available in only one-third of the surveyed HFs. The least available RMNCH service was space for sterilization or presence of the autoclave or puppinel (27.1%), followed by emergency cesarean section room (20.2%) and transfusion station (19.8%) (Table 2). The availability of infrastructures was significantly higher in private HF than in public HF (Pearson’s chi-squared test; p < 0.001).
|
N° |
Medicines/medical acts |
Unit Price (in USD) |
Affordability per treatment unit (in days) a |
|
1 |
Oxytocin injection 10 IU, 1 ml |
0.09 |
0.1 |
|
2 |
Misoprostol tablet, 200 μg |
0.13 |
0.2 |
|
3 |
Magnesium sulfate injection, 500 mg/ml |
0.29 |
0.3 |
|
4 |
Admission costs in HCs |
0.6 |
0.7 |
|
5 |
Admission costs in GRHs |
1 |
1.2 |
|
6 |
Blood transfusion |
6.04 |
7.1 |
|
7 |
Eutocic childbirth |
4.72 |
5.6 |
|
8 |
Distocic childbirth |
15.1 |
17.8 |
|
9 |
Cesarean section |
36.12 |
42.5 |
GRH: General Referral Hospital, HC: Health Centre.
aAffordability per treatment unit was calculated according to the number of days needed to pay for the standard essential medicines or medical services and the population’s lowest daily income (approximately 0.85$ per person). Medicines or medical services costing more than the daily income were considered unaffordable.
Table 1: Affordability of medicines and medical services in the HFs of Kasai Health Division, 2019.
|
N° |
RMNCH services |
Number1 |
% |
|
1 |
Delivery room with a delivery bed with newborn corner, water drainage and soak away |
15 |
29.7 |
|
2 |
Incinerator |
14 |
28.1 |
|
3 |
Light source |
15 |
30.4 |
|
4 |
Labor room |
14 |
29.2 |
|
5 |
Space for prenatal, postnatal and preschool consultations |
16 |
31.8 |
|
6 |
Safe water source or hand washing device |
14 |
29.5 |
|
7 |
Examining table |
14 |
27.8 |
|
8 |
Postpartum ward |
14 |
28.9 |
|
9 |
Space for sterilization/presence of the autoclave or puppinel |
13 |
27.1 |
1A total of 49 HFs were surveyed, comprising 18 GRHs and 31 HCs.
Table 2: Availability of infrastructure with RMNCH services in the HFs of Kasai Health Division, 2019.
3.6. Equipment/healthcare and travel materials of RMNCH services
3.7. Sustainability of infrastructure with RMNCH services
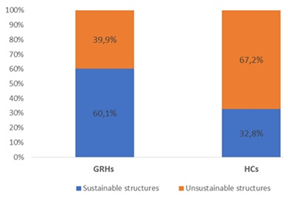
Approximately 80% of the infrastructures of surveyed HFs were unsustainable (Figure 3). In addition, private HFs had more sustainable infrastructures than public HFs (Pearson’s chi-squared test; p < 0.0001).
An infrastructure was considered sustainable if it had at least 11 RMNCH services (delivery room with delivery bed with newborn corner, water drainage and soakaway, incinerator, light source, labor room, space for prenatal, postnatal and preschool consultations, safe water source, or handwashing device, examining table, postpartum ward, space for sterilization/presence of the autoclave or puppinel, emergency cesarean section room and blood transfusion station)
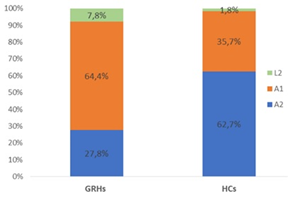
3.8. Qualification and training of health professionals in RMNCH package
Approximately half of the healthcare providers were less skilled (nurses’ level A2) (Figure 4). Among them, 18% were trained in RMNCH package, and only 14% of the skilled nurses (nurses’ level A1) were also midwives. The qualification and training of health professionals in RMNCH package were not significantly different between private and public HFs (p > 0.05).
Figure 4: Qualification of health professionals in the GRHs/HCs of Kasai Health Division, 2019. Nurses’ level A2: nurses with secondary level education, nurses’ level A1: nurses with undergraduate university level, licensed nurses: nurses with completed university level. GRHs (N=90) and HCs (N=157).
3.9. Availability of essential medicines in sufficient stock of RMNCH services
Between 70% and 90% of the surveyed HFs did not have minimum equipment/healthcare materials of RMNCH services (Table 3).
The equipment with the least number was negative pressure vacuum with a suction probe (9.7%), followed by warm table or table with heat source (9.9%), flexible gynecological examination light (10.5%) and suction cup and/or forceps (15%). Only one GRH had an ambulance to transport emergency patients (Table 3). Private HFs had significantly greater availability of equipment than public HFs (Pearson’s chi-squared test; p < 0.0001).
The least essential medicines were silver nitrate (1%) or argyrol (0.5%) (16.6%), vitamin K1 ampoule 1 mg/ml (17.8%), papaverine, N-butylscopolamine (20.2%) and chlorine-based disinfectants (19.5%). Only 43.2% of HFs had parenteral anticonvulsants (diazepam, magnesium sulfate, and calcium gluconate), but almost 70% had uterotonic drugs (oxytocin, misoprostol) and parenteral antibiotics (ampicillin, gentamicin) (Table 4).
|
N° |
Equipment/healthcare and travel materials |
Number1 |
% |
|
1 |
Flexible gynecological examination light |
5 |
10.5 |
|
2 |
Warm table or table with heat source |
5 |
9.9 |
|
3 |
Baby scale |
15 |
31.4 |
|
4 |
Negative pressure vacuum with a suction probe |
5 |
9.7 |
|
5 |
Sterilizer or pressure cooker |
17 |
35.5 |
|
6 |
Blood pressure monitor and stethoscope |
15 |
31.6 |
|
7 |
Obstetric stethoscope (foetoscope) |
18 |
37.1 |
|
8 |
Single-use detachable pear |
17 |
35.7 |
|
9 |
Self-inflatable ventilation bag (250–500 ml capacity) and face mask N°0 and N°1 |
6 |
11.3 |
|
10 |
Delivery box |
15 |
30.2 |
|
11 |
Box for examination/suture of the vagina and cervix |
15 |
29.8 |
|
12 |
Box of vaginal specula of different sizes (small, medium, and large) |
12 |
25.1 |
|
13 |
Suction cup and/or forceps |
7 |
15 |
|
14 |
Ambulance |
1 |
0.02 |
1A total of 49 HFs were surveyed, comprising 18 GRHs and 31 HCs.
Table 3: Equipment/healthcare and travel materials of RMNCH services in the HFs of Kasai Health Division, 2019
|
N° |
Availability of essential medicines |
Number1 |
% |
|
1 |
Silver nitrate (1%) or argyrol (0.5%) |
8 |
16.6 |
|
2 |
Vitamin K1 ampoule 1 mg/ml |
9 |
17.8 |
|
3 |
Papaverine, N-butylscopolamine |
12 |
20.2 |
|
4 |
Chlorine-based disinfectants |
12 |
19.5 |
|
5 |
Hand disinfectants |
20 |
40 |
|
6 |
Combinations of artesunate, quinine |
20 |
41.3 |
|
7 |
Antiseptic solutions |
20 |
41.7 |
|
8 |
Diazepam, magnesium sulfate, calcium gluconate |
21 |
43.2 |
|
9 |
Ampicillin, gentamicin |
33 |
67.4 |
|
10 |
Physiological saline 0.9%, Ringer’s lactate, glucose solution 50% |
32 |
64.9 |
|
11 |
Paracetamol |
33 |
67.5 |
|
12 |
Vitamin A, Folic acid |
33 |
67.1 |
|
13 |
Oxytocin/misoprostol |
33 |
68.2 |
1A total of 49 HFs were surveyed, comprising 18 GRHs and 31 HCs.
Table 4: Availability of essential medicines of RMNCH services in the HFs of Kasai Health Division, 2019.
3.10. Availability, the content and the completion of delivery, and data reporting tools of RMNCH services
Almost all of the surveyed HFs (approximately 95%) had delivery and data reporting tools. This information was updated and well maintained. The staff periodically reviewed patient records (Table 5).
|
N° |
Availability of reporting tools |
Number1 |
% |
|
1 |
Are the tools (partographs, sheets and registers) available? |
46 |
94.7 |
|
2 |
Are they updated and well maintained? |
36 |
74.3 |
|
3 |
Are all the columns filled? |
36 |
73.5 |
|
4 |
Is there a column for reporting the diagnoses? |
36 |
73.8 |
|
5 |
Are diagnoses reported regularly in this column? |
39 |
79.4 |
|
6 |
Is there a column for reporting the treatment? |
40 |
81.5 |
|
7 |
Is there a column for reporting obstetrical and neonatal complications? |
38 |
77.9 |
|
8 |
Are patient records periodically reviewed by the staff? |
36 |
77.7 |
1A total of 49 HFs were surveyed including 18 GRHs and 31 HCs.
Table 5: Availability of reporting tools of RMNCH services in the HFs of Kasai Health Division, 2019.
3.11. Availability and quality of EmOC
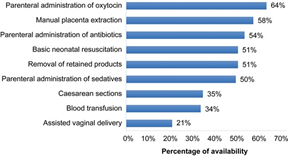
Parenteral administration of oxytocin was the most performed signal function (63.6%), followed by manual placenta extraction (57.8%) and parenteral antibiotic administration (53.9%). The least performed signal functions was assisted vaginal delivery (20.9%), followed by parenteral sedative administration (49.8%), basic neonatal resuscitation (50.6%) and retained product removal (50.8%) (Figure 5).
Among the surveyed HFs, 11.8% provided basic EmOC, and only 7.6% offered comprehensive EmOC (Fig. 5). Private HFs provided better basic and comprehensive EmOC than public HF (Pearson’s chi-squared test; p < 0.001). According to the quality criteria, none of the surveyed HFs provided high-quality basic or comprehensive EmOC.
Basic EmOC was available if HF provided the first six and the last signal functions, comprehensive EmOC was available if HF provided all 11 signal functions.
4. Discussion
In Kasai province, the population (nearly 50%) generally had limited or poor geographical access to RMNCH services and could not afford most of the medical services because of high prices.
Only 11.8% of HFs offered basic EmOC, and only 7.6% could provide comprehensive EmOC; in addition, none of the surveyed HFs provided high-quality basic or comprehensive EmOC.
The insufficiency of necessary inputs and personnel to perform RMNCH services in most of the HFs explain the low availability and quality of the EmOC. Only one-third of the surveyed HFs had available infrastructures with RMNCH services, and nearly 80% were unsustainable. Almost half of the healthcare providers were inadequately skilled, and majority of them were not trained in RMNCH package. Only 10%–30% of the surveyed HFs had minimum equipment/healthcare materials of RMNCH services. Only one facility had an ambulance to transport patients in an emergency. In the last 6 months, 40%–80% of the surveyed HFs did not have a category of essential medicines, consumables, and small medical equipment. Conversely, almost all the surveyed facilities had delivery and data reporting tools, which were updated and well maintained.
To our knowledge, this survey is the first to be conducted in Kasai province in over 20 years. Another strength of this study is that it was conducted in all 18 GRHs of this province, thereby acquiring crucial information on the RMNCH in these facilities. The survey also used a standardized WHO and HAI methodology, allowing us to assess affordability [21]. The other items collected during the survey were adapted from the list of interventions proposed by RMNCH experts [1, 23].
However, our study presented several limitations that where clearly identified and partially resolved. The study was conducted in only 31 HCs, representing only 20% of the HFs in Kasai province. However, the sampling (stratified random sampling) used allowed us to ensure the representativeness of the HCs in all axes of each HZ. As part of continuity of care, a survey should also be conducted at the family/community level. Unfortunately, we did not conduct a survey at this level because we assumed that such survey was already performed at this level.
Other studies also reported poor geographic access to RMNCH services and unaffordability of essential drugs and medical services. Access to RMNCH services was impeded by affordability and the distance of the patient's residence from the HF (longest travel times) [27]. Other studies highlighted that long distances associated with poor transportation conditions, can be potential key barriers to RMNCH service utilization [28, 29]. Limited access to RMNCH services leads to late identification and referral of high-risk pregnancies [13].
Our study showed that EmOC is less available in the HFs of Kasai province. Basic and comprehensive EmOC were offered by only 11.8% and 7.6% of HFs, respectively, and none provided high-quality EmOC. These results are largely consistent with those of other studies conducted in the DRC [15, 16, 18, 30]. The present study revealed that approximately 40%–50% of HFs did not provide any signal functions of basic EmOC. The least performed signal functions were sedative administration, basic neonatal resuscitation, retained product removal and assisted vaginal delivery, consistent with other studies [14, 18]. The lack of such signal functions may explain the poor management of the HFs in dealing with preeclampsia/eclampsia and preventing postpartum hemorrhages, and neonatal asphyxia, which are main causes of maternal and neonatal mortality [11, 14, 18].
The most common reasons of not performing basic EmOC signal functions may be unavailability and unsustainability of infrastructures, inadequate skills and the lack of training of personnel in RMNCH package, insufficiency of equipment and healthcare materials, lack of essential medicines, and unavailability of delivery and data reporting tools [14, 18]. Almost all of these reasons were found in our study.
A study conducted in rural India showed that improved availability and sustainable infrastructures of public HFs could lead to increased utilization of health services [29]. Basic sustainable infrastructures can also play an important role in improving access to RMNCH services [31].
Skilled and trained healthcare providers can recognize and manage rapidly high-risk pregnancy; thus, they could prevent delivery complications and maternal and newborn morbidity and mortality [13, 29, 32].
Furthermore, Patel et al. observed that the availability of quality equipment/healthcare materials strongly encourages women to give birth in public HFs [29], similar to studies elsewhere; Cole-Ceesay et al. also showed that supplying adequate new equipment and materials could help improve emergency management during pregnancy, childbirth, infancy and childhood [32].
Our study revealed that essential medicines, consumables, and small medical equipment were unavailable in nearly 40%–80% surveyed HFs during a period of 6 months, consistent with other studies [13, 29, 32]. The availability of essential emergency medicines such oxytocin, misoprostol, magnesium sulfate, antibiotics, and fluids could prevent postpartum hemorrhage, eclampsia and sepsis, which are the common causes of maternal and child mortality in low-income countries [32].
Contrary to a previous study where data reporting was neither complete nor accurate [33], our study observed that delivery and data reporting tools were available, updated and well maintained in almost all the surveyed HFs. The difference may be explained by the fact that most of the HFs in Kasai province regularly received the data collection tool from a financial partner, which also supervised their filling.
5. Conclusions
In Kasai province, only half of the population of surveyed HFs had geographical access to RMNCH services, and the medical services were mostly unaffordable. In addition, both basic and comprehensive EmOC were less available and had a low quality because the HFs had unsustainable infrastructures, less skilled personnel, frequent stockouts of essential emergency medicines and blatant lack of equipment/healthcare materials. Therefore, rehabilitation of infrastructure, dotation of equipment, regular supply of medicines, and strengthening of human resource capacity are necessary to improve EmOC coverage.
6. Declarations
6.1. Acknowledgments
We thank all persons, who assisted the drafting of this article. The authors thank also Professor Ntabe Namegabe for coordinating the data collection for this research. We also acknowledge the field workers.
6.2. Funding
The project was funded by the Swedish Government, through its International Development Cooperation Agency, "SIDA” with grant number: 11836. The founder had no role in study design, data collection and analysis, in the writing of paper, and decision to publish it.
6.3. Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
6.4. Ethics approval and consent to participate
This research was reviewed and approved by DRC Protestant University ethics committee (ref: CEUPC 0059). The research team obtained informed written consent for each participant. Data were collected anonymously after obtaining authorizations from provincial health and HZ authorities prior to the survey
Conflicts of Interest
There are no conflicts of interest.
Author’s Contributions
Britou Ndela, Philippe Ngwala, Adrien N’siala, and Bien-Aimé Mandja designed the study, supervised all aspects of study implementation, wrote and edited the manuscript; Nancy Ntatukidi, Harmonie Bokole and Jean-Jacques Masumbuku collected the data; Albert Kalonji, Felix Minuku, and Ngoma Miezi Kintaudi guided data analysis; Britou Ndela and Bien-Aimé Mandja performed data curation and conducted data analysis; Albert Kalonji, Felix Minuku, and Ngoma Miezi Kintaudi developed figures and tables and participated in writing and editing the manuscript. Nancy Ntatukidi, Harmonie Bokole and Jean-Jacques Masumbuku participated also in writing and editing the manuscript.
References
- Black R, Laxminarayan R, Temmerman M, Walker N, editors. Disease control priorities, (volume 2): reproductive, maternal, newborn, and child health. World Bank Publications; 2016 Apr 11.
- World Health Organization. Trends in maternal mortality: 1990-2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2015.
- Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet 388 (2016): 3027–3035.
- You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet 386 (2015): 2275–2286.
- National Statistics Institute (NSI). Multiple Indicators Cluster Survey (MICS), 2017-2018, investigation results report. Kinshasa, Democratic Republic of the Congo. 2019.
- You D, Hug L, Ejdemyr S, Beise J. Levels and trends in child mortality: Report 2015. Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation. U N Child Fund N Y. 2015.
- Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE et al., Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 385 (2015): 430–440.
- Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Group BCSS. How many child deaths can we prevent this year? Lancet 362 (2003): 65–71.
- Lee AC, Cousens S, Wall SN, Niermeyer S, Darmstadt GL, Carlo WA, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health 11 (2011): S12.
- Standards for improving quality of maternal and newborn care in health facilities. 2016.
- Mirkuzie AH, Sisay MM, Reta AT, Bedane MM. Current evidence on basic emergency obstetric and newborn care services in Addis Ababa, Ethiopia; a cross sectional study. BMC Preg Childbirth 14 (2014): 1–8.
- Friberg IK, Kinney MV, Lawn JE, Kerber KJ, Odubanjo MO, Bergh AM, et al. Sub-Saharan Africa’s mothers, newborns, and children: how many lives could be saved with targeted health interventions? PLOS Med 7 (2010): e1000295.
- Bhutta ZA, Cabral S, Chan CW, Keenan WJ. Reducing maternal, newborn, and infant mortality globally: an integrated action agenda. Int J Gynecol Obstet 119 (2012):13–17.
- Teshoma KR, Eticha CT. Availability and quality of emergency obstetric and newborn care service in Dire Dawa, Ethiopia. J Women’s Health Care 5 (2016).
- Casey SE, Mitchell KT, Amisi IM, Haliza MM, Aveledi B, Kalenga P, et al. Use of facility assessment data to improve reproductive health service delivery in the Democratic Republic of the Congo. Confl Health 3 (2009):12.
- Ministry of Public Health., United Nations Fund Population, World Health Organization, Averting Maternal Death, and Disability. [Emergency obstetric and neonatal care in health facilities in the DRC: needs assessment in three provinces. Investigation report: DRC]. 2012.
- Ministry of Public Health. Mapping of maternal, newborn and child health interventions and stakeholders including family planning in DR Congo DRC. 2012.
- Mpunga Mukendi D, Chenge F, Mapatano MA, Criel B, Wembodinga G. Distribution and quality of emergency obstetric care service delivery in the Democratic Republic of the Congo: it is time to improve regulatory mechanisms. Reprod Health 16 (2019): 102.
- Kasai DPS. Operational action plan 2019, Ministry of Public Health, Democratic Republic of Congo, 2019.
- Maina J, Ouma PO, Macharia PM, Alegana VA, Mitto B, Fall IS, et al. A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Sci Data 6 (2019): 1–8.
- Measuring medicine prices, availability, affordability and price components. World Health Organization. 2008.
- Central Bank of Congo. Exchange rates 2019.
- Interagency list of medical devices for essential interventions for reproductive, maternal, newborn and child health. 2016.
- Microsoft Corporation. Microsoft Excel [Internet]. 2018.
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2019.
- QGIS Development Team. QGIS Geographic Information System. Open Source Geospatial Foundation Project. 2019.
- Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res 12 (2012):120.
- Yao J, Murray AT, Agadjanian V. A geographical perspective on access to sexual and reproductive health care for women in rural Africa. Soc Sci Med 96 (2013): 60–68.
- Patel R, Ladusingh L. Do physical proximity and availability of adequate infrastructure at public health facility increase institutional delivery? A three level hierarchical model approach. PLOS ONE 10 (2015): e0144352.
- Casey SE, Chynoweth SK, Cornier N, Gallagher MC, Wheeler EE. Progress and gaps in reproductive health services in three humanitarian settings: mixed-methods case studies. Confl Health 9 (2015): S3.
- Fay M, Leipziger D, Wodon Q, Yepes T. Achieving child-health-related millennium development Goals: the role of infrastructure. World Dev 33 (2005): 1267–1284.
- Cole-Ceesay R, Cherian M, Sonko A, Shivute N, Cham M, Davis M, et al. Strengthening the emergency healthcare system for mothers and children in The Gambia. Reprod Health 7 (2010): 21.
- Mate KS, Bennett B, Mphatswe W, Barker P, Rollins N. Challenges for routine health system data management in a large public programme to prevent mother-to-child HIV transmission in South Africa. PLOS ONE 4 (2009): e5483.
Supporting Information
S1 Dataset. The datasets supporting the conclusions of this article. (XLSX)
S1 Appendix. STROBE guideline. A guideline includes 22 items deemed essential for transparent reporting of an observational study. (DOCX)
S2 Appendix._Questionnaire_French. Survey questionnaire in French. (DOCX)
S3 Appendix._Questionnaire_English. Survey questionnaire in English. (DOCX)



 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 