Comparison of Specific Antibody Levels among Pregnant Women: A Case- Control Study
Dr. Bidisha Chakma1, Prof. Dr. Tripti Rani Das2, Dr. Shah Noor Sharmin3, Dr. Jinat Fatema4, Farah Noor5, Dr. Sabiha Islam6*, Dr. Dipika Majumder7, Dr. Tanzina Iveen Chowdhury8
1Associate Professor, Department of Obstetrics & Gynecology, Bangladesh Medical University (BMU), Dhaka, Bangladesh.
2Professor, Department of Obstetrics & Gynecology, BMU. Dhaka, Bangladesh.
3Medical officer, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
4Assistant Professor, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
5Assistant Professor, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
6Associate Professor, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
7Medical Officer, Department of Obstetrics & Gynecology, Madaripur, Bangladesh.
8Assistant Professor, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
*Corresponding author: Dr. Sabiha Islam, Associate Professor, Department of Obstetrics & Gynecology, BMU, Dhaka, Bangladesh.
Received: 30 May 2025; Accepted: 10 June 2025; Published: 12 June 2025
Article Information
Citation: Dr. Bidisha Chakma, Prof. Dr. Tripti Rani Das, Dr. Shah Noor Sharmin, Dr. Jinat Fatema, Farah Noor, Dr. Sabiha Islam, Dr. Dipika Majumder, Dr. Tanzina Iveen Chowdhury. Comparison of Specific Antibody Levels among Pregnant Women: A Case-Control Study. Obstetrics and Gynecology Research. 8 (2025): 96-102.
View / Download Pdf Share at FacebookAbstract
Background:
Disorders of pregnancy, with preeclampsia, persists an important cause of maternal and perinatal morbidity and mortality worldwide, with disproportionately high burdens experiential in low and middle-income countries such as Bangladesh. Emerging indication suggests a potential immunological basismainly the role of antiphospholipid antibodies like anticardiolipin IgMin the pathogenesis of these complications, meriting greater care in regional maternal healthcare policies.
Aim:
To find out the association between specific antibody levels among pregnant women.
Materials and Methods:
A case-control study was conducted at Bangladesh Medical University (BMU), Dhaka, from July 2021 to June 2022, including78 pregnant women at <20->30 weeks of gestation. Participants were selected purposively based on specific inclusion criteria. Socio-demographic, clinical, and biochemical data, with serum anticardiolipin IgM levels, was collected. Data were analyzed using SPSS v26, applying Fisher's Exact Test for Chi-square, with p<0.05 considered significant. Ethical approval and informed consent were taken.
Results:
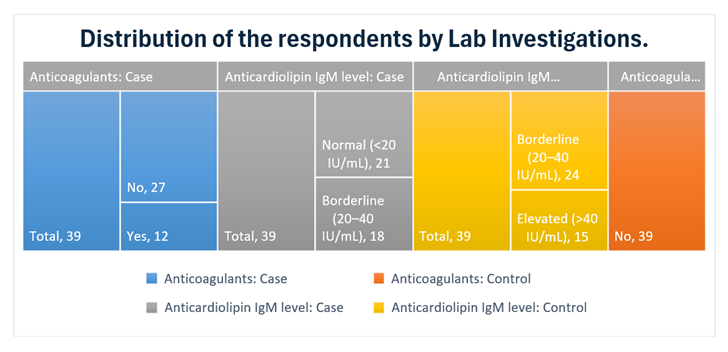
Out of 78 participants, 12 cases used anticoagulants while none among controls did. In the case group, anticardiolipin IgM levels were normal in 21 and borderline in 18 individuals. Among controls, 24 had borderline and 15 had elevated levels. These results recommend a variance in antibody level distribution and anticoagulant use between the groups.
Conclusion:
High anticardiolipin IgM antibodies may underwrite to hypertensive disorders in pregnancy, even in the absence of classic autoimmune profiles. Broader aPL screening and initial intervention, with anticoagulant therapy, may help decrease adverse outcomes. These results warrant more investigation in greater, diverse populations.
Keywords
<p>Preeclampsia; Anticardiolipin IgM; Hypertensive Disorders; Fisher's Exact Test Pregnant women</p>
Article Details
INTRODUCTION
Antiphospholipid antibodies (aPL) are a heterogeneous cluster of autoantibodies focusedcompared to phospholipid-binding proteins [20]. Their existence has been reliablyrelated with a spectrum of opposing pregnancy outcomes [2, 3], with early and late pregnancy loss, stillbirth, and placental insufficiency [8, 6]. These antibodies, which comprise lupus anticoagulant (LA) and anticardiolipin antibodies (aCL), have been noticed in both the general obstetric population and in women undergoingnumerous pregnancy difficulties [1, 2].
The link between aPL and recurrent pregnancy loss (RPL) is fixed [4, 5, 6, 10, 21, 22], with some studies found high potential fetal loss rates in untreated pregnancies of women with RPL and aPL [6]. Furthermore, the incidence of aPL contributes to pregnancy loss in women with systemic lupus erythematosus (SLE) [7]. Outside pregnancy loss, aPL have been progressivelydocumented as a risk factor for severe pregnancy problems such as early-onset preeclampsia [11, 12, 13].
The exact mechanisms by which aPLprime to these adverse outcomes are multifaceted and not fully unwritten. Nevertheless, planned mechanisms comprise the initiation of endothelial cell tissue factor action, possiblyactivating a prothrombotic state within the placental vasculature [9]. Variations in aPL levels throughout pregnancy have also been detected, which may influence coagulation initiation [19]. The clinical significance of aPL is officiallystandard in the universalsorting criteria for certain antiphospholipid syndrome (APS), which contains obstetric morbidity [15]. In spite of this gratitude, significant contests remain in the setting and clarification of aPL testing across different laboratories [16, 17, 18].
While a broad range of aPL isotypes (IgG, IgM, IgA) and specificities, counting antibodies focused against β2-glycoprotein I (β2GPI) [6], have been examined in the setting of pregnancy problems, this case-control study exactly aims to compare anticardiolipin IgM levels between pregnant women with and without certain pregnancy outcomes. Certain the well-documented associations between aPL and adverse pregnancy outcomes, this study seeks to further explain the potential role of IgM levels in these conditions.
Materials and Methods:
This case-control study was conducted in the Department of Obstetrics and Gynecology at the BMU, Dhaka, from July 2021 to June 2022. A total of 78 pregnant women between <20->30+ weeks of gestation were purposively selected and separated into two groups: 39 with cases and 39 with controls. Inclusion criteria were age <20-30+ years. Exclusion criteria included chronic hypertension, autoimmune disorders, infectious diseases, and refusal to consent.
Sociodemographic, anthropometric, and clinical data were collected by means of a semi-structured questionnaire. Blood pressure and urine protein levels were measured, and 5 ml of venous blood was collected for serum anticardiolipin IgM antibody estimation using Immunometric Enzyme Immunoassay. Samples were processed at the BMU laboratory.Data were analyzed using SPSS version 26. Descriptive statistics, Fisher's Exact Test for Chi-square were pragmatic, with a p-value <0.05 measured statistically significant. Ethical consent was taken from the BMU review board, and knowledgeable written accord was taken from all participants. Data privacy and participant truths were firmlyupheld.
Results:
A total of 78 pregnant women were registered, with 39 in each group (case and control). Anticoagulant use was stated only among the case group, with 12 using and 27 not using anticoagulants. None of the control groups reported anticoagulant use.
Concerning anticardiolipin IgM levels, 21 cases revealed normal levels (<20 IU/mL), while 18 had borderline levels (20-40 IU/mL). Between the control group, 24 had borderline levels and 15 had elevated levels (>40 IU/mL). These results specify that elevated anticardiolipin IgM levels were more prevalent in the control group, where anticoagulant use was observed completely among cases.
Table 1: Distribution of the respondents by socio-demographic factors
|
Age category |
|||
|
Group |
Age |
Frequency |
Percent |
|
Case |
20-30 |
23 |
59 |
|
30+ |
16 |
41 |
|
|
Control |
20-30 |
20 |
51.3 |
|
30+ |
19 |
48.7 |
|
|
Educational Status |
|||
|
Case |
No formal education |
5 |
12.8 |
|
Primary |
12 |
30.8 |
|
|
Secondary |
22 |
56.4 |
|
|
Control |
Secondary |
22 |
56.4 |
|
Higher secondary and Above |
17 |
43.6 |
|
|
Occupation |
|||
|
Case |
Housewife |
29 |
74.4 |
|
Service holder |
10 |
25.6 |
|
|
Control |
Service holder |
11 |
28.2 |
|
Business |
11 |
28.2 |
|
|
Others |
17 |
43.6 |
|
|
Monthly family income (in BDT) |
|||
|
Case |
<20,000 |
9 |
23.1 |
|
20,000–40,000 |
30 |
76.9 |
|
|
Control |
20,000–40,000 |
26 |
66.7 |
|
|
>40,000 |
13 |
33.3 |
|
Total |
78 |
100 |
|
Table 1 shows that the most respondents were aged 20–30 years (59.0% cases, 51.3% controls). Among cases, 56.4% had secondary education, while 43.6% of controls had higher secondary or above. The majority of cases were housewives (74.4%), whereas controls were service holders (28.2%), businesspersons (28.2%), or others (43.6%). Monthly income ranged mostly between 20,000–40,000 BDT (76.9% cases, 66.7% controls); 33.3% of controls earned over 40,000 BDT. These characteristics may influence the antibody level differences observed between groups.
Table 2: Distribution of the respondents by pregnancy related information
|
Group |
Parity status: |
Frequency |
Percent |
|
|
Parity status |
||||
|
Case |
Primipara |
31 |
79.5 |
|
|
Multipara |
8 |
20.5 |
||
|
Total |
39 |
100 |
||
|
Control |
Multipara |
39 |
100 |
|
|
Gestational age |
||||
|
Case |
<20 weeks |
2 |
5.1 |
|
|
20-30 weeks |
28 |
71.8 |
||
|
>30 Weeks |
9 |
23.1 |
||
|
Total |
39 |
100 |
||
|
Control |
>30 Weeks |
39 |
100 |
|
|
Presence of pregnancy complications in the current pregnancy: |
||||
|
Case |
Normal |
39 |
100 |
|
|
Control |
Normal |
11 |
28.2 |
|
|
|
Hypertensive |
28 |
71.8 |
|
|
Total |
39 |
100 |
||
Table 2 summarizes pregnancy-related information of the respondents. Among cases, 79.5% were primipara and 20.5% multipara, whereas all controls (100%) were multipara. Most cases (71.8%) were between 20–30 weeks of gestation, while all controls were beyond 30 weeks. All case participants had normal pregnancies, in contrast to the control group, where 71.8% had hypertension-related complications and only 28.2% had normal pregnancies.
Table 3: Distribution of the respondents by history of comorbidities.
|
Autoimmune Disorders |
Frequency |
Percent |
||
|
Case |
SLE |
2 |
5.1 |
|
|
antiphospholipid syndrome |
3 |
7.7 |
||
|
Other |
5 |
12.8 |
||
|
No |
29 |
74.4 |
||
|
Total |
39 |
100 |
||
|
Control |
No |
39 |
100 |
|
|
Thromboembolic Disorders |
||||
|
Case |
Yes |
3 |
7.7 |
|
|
No |
36 |
92.3 |
||
|
Total |
39 |
100 |
||
|
Control |
No |
39 |
100 |
|
|
Blood Pressure |
||||
|
Case |
Hypertensive |
39 |
100 |
|
|
Control |
Normal |
39 |
100 |
|
|
IUGR |
||||
|
Case |
Yes |
14 |
35.9 |
|
|
No |
25 |
64.1 |
||
|
Total |
39 |
100 |
||
|
Control |
No |
39 |
100 |
|
Table 3 illustrates the respondents’ history of comorbidities. Among cases, 25.6% had autoimmune disorders5.1% with SLE, 7.7% with antiphospholipid syndrome, and 12.8% with other conditionswhile all controls (100%) reported none. Thromboembolic disorders were present in 7.7% of cases, but none in controls. All cases were hypertensive, whereas all controls had normal blood pressure. Intrauterine growth restriction (IUGR) was observed in 35.9% of cases and in none of the controls.
Figure 1 displays that among the case group, 12 respondents reported using anticoagulants, while 27 did not. In the control group, none reported using anticoagulants. Regarding anticardiolipin IgM levels, 21 cases had normal levels (<20 IU/mL) and 18 had borderline levels (20–40 IU/mL). In contrast, among the controls, 24 had borderline levels and 15 had elevated levels (>40 IU/mL).
Table 4: Association between case and control on normal and preeclampsia patients
|
Group |
IgM level |
Total |
p-Value |
|
|
Normal |
Preeclampsia |
|
||
|
Case |
20 |
19 |
39 |
|
|
Control |
9 |
30 |
39 |
0 |
Table 4 explains that there was a significant association between case and control on normal and preeclampsia (p=0.000)
Table 5: Association between case and control with IgM category
|
IgM category |
Group |
p-value |
95% Confidence Interval |
OR |
|||
|
Case |
Control |
||||||
|
Lower |
Upper |
||||||
|
2.934 |
41.236 |
11 |
|||||
|
Normal |
0 |
9 |
.000 f |
||||
|
Preeclampsia |
20 |
2 |
|||||
|
Total |
20 |
11 |
31 |
||||
*1 cell (25.0%) has expected count less than 5. *f- Fisher's Exact Test
Table 5 reveals that there was a significant association between case and control and IgM category (p=0.000). It also explores that there are 11 times (OR=11) higher risk to develop preeclampsia among the case than control group.
Discussion:
This case-control study assessed the association between anticardiolipin IgM antibody levels and pregnancy-related problems among 78 pregnant women. The study exposed that high anticardiolipin IgM levels were more communal among the control group, while anticoagulant practice was exclusive to the case group. These results proposed significant insights into the immunological changes between women with and without hypertensive problemsthroughout pregnancy.
Antiphospholipid antibodies, mainly anticardiolipin IgM, have long been concerned in pregnancy-related difficulties, with preeclampsia, recurrent miscarriage, and intrauterine growth restriction [1, 2, 6, 11]. Remarkably, in the study, none of the controls (who mostly had hypertensive disorders) stated anticoagulant use, yet they showed significantly advanced levels of anticardiolipin IgM. This recommends that elevated antibody levels may be related with, or possibly precede, clinical appearances of hypertensive disorders in pregnancy, mainly when not alleviated by anticoagulation therapy.
Socio-demographic characteristics may partlyclarify the antibody level changes found. An advanced percentage of controls had higher secondary or above education and informed more expanded occupations with relatively higher incomes. These factors might affect access to healthcare and health-seeking behavior, possiblypostponing diagnosis and intervention [2, 5].
From the obstetric history, a significant difference was originated in parity and gestational age. Maximum cases were primiparous and in earlier gestational weeks, while all controls were multiparous and outside 30 weeks. This inequality is clinically appropriate, as aPL-related complications often manifest in early-to-mid gestation [4, 6, 19]. It is probable that women in the case group were diagnosed earlier and managed on time, counting with anticoagulants, actually clearing up their more promising aCL IgM profiles.
The association between comorbid conditions and anticardiolipin antibody levels was also notable. Autoimmune disorders, with systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS), were originatecompletely among the case group, reliable with recognized literature display elevated aPL prevalence in autoimmune populations [7, 14, 20]. Moreover, thrombo-embolic disorders and IUGR well-known significances of aPL activity were also exclusive to the case group [6, 8, 9]. This resultbring into line with studies reportage endothelial dysfunction and prothrombotic states made by aPL, particularly in the presence of autoimmune comorbidities [9, 13].
Illogically, despite their autoimmune background and comorbidities, cases had predominantly normal or borderline anticardiolipin IgM levels, possibly due to effective anticoagulant use. Anticoagulant therapy, particularly low-dose aspirin and heparin, has been exposed to decrease antibody-mediated pregnancy problems [10, 12]. Our outcomessupport this, as anticoagulant users were completely in the case group and had no elevated IgM levels.
Equally, the control groupdevoid of autoimmune disease and anticoagulant therapyhad suggestively more elevated IgM levels and hypertensive disorders, signifying an under-recognized population possibly at risk. This opinionrecommends anessential to screen for antiphospholipid antibodies beyond usually defined high-risk groups, as suggested by current literature [16, 17].
The statistically significant association between case/control status and both preeclampsia (p=0.000) and IgM levels further highlights the potential pathophysiological role of aPL in hypertensive pregnancy disorders. While the conventional view associates aPL with thrombotic miscarriage, their influence to late-onset problems like preeclampsia is gaining credit [11, 13, 18].
This study, has limitations. The sample size is modest, and selection was purposive, restrictive generalizability. The study attentive solely on anticardiolipin IgM, without other isotypes (IgG, IgA) and β2-glycoprotein I antibodies, which are also clinically appropriate [6, 18]. Inter-assay variability in aPL testing has been before noted as a challenge [15, 16], though efforts were completed to standardize examines in this study.
Conclusion:
This case-control study demonstrates a significant association between anticardiolipin IgM antibody levels and hypertensive difficulties during pregnancy. Remarkably, high antibody levels were detected among pregnant women without known autoimmune conditions, emphasizing the need to consider wider screening for antiphospholipid antibodies outsideconventionally defined high-risk groups. The results also proposed that early diagnosis and anticoagulant therapy may help mitigate antibody-mediated opposing pregnancy outcomes. Mixing immunological markers like anticardiolipin IgM into antenatal screening protocols could increase risk stratification and clinical administration in obstetric care. Added large-scale, longitudinal studies are acceptable to confirm these associations and guide clinical rules.
Declaration of Interest
The authors declare no competing financial interests.
Conflict of Interest:
The authors declare no conflicts of interest related to this study.
References
- Lockwood CJ, et al. The prevalence and biological significance of lupus anticoagulant and anticardiolipin antibodies in a general obstetric population. Am J Obstet Gynecol 160 (1989): 439-443.
- Pattison NS, et al. Antiphospholipid antibodies in pregnancy: prevalence and clinical associations. Br J ObstetGynaecol 100 (1993): 909-913.
- Yasuda M, et al. Prospective study of the association between anticardiolipin antibody and outcome of pregnancy. Obstet Gynecol 86 (1995): 555-559.
- Barbui T, et al. Antiphospholipid antibodies in early repeated abortions: A case-controlled study. Fertil Steril 50 (1988): 589-592.
- Parazzini F, et al. Antiphospholipid antibodies and recurrent abortion. Obstet Gynecol 77 (1991): 854-858.
- Rai RS, et al. High prospective fetal loss rate in untreated pregnancies of women with recurrent miscarriage and antiphospholipid antibodies. Hum Reprod 10 (1995):3 301-3304.
- Ginsberg JS, et al. Relationship of antiphospholipid antibodies to pregnancy loss in patients with systemic lupus erythematosus: a cross-sectional study. Blood 80 (1992): 975-980.
- Out HJ, et al. A prospective controlled multicenter study on the obstetric risks of pregnant women with antiphospholipid antibodies. Am J Obstet Gynecol 167 (1992): 26-32.
- Branch DW, et al. Induction of endothelial cell tissue factor activity by sera from patients with antiphospholipid syndrome: a possible mechanism of thrombosis. Am J Obstet Gynecol 168 (1993): 206-210.
- Kutteh WH, et al. A clinical trial for the treatment of antiphospholipid antibody associated recurrent pregnancy loss with lower dose heparin and aspirin. Am J Reprod Immunol 35 (1996): 402-407.
- Branch DW, et al. The association of antiphospholipid antibodies with severe preeclampsia. Obstet Gynecol 73 (1989): 541-545.
- Allen JY, et al. Antiphospholipid antibodies in patients with preeclampsia. Am J Reprod Immunol 36 (1996): 81-85.
- Moodley J, et al. The association of antiphospholipid antibodies with severe early-onset pre-eclampsia. S Afr Med J 85 (1995): 105-107.
- Wilson WA, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum 42 (1999): 1309-1311.
- Harris EN, et al. Anti-cardiolipin antibody testing: The need for standardization. Arthritis Rheum 30 (1987): 835-837.
- Peaceman AM, et al. Interlaboratory variation in antiphospholipid antibody testing. Am J Obstet Gynecol 166 (1992): 1780-1787.
- Roberts JM, et al. Inter-assay variation in antiphospholipid antibody testing. Br J ObstetGynaecol 109 (2002): 348-349.
- Rai RS, et al. Antiphospholipid antibodies and β2-glycoprotein I in 500 women with recurrent miscarriage: Results of a comprehensive screening approach. Hum Reprod 10 (1995): 2001-2005.
- Donohoe S, et al. Fluctuations in levels of antiphospholipid antibodies and increased coagulation activation markers in normal and heparin-treated antiphospholipid syndrome pregnancies. Lupus 11 (2002): 11-20.
- Quenby SM, et al. Predicting recurring miscarriage: what is important? Obstet Gynecol 82 (1993): 132-138.
- Tulppala M, et al. A prospective study of 63 couples with a history of recurrent spontaneous abortion: contributing factors and outcome of subsequent pregnancies. Hum Reprod 8 (1993): 764-770.
- Kumar KS, et al. Beta 2-glycoprotein I dependent anticardiolipin antibodies and lupus anticoagulant in patients with recurrent pregnancy loss. J Postgrad Med 48 (2002): 5-10.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 