COVID-19: Pregnant Women’s Knowledge, Perceptions & Fears. First National Data from Lebanon
Diana Carolina Awad1#, Aline Zaiter1#, Peter Ghiya1#, Karine Zaiter2, Jean G Louka1, 3, Chadi Fakih4, 5, Mirna N Chahine1, 6*
1Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
2Department of Obstetrics and Gynecology, Hermel Governmental Hospital, Bekaa, Lebanon
3Simone-Veil Hospital, Eaubonne, France
4Department of Obstetrics and Gynecology, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
5Department of In-vitro Fertilization, Al-Hadi Medical Center, Beirut, Lebanon
6Department of Basic Sciences, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
#- Authors’ equal contribution
*Corresponding Author: Mirna N Chahine, Department of Basic Sciences, Lebanese University, Faculty of Medical Sciences, Hadath, Lebanon
Received: 12 October 2020; Accepted: 20 October 2020; Published: 04 November 2020
Article Information
Citation:
Diana Carolina Awad, Aline Zaiter, Peter Ghiya, Karine Zaiter, Jean G Louka, Chadi Fakih, Mirna N Chahine. COVID-19: Pregnant Women’s Knowledge, Perceptions & Fears. First National Data from Lebanon. Obstetrics and Gynecology Research 3 (2020): 220-234.
View / Download Pdf Share at FacebookAbstract
Background and objective: The world is facing the pandemic of COVID-19 declared on the 11th of March by the World Health Organization caused by the novel corona virus SARS-COV-2.With insufficient worldwide evidence on the effect of COVID-19 on pregnancy, it is critically important to understand pregnant women’s knowledge, perceptions, and fears regarding COVID-19 and to provide them support as far as possible. The aim of the study was to explore pregnant women’s awareness level of COVID-19 risk and its implication during the outbreak.
Methods: This was a cross-sectional and observational study conducted on pregnant women living in Lebanon, using an electronic survey (Google form). Questions about demographics, knowledge of the COVID-19, risk perception, precautionary measures, source of information and degree of trust, anxiety levels were asked. Scores were calculated. Data was analysed using the SPSS version 22. Descriptive, bivariate, and multivariate analyses were carried out and p<0.05 was considered statistically significant.
Results: With 449 pregnant women enrolled, the mean knowledge score was 4.4 (± 1.17) over 5. The mean perception score was 30.2 (± 5.4) over 51, while the mean precaution score was 19.7(± 3.04) over 25. As for the anxiety, the mean score was 7.1(± 5.8) over 21. Significant correlation was found between knowledge score vs both perception and precaution score (R=-0.213, p<0.001/R=0.465, p<0.00, respectively) between perception score vs knowledge, precaution, and anxiety scores (R= -0.213, p<0.001/ R=0.107, p=0.023/R=0.248, p<0.001, respectively), between precaution score vs knowledge and perception scores (R=0.465, p<0.001/ R=0.107, p=0.023, respectively) and finally between GAD 7 anxiety score vs perception score (R=0.248, p<0.001). Using the Kruskal Wallis, Mann-Whitney, the bivariate analysis sho
Keywords
<p>COVID-19, Pregnant Women</p>
Article Details
1. Introduction
The world is facing the pandemic of COVID-19 declared on the 11th of March by the World Health Organisation and caused by the novel corona virus SARS-CoV-2 [1]. Ever since the emergence of the novel coronavirus, information is rapidly evolving through worldwide conducted studies. The novel Coronavirus is primarily transmitted from symptomatic people to others who are in close contact through respiratory droplets, by direct contact with infected persons, or by contact with contaminated objects and surfaces [2]. The average incubation period of the virus varies between 2-14 days. Symptoms of infection include fever, chills, dry cough, dysgeusia, anosmia, coryza, sore throat, breathing difficulty, myalgia, nausea, vomiting and diarrhea [3]. In addition, it has been shown that advanced age and comorbidities have a great effect on the progression of the disease toward acute respiratory distress syndrome (ARDS) and death. There is no current treatment or vaccine for COVID-19. The entire globe is now gradually releasing from the lockdown phase [1, 3]. Due to the immunosuppressive state and physiological changes (Increased oxygen demand, airways mucosal edema, diaphragm elevation...), pregnant women are prone to developing respiratory infections and serious pneumonia [4]. Actually, severe diseases requiring admission to the maternal intensive care unit and the need for extracorporeal membrane oxygenation may occur in pregnant women, versus non pregnant ones [5-8]. Infected pregnant women with COVID-19 particularly those who develop pneumonia, appear to have an increased risk of preterm labor, pre-labor rupture of membranes, premature birth, preeclampsia, and cesarean delivery for fetal distress [9-10]. Such complications are possibly linked to severe maternal illness [9]. On the other hand, no study have demonstrated the presence of a vertical transmission of SARS-CoV-2 in neonates delivered from pregnant mothers with COVID-19 [10, 11]. In addition, in pregnant women with COVID-19 pneumoniae, transmission of SARS-CoV-2 to the baby through breast milk was not shown to be a risk factor [4], even if an infected mother can transmit the virus through respiratory droplets during the breastfeeding process [12]. Furthermore, there are currently no data indicating an increased risk of miscarriage or early loss of pregnancy in relation to COVID-19 nor teratogenic effect on the fetus [13]. Unfortunately, a wider information about vertical transmission is still needed, and pregnant women are worried about their fetus’s health. Changes of everyday lifestyle, economic crises worldwide, lock down measures, all these factors will contribute in the elaboration of questions and fears among pregnant women [14-15]. In consequence, growing mothers' awareness of coronavirus transmission, risk factors, and red flags, as well as providing tele-counseling for pregnancy care is now a global concern. Gynecology societies, WHO, Centers For Disease Control and Prevention (CDC), ministries of public health across the globe are trying to provide all needed prenatal, intrapartum, and postnatal care for pregnant women [16-20]. As for Lebanon, the first case of COVID 19 emerged on the 21st of February 2020. Lockdown was announced on the 15th of March 2020 [21]. Ever since, the Ministry of public health (MOPH) along with The Lebanese Society of infectious Diseases and Clinical Microbiology (LSIDCM) have been collaborating with other government institutions and scientific societies to adopt a strategy to avoid the spread of the novel coronavirus [21, 22], notably with the Lebanese Society of obstetrics and gynecologists (LSOG) through a campaign to raise awareness of pregnant women via the social media platform. The Technical Taskforce of Corona in Pregnancy in Lebanon, launched since April 2020, has elaborated guidelines on the practice of OBGYN in Lebanon during the outbreak [21, 23]. With insufficient worldwide evidence on the effect of COVID-19 on pregnancy, it is critically important to provide support for women and families as far as possible. Based on a study published about pregnant women’s fears and perceptions on SARS [24] and two other ones on perceptions of the novel coronavirus outbreak by the US population [25], and the Lebanese general population [26], we suggest this present study as the first of its kind regarding COVID-19 and pregnant women in Lebanon. The aim of the study was to explore pregnant women’s awareness level of COVID-19 risk and its implication during the outbreak, by: 1) assessing the level of knowledge, perceptions, and precautions of pregnant women on COVID-19 ; 2) identifying the sources of information about COVID-19 and their reliability, and the degree of trust in the international organizations; 3) measuring the anxiety level of the pregnant women during the crisis.
2. Methods
2.1 Ethical considerations
This observational study required an IRB waiver that was obtained from Al-Hayat Hospital Ethical Committee (ETC-02-2020/ April 2020). It was conducted in accordance with Good Clinical Practice ICH Section 3, and the principles laid down by the 18th World Medical Assembly (Helsinki, 1964) and all applicable amendments. The survey did not require the names, phone numbers, emails of the participants. Each
participant was designated by a code.
2.2 Participants
This was a cross-sectional study conducted across Lebanon on pregnant women or women who have given birth to their babies over the last 6 weeks. Data were collected in the last 2 weeks of April using an electronic questionnaire via Google form. Our team addressed some patients over face-to-face or phone interviews from dispensaries, “Médecins Sans Frontières”, and Red Cross. The population was targeted in the five governorates across Lebanon.
2.3 Questionnaire
The online questionnaire was based on a survey executed and validated by the Yale University [25]. Permission was granted for the reproduction of the questionnaire via another study performed by our team on the Lebanese general population [26]. The questions were presented within a modified validated version of their questionnaire. Other guidelines [16-20, 24] and tools [27] were also used to build up the questionnaire of this study. The online questionnaire (as Google form) was sent to various social media platforms. The questionnaire was used in the English version and the Arabic version. The study instrument was translated using the inverted method of Fortin [28]. The authors first translated the English version into Arabic. Then the Arabic version was translated into English by a healthcare professional translator to compare the agreement of the instrument. The final version of the questionnaire was submitted to a foreigner for linguistic control. A pre-test was carried out with ten persons who were not part of the sample in order to validate the understanding and clarity of the different items. At the end of the pre-test, changes / no changes were made to the questions [28]. Two parts were included in our survey: 1) The informed consent of the participant, background, objective, procedures, voluntary nature of participation, declarations of anonymity, and confidentiality. 2) It included six sections detailed in the next section’’ Measures’.
2.4 Measures
The questionnaire covered six major sections (Appendix
1): I-Demography; II-Knowledge; III-Perception IV- Precautions; V-Source of information and degree of trust; VI- Anxiety Level. A score evaluating the knowledge [16-20, 23-26] (Cronbach’s α = 0.744) of the pregnant woman about COVID-19 included 5 knowledge items related to COVID-19. For every correct answer, one point was given (total 5 points). Incorrect and “I do not know” answers got 0 point. A score evaluating the perception [16-20, 23-26] (Cronbach’s α = 0.718) on the COVID-19 included 12 questions that followed a Likert scale ranging from 1 to 5 as such: 1 “strongly disagree”, 2 “disagree”, 3 “Neutral”, 4 “agree”, 5 “strongly agree”, and 0 “Don’t Know”. Precautions or Preventive measures scale [16-20, 23-25] (Cronbach’s α = 0.718) included 25 questions about the participants’ measures taken to prevent COVID-19. These questions were answered on a True/False basis and Yes/No. The sources of information [25] (television, newspapers / magazines, websites, friends/family, health care professionals, MOPH, and social media) and their reliability in addition to the degree of trust they have shown in the organizations responsible of awareness campaigns (own doctor, MoPH, NGO, WHO). These questions followed a Likert scale from 1 to 5 as such (1 “very weak”, 2 “weak”, 3 “intermediate”, 4 “good”, 5 “very good”, and 0 “don’t know”). Their mental health based on the general anxiety disorder questionnaire GAD-7 (Cronbach’s α = 0.888) that consists of 7 items measuring worry and anxiety symptoms. Each item was scored on a four-point Likert scale (0–3) with total scores ranging from 0 to 21 with higher scores reflecting greater anxiety severity. Scores above 10 were considered to be in the clinical range [27].
2.5 Sample size and statistical analysis
A total of 449 participants were included (400 participants were needed based on Slovin’s Formula, n = N / (1 + Ne2): with N representing the number of pregnant women in the Lebanese population (Around 70000 pregnant women per year) and e representing the p value of 0.05). Three types of analysis (Descriptive, Bivariate and multivariate analysis) were performed:
- Descriptive analysis: Data was represented as frequencies and proportions for the nominal variables and frequencies, mean and standard deviation for the continuous variables. A total of 4 Scores was computed: Knowledge, Perception, Prevention, Anxiety level (GAD-7). A reliability analysis realized to validate each of these scores was performed using the Cronbach’s alpha test (Cronbach Alpha should be more than 0.7). A Shapiro-Wilk’s test (P < 0.05) and a visual inspection of the Q-Q plots and box plots showed that the scores were not normally distributed with a skewness and kurtoses out of the range (-1.96 and +1.96).
- Bivariate analysis: A bivariate analysis was conducted in order to test the correlation between each of the 4 scores and the secondary variables using the Kruskal Wallis, Mann-Whitney, Spearman tests. A correlation was found to be statistically significant if the p value was less than 0.05 using Alpha error equal to 5%.
- Multivariable analysis: A linear regression model was used in order to predict factors affecting each of the 4 scores in our studied population.
3. Results
3.1 Demographic characteristics
This study included 449 pregnant women living in Lebanon, of majority Lebanese (94.9%) aged between 18 and 35 years (86.9%). Among the 449 participants, 37.2% were living in Mount Lebanon, 20.7% in South Lebanon, 18.3% in Bekaa, 12.2% in North Lebanon, and 11.6% in Beirut. Around half of participants were living in a city (54.57%) and 45.4% were living in a village. With regard to their monthly personal income, 25.6% had an income between 1,501,000 LBP and 3,000,000 LBP, and 65.4% had an income less than 1,500,000 LBP. About their educational level, 38.9% had a bachelor’s degree, 22.9% had master’s degree, 18.3% had middle school level, and 12.5% had PhD or equivalent. Concerning Anthropometric data, the mean weight was 70.3 (± 12.5) Kg, the mean height was 164.3 (± 6.1) cm and the mean BMI was 26.05 (± 4.37) Kg/m2. Out of 449 pregnant women, 14.9% were smokers, 5.8% alcoholic consumers, 54.6% employers, and 73.7% healthcare workers. Concerning the working status during COVID-19 phase, 38.1% were going to work and 8.3% were obliged by their employer to go to work. During the outbreak, 29.4% were responsible of the daily grocery supplies.
3.2 Pregnancy characteristics
Out of 449 pregnant women, 48.5% became pregnant for the first time; 15.4% were in the first pregnancy trimester, 27.6% in the second pregnancy trimester, 36.1% in the third pregnancy trimester, and 20.1% had already delivered within the last 6 weeks. Regarding complications and comorbidities, 8.2% had gestational complications (gestational diabetes or hypertension) and 14.3% had chronic diseases. The most prevalent chronic diseases were blood disorders (4.7%), thyroid disorders (4%), mental disorders (1.8%), and asthma (1.3%).
3.3 Knowledge, perception, precaution, and anxiety scores
The mean knowledge score was 4.4 (± 1.17) with a minimum of 0 over 5 and a maximum of 5 over 5. More than half of the participants had a knowledge score 5 over 5 and less than 25% of the participants had a score less than 4 over 5. The mean perception score was 30.2 (± 5.4) with a minimum of 16 over 51 and a maximum of 49 over 51. More than 25% of the participants had a perception score more than 34 over 51 and 25% of the participants had a perception score less than 27 over 51. The mean precaution score was 19.7 (± 3.04) with a minimum of 4 over 25 and a maximum of 25 over 25. More than 25% of the participants had a precaution score more than 22 over 25 and 25% of the participants had a perception score less than 19 over 25. The mean Anxiety GAD-7 score was 7.1 (± 5.8) with a minimum of 0 over 21 and a maximum of 21 over 21. Half of participants had a mean GAD-7 score less than 6 over 21 and 25% of the participants had a mean GAD-7 score more than 11 over 21.
3.4 Trust in the organizations
The most trusted organizations as a source of information were personal doctor (Mean trust = 4.4 ± 0.9 over 5) and MOPH (Mean trust = 4.2 ± 1.1 over 5). A proportion of 80% of the participants were not aware of the existence of a hotline number for the Lebanese Order of midwives in Lebanon, which volunteered to assess women’s concerns and questions during the outbreak.
3.5 Factors affecting the knowledge score
The bivariate analysis between the knowledge score and the study variables showed that a high knowledge level about COVID-19 was high enough when the pregnant woman had an older age (p=0.0001), lived out of Beirut (P =0.0001), was employed (p <0.0001), was paid a higher monthly salary (p<0.0001), had a higher educational level (p<0.0001), was a healthcare provider (nurse, physician, pharmacist...) (p <0.0001), was a nonsmoker (p= 0.022), had a low perception Score (Pearson coefficient = - 0.191, P <0.001), and a high precaution Score (Pearson coefficient = 0.213, P <0.001). A high knowledge score was not associated with nationality, living area, alcohol status, gestational complication, diagnosis with any chronic disease before pregnancy, being a primipara, nor with pregnancy trimester (p>0.05). The multivariate analysis was performed in order to predict the factors affecting the knowledge score concerning coronavirus in pregnant women (Table A). The linear regression analysis showed that the knowledge score increased when she was employed (β =0.321, p<0.001), had a low perception Score concerning COVID-19 (β=-0.047, p<0.001), had a high precaution Score (β=0.174, p<0.001), and lived outside Beirut (β= -0.190, p=0.009).
3.6 Factors affecting the perception score
The bivariate analysis between the perception score and the study variables showed that a pregnant woman had a high perception score when she received a lower monthly salary (p<0.0001), had a lower Educational level (p<0.0001), was unemployed (p<0.0001), was not a healthcare provider (Nurse, physician, pharmacist...) (p = 0.032), was not an alcohol user (p = 0.018), and had low knowledge score (p <0.001, Pearson coefficient = - 0.191), a high precaution score (Pearson coefficient = 0.171, p <0.001) and a high anxiety score (Pearson coefficient = 0.255, p <0.001). A high perception level was not associated with nationality, region, living area, smoking status, gestational complication, being a primipara, nor with pregnancy trimester (p>0.05). The multivariate analysis was performed in order to predict the factors affecting the perception score toward coronavirus in pregnant women (Table B). The linear regression analysis showed that the perception score increased when she was unemployed (β =-1.335, p=0.008), had a low Knowledge Score concerning COVID-19 (β=-1.064, p<0.001), had a high precaution Score (β=0.475, p<0.001), was paid a lower monthly salary (β= -1.268, p<0.001), and when she had a higher GAD7 score (β= 0.209, p<0.001).
3.7 Factors affecting the precaution score
The bivariate analysis between the precaution score and the study variables showed that a pregnant woman had a high precaution score when she had an older age (p=0.004), lived outside Beirut (p=0.018), achieved higher educational level (p<0.001), was employed (p=0.036), was a healthcare provider (nurse, physician, pharmacist...) (p<0.0001), and was in an advanced pregnancy stage or was in the puerperium period (p<0.0001) and had a high knowledge score (Pearson coefficient = 0.213, p <0.001,), and a high perception score (Pearson coefficient = 0.171, p <0.001). A high precaution score was not associated with nationality, region, living area, monthly income, smoking and alcohol status, gestational complication, nor with being a primipara (p>0.05). The multivariate analysis was performed in order to predict the factors affecting the precaution score toward coronavirus in pregnant women (Table C). The linear regression analysis showed that the precaution score increased when the pregnant woman was Healthcare provider (β=0.957, p=0.001), had a high Perception Score towards COVID-19(β =0.120, p<0.001), had a high Knowledge level on COVID-19 (β=1.231, p<0.001), and was in an advanced pregnancy stage(β =0.589, p<0.001).
3.8 Factors affecting the anxiety GAD-7
The bivariate analysis between the GAD-7 score and the study variables showed that a pregnant woman had a high anxiety score when she was Lebanese (p = 0.013), achieved a lower educational level (p= 0.026), and was multiparous (p = 0.021), and had a high perception score (Pearson coefficient = 0.255, p <0.0001). A high GAD-7 score was not associated with age, region, living area, monthly income, employment status, being a healthcare provider, smoking status, alcohol status, gestational complication, chronic disease nor with pregnancy trimester (p>0.05). The multivariate analysis was performed in order to predict the factors affecting the Anxiety GAD-7 score in pregnant women (Table D). The linear regression analysis showed that the Anxiety GAD-7 score increased when she was Lebanese (β=-2.702, p = 0.024), was multiparous (β =-1.257, p=0.017), and had a higher perception Score (β =0.265, p<0.001).
3.9 Correlation between the four scores
Significant correlation was found between knowledge score and both perception and precaution score (R=-0.213, p<0.001/R=0.465, p<0.001 respectively…), between perception score and knowledge, precaution, anxiety scores (R=-0.213, p<0.001/R=0.107, p=0.023/R=0.248, p<0.001 respectively), between precaution score and knowledge and perception scores (R=0.465, p<0.001/ R=0.107, p=0.023) and finally between GAD 7 anxiety score and perception score (R=0.248, p<0.001). Therefore, the perception score was high when the pregnant woman had low level of knowledge regarding COVID-19, a high precaution score and an elevated GAD-7 score.
|
Unstandardized Coefficients |
T |
P.value |
||
|
B |
Std. Error |
|||
|
(Constant) |
1.755 |
0.475 |
3.692 |
0.000 |
|
Employment Status |
0.321 |
0.097 |
3.316 |
0.001 |
|
Perception Score |
-0.047 |
0.009 |
-5.311 |
0.000 |
|
Precaution Score |
0.174 |
0.016 |
11.192 |
0.000 |
|
Region |
-0.190 |
0.073 |
-2.619 |
0.009 |
|
Dependent Variable: Score Knowledge |
||||
B: Beta regression coefficient; T: t regression value; P-value significant if less than 0.05
Table A: Linear regression for the factors predicting the Knowledge score.
|
Unstandardized Coefficients |
t |
P.value |
||
|
B |
Std. Error |
|||
|
(Constant) |
30.127 |
1.790 |
16.826 |
0.000 |
|
Personal Monthly income (in LBP) |
-1.268 |
0.239 |
-5.296 |
0.000 |
|
Employment Status |
-1.335 |
0.505 |
-2.646 |
0.008 |
|
Knowledge Score |
-1.064 |
0.226 |
-4.699 |
0.000 |
|
Precaution Score |
0.475 |
0.084 |
5.673 |
0.000 |
|
Anxiety Score |
0.209 |
0.039 |
5.368 |
0.000 |
|
Dependent Variable: Score Perception |
||||
B: Beta regression coefficient; T: t regression value; P-value significant if less than 0.05
Table B: Linear regression for the factors predicting the Perception score.
|
Unstandardized Coefficients |
t |
P.value |
||
|
B |
Std. Error |
|||
|
(Constant) |
8.952 |
0.936 |
9.562 |
0.000 |
|
Healthcare provider |
0.957 |
0.279 |
3.435 |
0.001 |
|
Perception Score |
0.120 |
0.022 |
5.340 |
0.000 |
|
Knowledge Score |
1.231 |
0.107 |
11.540 |
0.000 |
|
Pregnancy Trimester |
0.589 |
0.122 |
4.829 |
0.000 |
|
Dependent Variable: Score Precaution |
||||
B: Beta regression coefficient; T: t regression value; P-value significant if less than 0.05
Table C: Linear regression for the factors predicting the Precaution score.
|
Unstandardized Coefficients |
t |
P.value |
||
|
B |
Std. Error |
|||
|
(Constant) |
2.563 |
1.954 |
1.312 |
0.190 |
|
Nationality |
-2.702 |
1.190 |
-2.270 |
0.024 |
|
First Pregnancy |
-1.257 |
0.525 |
-2.393 |
0.017 |
|
Perception Score |
0.265 |
0.048 |
5.487 |
0.000 |
|
Dependent Variable: Anxiety GAD-7 score |
||||
B: Beta regression coefficient; T: t regression value; P-value significant if less than 0.05
Table D: Linear regression for the factors predicting the Anxiety GAD-7 score.
4. Discussion
This is the first national Lebanese data aiming to explore pregnant women’s basic knowledge of COVID-19 risk factors and its impact on pregnancy and to identify knowledge gaps and resources needed to improve outcome. In that regard, we evaluated the quality and reliability of information available to pregnant women and their trust toward their healthcare organizations. We also assessed pregnant women’s perceptions of COVID-19 disease severity, their anxiety, and the precautions they took during pregnancy to ensure their wellbeing and healthy fetal development. The socio-economic characteristics of the participants in our study defined a representative sample of pregnant women across Lebanon. Unfortunately, low socioeconomic conditions (below minimum range income, unemployment) affect a significant portion of the population. Although a fairly high level of education among participants (majority had a bachelor degree), we still find smokers and alcohol consumers during pregnancy. However, lower rate of smokers among pregnant women in 2020 was noted in comparison with Chaaya et al findings in 2003 [29], (14.9% vs 32%, respectively), reflecting possible wiser understanding of smoking effects on pregnancy or on the immune system during the novel coronavirus outbreak. Employment status among pregnant women improved from 2003 to 2020 accounting for 54.5%vs 30% in 2003, as reported by Chaaya et al. [29]. Decreased multiparity rate to 51 % versus 66% as previously shown [29]. This could be explained by the engagement of pregnant woman in Lebanon at work.
On the other hand, conception requires responsibilities and strict economical consideration especially in a country facing a critical economic crisis and a continuous war threatening. Furthermore, gestational complications should not be overlooked since 8.2% of participants had experienced one of them. Accordingly, lower gestational complications could explain the reduced maternal mortality in Lebanon to 14.9 % per year between 2010 and 2018 [30]. Regarding COVID-19, this study has shown a relatively high knowledge score among pregnant women across Lebanon. This result was consistent with Halawi et al. survey of the Lebanese public knowledge, perception, and preventive measures regarding the COVID-19 outbreak [26]. Only 3.3% of participants had misleading beliefs about potential vertical or breastfeeding transmission of the novel coronavirus.
Higher level of education, higher monthly salarys, older maternal age, a profession in the healthcare and employment have been associated with a higher level of knowledge. The participants living outside Beirut had a higher level of knowledge and precaution in contrast with Nwafor JI et al. study where rural residents in Nigeria presented inadequate practice of preventive measures [31]. This could explain why the highest number of COVID-19 cases in Lebanon was registered in Beirut as per the MOPH daily reports [32]. A low precaution score was noticed consistent with Halawi et al. study on general Lebanese population [26]. The mean precaution score was 19.5 over 25 (max score=25) with 25% only of the participants acquired a score of 22 over 25. In fact, pregnant women have been able to take general preventive measures (increased hygiene, wearing a facial mask, decreasing social activities, adopting healthy lifestyle, etc.) but there has been a lack of knowledge on specific pregnancy related measures. Despite the clear guidelines developed by the Technical Taskforce of Corona on Pregnancy in Lebanon, an eventual lack of communication between the patient and her physician about obstetric management during the outbreak was explored [23].
Interestingly the majority of pregnant women acknowledged changes regarding in-person visits and shifting to Telemedicine. In fact, this would be attributed to effective explanations received by these patients from their physicians about clinical practice and the requisite visits during pregnancy at the time of COVID-19 outbreak. Despite ACOG and other OBGYN societies recommendations, most participants were not instructed by their doctors to self-monitor the status of fetal and maternal health status by measuring their blood pressure at home. Surprisingly, a large number of participants admitted refusing restrictions on hospital visitors, possible early discharge from hospital, and delay in the first post-partum visit. Even though, the majority preferred not to conceive during the pandemic, half of participants did not discuss methods of contraception with their physicians [16-20]. Poor adherence to the flu vaccine has been noticed. Eventually, same practice was found among the Lebanese population by Halawi et al. [26].
Moreover, the adherence of the pregnant women to the general population preventive measures recommended by the MOPH was consistent with the study by Ng J et al. during the SARS epidemic where pregnant women adhered to precaution measures recommended by WHO [24]. In contrast, a low precaution score for general practice was found by Nwafor JI et al. [31]. Perception score was high enough, in contrast to the study by McFadden et al. on Perceptions of the Adult US Population regarding the Novel Coronavirus Outbreak and to the study by Halawi et al. on general Lebanese population [25, 26]. Moreover, COVID-19 still has an uncertain impact on pregnant women, concerns arise about pregnant women’s health, delivery, breastfeeding, etc. The majority of participants would consider that pregnant women are more prone to contract the disease, to develop its complications and would need more preventive measures than the general population. In addition, they would be afraid of delivery at the hospital.
In fact, Shannon FQ et al reported a decline in institutional deliveries during the Ebola outbreak in Liberia, which could be attributed to fear of encountering the virus in the hospital setting [33]. Speculation occurs around breastfeeding 25% of the patients would avoid it if they were affected by the disease. Similarly, half of pregnant women participating in a recent study in turkey reported uncertainty about breastfeeding safety during COVID-19 pandemic [34]. Furthermore, this survey has highlighted the high level of anxiety among women with high perception scores. This would explain the misbeliefs of pregnant women during this critical period. Similar findings were reported by NG J et al. during the SARS epidemic [24].
On another hand, Lebanese women have shown a higher anxiety score compared to non-Lebanese women. To note, 25% of the participants revealed an anxiety score in the clinical settings. Interestingly, overwhelming distress was also perceived among pregnant women in Turkey [34]. Therefore, focused intervention is needed. Postpartum blues is a serious complication that should always be considered since depression and anxiety prevalence among Lebanese population is higher compared to other countries [35]. Eventually, COVID-19 did not only affect public health, but the socioeconomic status of every person across the globe has changed. In Lebanon, people are at risk of unemployment, job losses, cuts in salaries, etc. This would explain the higher perception score among unemployed women and women with lower monthly incomes. On the other hand, the advanced pregnancy stage was associated with a higher precaution score while multiparity was associated with a higher anxiety score. It could be related to the fact that the mother would increase her concern and responsibility for the life of her own baby. This finding contrasts with the results of the Ng J et al. study during the SARS epidemic which showed no significant association between parity, gestational age, and anxiety [24].
In addition, a higher score of precaution was perceived among healthcare workers possibly explained by the effective training programs conducted in Lebanese hospitals to confront the COVID-19 pandemic. With regard to the trusted source of information, pregnant women across Lebanon would most likely rely on MOPH along with their professional health care provider. This would reveal the success of MOPH in raising public awareness about the spread of the novel corona virus. This finding was consistent with the previous study by Halawi et al. [27]. Besides, 80% of the participants were not aware of the hotline of the order of midwives (http://osfliban.com) who volunteered to assess pregnant women’s fears and perceptions.
4.1 Impact of the study
This study helped us to understand the point of view of pregnant women regarding the novel coronavirus. Revealing their doubts and concerns would make it easier to focus on the relevant factor needed to be involved in awareness campaigns. In addition, the lack of communication between the doctor and his pregnant patients would alarm us to emphasize on the important information that should be given to pregnant women during this outbreak. For example, more focused explanation of the essential role of breastfeeding should be given, as it has not been cleared if the novel corona virus is transmitted via breast milk. Moreover, clinical visits should be managed as the national guidelines recommended and a thorough explanation about the new practice methods should be given to the patients. Hospitals should restrict the number of visitors to the delivery ward (Figure 1).
Adopting a closed circuit in the delivery ward as recommended by national and international guidelines, would ensure that pregnant women are assured regarding medical consults and delivery. As 25 % of the participant revealed a clinical anxiety score, OBGYN physicians should strictly assess their patient’s mental health during this outbreak. By consequence, patients with clinical aspects of mental health diagnosis should be referred to psychiatrists. Post-partum blues and pregnancy related anxiety should not be neglected in this outbreak, since pregnancy alone is a risk factor for mental health problems. From our findings, we can understand the importance of MOPH in raising awareness among the Lebanese population and, in particular, among pregnant women who are in extreme need of clarification and support during this critical period. Midwives’ role in assessing pregnant women’s worries, misconceptions and mental health should be emphasized by encouraging the use of the hotline provided. One of our study strengths was the originality of our study in the region. Data collection was completed in ten days. In addition, questions related to clinical practice in Lebanon were addressed, thus allowing us to better understand the weak aspects that need to be improved in the outpatient and inpatient settings during the outbreak and thus preventing healthcare system deterioration during a possible second wave.
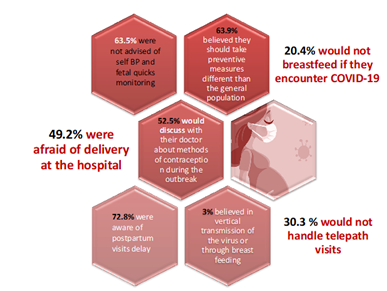
Figure 1: Frequency of answers to knowledge, perception and precaution specific questions provided by pregnant women regarding COVID-19.
4.2 Study limitations
There are many limitations to this study. First, most of the study was conducted using an online questionnaire distributed over social media platform, that was filled in a self-reported manner, which might have caused some Reporting Bias. In addition, this online questionnaire might have favored a Selection bias by since it might not allow illiterate population or population with no access to online resources to participate. However, our team addressed some patients over face-to-face or phone interviews from dispensaries (mostly approached by lower socio-economic class population), ‘’Médecins Sans Frontières’’, and Red Cross clinics in order to minimize reporting and selection biases To note that we could not reach a large number of Syrian and Palestinian refugees even after the concerned associations for this population. Thus, these population groups health care should not be neglected. Furthermore, in our study, the larger number of participants was noticed among health care workers so it might have caused a sampling bias. Last but not least, the pregnancy related anxiety questionnaire PRAQ that assesses anxiety symptoms specifically related to pregnancy, was not used in this questionnaire [67]. We only used GAD-7 score. Therefore, anxiety noticed among pregnant women could be related to pregnancy itself and not to the outbreak situation.
5. Conclusion
In conclusion, a high knowledge score among pregnant women across Lebanon suggests a strong commitment on the part of these women to gain a better understanding of their health, their responsibilities towards their fetuses, and to counter this unpredictable pandemic. High clinical range of anxiety was expected since this outbreak modified every person life across this globe. COVID- 19 has not only threatened public health but has resulted in a multiplication of the socio-economic crisis already present in Lebanon. Thus, understanding pregnant women’s fears, misconceptions, and perceptions would be necessary to help these women cope with daily stressors during the outbreak. The experience of COVID-19 in Lebanon has shown solidarity among the Lebanese population by adhering to lockdown measures, trying to adapt with medical consultations changes, trying to spread positivity and positive actions among the community. Pregnant women are an essential group of the Lebanese population. Although pregnancy itself has not been shown to be a risk factor for contracting the novel coronavirus, pregnant women’s physical and mental health is a major concern during this outbreak, as it has been proved that COVID-19 can induce preterm delivery, premature rupture of membranes, and preeclampsia associated with severe maternal illness [12, 13]. Insisting on the delivery of appropriate antenatal, intrapartum and postnatal care should be highly recommended. Understanding every limitation in the delivery of proper care during this period will prevent further complications and health care system deterioration during a possible feared second outbreak or any other future outbreak.
Conflict of Interest
None
Acknowledgment
We are grateful for Mr. Bachir Atallah for performing the statistical analysis. We also thank all the pregnant women who participated in our study and we wish full recovery to all patients worldwide fighting COVID-19. We are extremely grateful for Dr Imad Abou Jaoude, medical director and chief department OBGYN, Abou Jaoude Hospital and Dr Mabelle-Irene Toloza Awad, OBGYN department, Hermel Governorate Hospital and Dar Al Amal University Hospital who provided us with the contact of many of their pregnant patients. We thank the contribution of volunteers on behalf of ‘’Médecins Sans Frontières’’ and Red Cross to fill out our questionnaire for some of their pregnant patients. The main author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- World Health Organization. WHO Timeline COVID-19 (2020).
- Liu J, Liao X, Qian S, et al. Community Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, Shenzhen, China, 2020. Emerging infectious diseases 26 (2020): 1320-1323.
- De Giorgio A. COVID-19 is not just a flu. Learn from Italy and act now. Travel medicine and infectious disease 35 (2020): 101655.
- Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet (London, England) 395 (2020): 809-815.
- Wu Z, McGoogan J M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72-314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 323 (2020): 1239-1242.
- Liu D, Li L, Wu X, et al. Pregnancy and Perinatal Outcomes of Women With Coronavirus Disease (COVID-19) Pneumonia: A Preliminary Analysis. AJR. American journal of roentgenology 215 (2020): 127-132.
- Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. American journal of obstetrics & gynecology MFM 2 (2020): 100118.
- Garg S, Kim L, Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1-30, 2020. MMWR. Morbidity and mortality weekly report 69 (2020): 458-464.
- Zeng L, Xia S, Yuan W, et al. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. JAMA pediatrics 174 (2020): 722-725.
- Schwartz D A. An Analysis of 38 Pregnant Women with COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Archives of pathology & laboratory medicine (2020).
- Zhang L, Jiang Y, Wei M, et al. Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province. Zhonghua Fu Chan Ke Za Zhi 55 (2020): 166-171.
- Rasmussen S A, Smulian J C, Lednicky J A, et al. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. American journal of obstetrics and gynecology 222 (2020): 415-426.
- Zhang J P, Wang Y H, Chen L N, et al. Zhonghua fu chan ke za zhi 38 (2003): 516-520.
- Rashidi Fakari F, Simbar M. Coronavirus Pandemic and Worries during Pregnancy; a Letter to Editor. Archives of academic emergency medicine 8 (2020): e21.
- Jiao J. Under the epidemic situation of COVID-19, should special attention to pregnant women be given?. Journal of medical virology (2020).
- American College of Obstetricians and Gynecologists. COVID-19 FAQs for Obstetrician-Gynecologists, Obstetrics (2020).
- Centers of Disease Control and Prevention. Interim Considerations for Infection Prevention and Control of Coronavirus Disease 2019 (COVID-19) in Inpatient Obstetric Healthcare Settings (2020).
- Royal College of Obstetricians and Gynecologists. Coronavirus (covid19) infection in pregnancy, information for healthcare professionals, version 7 (2020).
- Peyronnet V, Sibiude J, Deruelle P, et al. Infection par le SARS-CoV-2 chez les femmes enceintes : état des connaissances et proposition de prise en charge par CNGOF [SARS-CoV-2 infection during pregnancy. Information and proposal of management care. CNGOF]. Gynecologie, obstetrique, fertilite & senologie, 48 (2020): 436-443.
- The American College Of Obstetricians And Gynecologists. Outpatient Assessment and Management for Pregnant Women With Suspected or Confirmed Novel Coronavirus (COVID-19) (2020).
- Republic of Lebanon the Ministry of Public Health. Statement Issued by the MoPH on the nCov-2019 in Lebanon (2020).
- The Lebanese Society Of Diseases And Clinical Microbiology. The Lebanese Society of Infectious Diseases and Clinical Microbiology (LSIDCM) Guidelines for the Management of COVID19 (2020).
- Technical Taskforce of Corona in Pregnancy-Lebanon, Outpatient COVID-19 (2020).
- Ng J, Sham A, Tang PL, et al. SARS: pregnant women’s fears and perceptions. Br J Midwifery 12 (2004): 698-702.
- McFadden S M, Malik A A, Aguolu O G, et al. Perceptions of the adult US population regarding the novel coronavirus outbreak. PloS one 15 (2020): e0231808.
- Halawi H, Ghazal M, Cherry H, et al. Knowledge, Perception and Precautions of the Lebanese Population Regarding the Novel Coronavirus Outbreak. Journal of Public Health and Diseases 3 (2020): 72-81.
- Spitzer R L, Kroenke K, Williams J B, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine 166 (2006): 1092-1097.
- Fortin MF, Gagnon J. Fondements et étapes du processus de recherche : méthodes quantitatives et qualitatives. (2nd ed). Canada : Chenelière Education Inc (2016).
- Chaaya M, Awwad J, Campbell O M, et al. Demographic and psychosocial profile of smoking among pregnant women in Lebanon: public health implications. Maternal and child health journal 7 (2003): 179-186.
- El-Kak F, Kabakian-Khasholian T, Ammar W, et al. A review of maternal mortality trends in Lebanon, 2010-2018. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 148 (2020): 14-20.
- Nwafor J I, Aniukwu J K, Anozie B O, et al. Pregnant women's knowledge and practice of preventive measures against COVID-19 in a low-resource African setting. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 150 (2020): 121-123.
- Lebanese Ministry Of Public Health, COVID-19 Daily Situation Report, October 2020.
- Shannon F Q, Horace-Kwemi E, Najjemba R, et al. Effects of the 2014 Ebola outbreak on antenatal care and delivery outcomes in Liberia: a nationwide analysis. Public health action 7 (2017): S88-S93.
- Yassa M, Birol P, Yirmibes C, et al. Near-term pregnant women's attitude toward, concern about and knowledge of the COVID-19 pandemic. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians 33 (2020): 3827-3834.
- Eva Hobeika, Miguella Outayek, Diana Malaeb et al. Postpartum Depression and Anxiety among Lebanese women: correlates and scales validation. Research Square (2020).
- Sinesi A, Maxwell M, O'Carroll R, et al. Anxiety scales used in pregnancy: systematic review. BJPsych open 5 (2019): e5.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 