Effect of cervical pessary on pregnancy outcome in patients with twin pregnancies: a systematic review and meta-analysis
Wang yuea1, Wu jiaxing2, Ma di3, Sun xin4, Lin lin5, Wang bo6, Huang mingli*
a1, 3, 4, 5, 6 Department of Obstetrics and Gynecology, First Affiliated Hospital of Harbin Medical University Harbin, Heilongjiang, China
2Department of Obstetrics and Gynecology, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, 1665 Kongjiang Road, Shanghai.
* Huang mingli, PHD, First Affiliated Hospital of Harbin Medical University Harbin, Heilongjiang, China
*Corresponding Author: Huang mingli, PHD, First Affiliated Hospital of Harbin Medical University Harbin, Heilongjiang, China.
Received: 21 December 2022; Accepted: 18 January 2023; Published: 27 January 2023
Article Information
Citation:
Wang yue, Wu jiaxing, Ma di, Sun xin, Lin lin, Wang bo,Huang mingli. Effect of cervical pessary on pregnancy outcome in patients with twin pregnancies: a systematic review and meta-analysis. Obstetrics and Gynecology Research 6 (2023): 31-47.
View / Download Pdf Share at FacebookAbstract
Background
Preterm birth is the main cause of child death under 5years of age. The incidence of twin pregnancies is less than 2%, but the incidence of preterm delivery is 50% and the risk of neonatal death is 5 times higher in twin pregnancies than in singleton pregnancies. However, there is still no consensus on the effect of cervical pessary on preventing preterm delivery, prolonging the pregnancy cycle, and improving maternal and infant outcomes in patients with twin pregnancies.
Objectives
To explore the effect of cervical pessary on the pregnancy outcome of unselected twin pregnancy patients.
Search Strategy Up to Jan 2022, researchers
Searched PubMed, EMBASE, COCHRANE, Web of Science, Wan fang, Weipu, and CNKI databases for research.
Study eligibility criteria
Randomized controlled trials that compared cervical pessary with standard care (no pessary) or alternative interventions (conventional and standard treatment (e.g.,Atoxiban therapy or vaginal progesterone) in patients with twin pregnancies.
Study appraisal and synthesis methods
Two authors independently extracted information related to the study characteristics and test results from each of the included literature, and used Revman 5.3 to analyze the data. Pooled relative risks with 95% confidence intervals were calculated. Cochrane collaborative tools were used to assess the risk of bias in individual studies. The main results were premature delivery at <34 weeks, preterm delivery <37 weeks, and abortion <28 weeks. Secondary results included spontaneous preterm delivery <34 weeks, spontaneous preterm delivery <34 weeks, spontaneous abortion <28 weeks, and preterm prelabour rupture of membranes <34 and preterm prelabour rupture of membranes, vaginal bleeding, chorioamnionitis, delivery week, vaginal infection
Keywords
<p>cervical pessary; pregnancy outcome; fetal outcome; preterm birth; preterm delivery; twin pregnancy</p>
Article Details
Introduction
Studies have shown that the mortality rate for children under 5 years of age in China is 37%, with the main cause of death being complications from premature birth, accounting for about 17% of all deaths[1].Surviving preterm infants are at greater risk for short-term complications, with higher rates of respiratory distress syndrome, bronchopulmonary dysplasia, necrotizing enterocolitis, sepsis, intraventricular hemorrhage, paraventricular leukodystrophy, and retinopathy than in term-born neonates[2,3]. The rate of these adverse outcomes is related to the gestational week at delivery and luckily preterm deliveries are more frequent (70%) in the late preterm period even in twin pregnancies[4], where in about 40% of cases labor starts spontaneously with or without PPROM. The incidence of twin pregnancies is less than 2%, but the incidence of preterm delivery is 50% and the risk of neonatal death is 5 times higher in twin pregnancies than in singleton pregnancies[5,6].Cervical insufficiency as a cause of spontaneous preterm delivery in patients with twin pregnancies[7]. Currently, the main therapeutic measures regarding the prevention of preterm delivery in patients with twin pregnancies are the vaginal progesterone, cervical cerclage and cervical pessary. In the Clinical Guidelines for the Management of Twin Pregnancies published in China in 2020, it is clearly stated that in asymptomatic patients with twin pregnancies with a short cervix, the use of progestins can effectively reduce the risk of preterm delivery before 35 weeks of gestation[8].As for cervical cerclage, for singleton patients, this treatment is currently considered effective in preventing preterm birth[9],but for patients with twin pregnancies, the efficacy of the treatment remains controversial[8,10]. Originally used to treat pelvic organ prolapse, cervical pessary placement has been used to prevent preterm birth since 1990. Currently, the Arabin cervical pessary is widely used in the prevention of spontaneous preterm labor. Cervical pessary reduces both uterocervical angles and corrects cervical angulation by pushing the cervix up toward the uterus. Maintaining the cervix aligned to the uterine axis leads to reduced cervical tissue stretch, so avoiding further cervical shortening[11,12].Currently studies show that cervical pessary is effective in reducing the rate of preterm birth in patients with singleton pregnancies[13,14],while cervical pessary remains controversial in patients with twin pregnancies. A retrospective analysis in 2016 showed that cervical pessary placement reduced the rate of preterm delivery before 37 and 34 weeks of gestation in patients with twin pregnancies[15].Data in literature are controversial, indeed in 2019, an RCT trial suggested that cervical pessary placement reduces preterm birth rates and improves pregnancy outcomes in patients with twin pregnancies[16], whereas others RCT and meta-analyses showed opposite conclusion[17,18]. In the 2014 ACOG guidelines, nonspecific and effective treatment were recommended to prevent preterm birth for twin women[19]. In 2019, the Canadian Association of Obstetricians and Gynecologists (SOGC) still believed that, even in twin patients with a short cervix, there was still no evidence that cervical pessary could effectively prevent premature birth[10]. China updated its guidelines in 2020 and did not give clear recommendations on the use of cervical pessary to prevent premature birth in twin patients. However, Chinese guidelines clearly support that vaginal progesterone can reduce the preterm birth and neonatal prevalence before 35 weeks in pregnant women with asymptomatic ultrasound showing a short cervix[8]. As for cervical cerclage, as an invasive treatment, its efficacy varies due to its different timing and indications. In 2014, ACOG noted that existing data demonstrated that ring ligation actually significantly increased preterm birth rates in asymptomatic twin pregnancies with CL ≤25mm[19]. The SOGC guidelines also indicate that cerclage increases asymptomatic preterm rates in twin pregnancies with CL ≤25mm, arguing that without physical evidence of physical examination, taking cerclage merely indicated by ultrasound hints of cervical shortening or previous second trimester abortion history increases the risk of preterm pregnancy. In conclusion, there is still no consensus on the effect of cervical pessary on preventing preterm delivery, prolonging the pregnancy cycle, and improving maternal and infant outcomes in patients with twin pregnancies. In this paper, we aim to present a meta-analysis of the effects of cervical pessary placement on perinatal outcomes in patients with twin pregnancies discussing the effectiveness of this procedure in improving adverse pregnancy and neonatal outcomes.
Materials and Methods
Literature Search
This study was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) statement[20],and was registered with PROSPERO, number CRD42021275530.Two authors independently extracted all study data into a canonical form. When there is a difference of opinion, the two authors reach a consensus through negotiation.
Up to Jan 2022, researchers searched PubMed, EMBASE, COCHRANE, Web of Science, Wan fang, Wi Pu and CNKI databases, for example, in the PubMed database, they searched for ((((((((cervical) OR pessary) OR cervical pessary)) OR pessary[MeSH Terms])) AND ((((((prematurity) OR prematurity[MeSH Terms]) OR premature birth) OR premature birth[MeSH Terms]) OR Preterm delivery) OR Preterm delivery[MeSH Terms])) AND (((((Twin) OR pregnancy) OR Twin pregnancy[MeSH Terms]) OR Multiple pregnancy) OR Multiple pregnancy[MeSH Terms])) AND ((cervical length) OR short cervix). Investigators selected studies for inclusion that met the inclusion standards. Relevant publications were searched.
Researchers also systematically reviewed the references of the literature included in the study.
Clinical pregnancy outcomes and neonatal outcomes were collected in the cervical pessary group (experimental group) and the non-cervical pessary group (control group). Cervical cerclage was excluded at an early stage of the study for the following reasons: 1. Meta-analysis has been conducted in relevant studies[21] ; Cervical cerclage is more irritating to patients than cervical pessary, cervical pessary as a non-invasive means, combined with non-invasive conventional fetal preservation methods such as bed rest, atosiban, vaginal progesterone, etc., compared with conventional fetal care methods, lower heterogeneity, more reliable results.
Two reviewers reviewed each potential eligibility article separately, analyzed the quality of the studies according to the Cochrane scale, and extracted data. Two authors W-Y and M-Dindependently performed the original screening of all study titles and abstracts, excluding literature that was deemed irrelevant by both observers. The PRISMA flowchart provides more detailed information about the article selection process (picture 1: flowchart). The researchers recorded in detail the year of publication of the records, country, study type, number of participants, week of gestation and range of cervical length (CL) at the time of placement of the cervical pessary, and mode of treatment for both groups of patients (table 1: characteristics of the included studies).
|
Name |
Country |
Type |
Number |
Characteristics |
Treatment |
|
Goya 2015[33] |
Spain |
RCT |
154 |
18-22week CL≤25mm |
Arabin Pessary Conventional treatment |
|
Nicolaided 2016[18] |
Multiple center |
RCT |
1180 |
18-25weel CL unlimitated |
Arabin Pessary Conventional treatment |
|
Liem 2013[32] |
Netherlands |
RCT |
808 |
16-22week CL unlimitated |
Arabin Pessary Conventional treatment |
|
Merced 2019[16] |
Spain |
RCT |
132 |
24-34week CL<20mm treatment |
Arabin Pessary Conventional treatment |
|
Norman 2021[48] |
UK |
RCT |
503 |
18-21week CL<35mm |
Arabin Pessary Conventional treatment |
|
Dang 2019[23] |
Vietnam |
RCT |
297 |
16-22week CL≤38mm |
Arabin Pessary Vaginal progesterone400mg |
|
Berghella 2017[30] |
Multiple center |
RCT |
46 |
18-24week CL<30mm |
Cervical Pessary Conventional treatment |
Table 1: Characteristics of the included studies
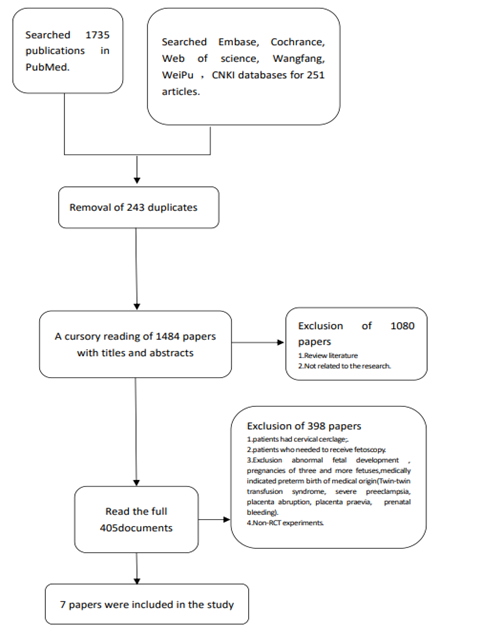
Picture 1:Flowchart
1.2 Eligibility criteria
The purpose of the included study was to investigate the effect of cervical pessary placement on pregnancy outcomes in patients with twin pregnancies. The inclusion criteria were1. Patients with twin pregnancies who underwent gynecological trans-vaginal ultrasound (TVU) after 16 +0 -33+7weeks of gestation and underwent cervical pessary because of the short cervix, and cervix dilation < 10 mm[8]. There were no special requirements for the mode of pregnancy (ART and non-ART), and medical history of patients with twin pregnancy), 2. Must be done for RCT studies, 3.The experimental group must be patients undergoing cervical pessary, which can be performed in combination with conventional and standard treatment (e.g. Atoxiban therapy) or vaginal progesterone, 4.The control group must be routine noninvasive treatment such as conventional therapy (such as Atoxiban) or vaginal progesterone. The exclusion criteria were: 1. The patient underwent cervical cerclage at this pregnancy, 2. patients who needed to receive fetoscopy, 3. Exclusion abnormal fetal development, pregnancies of three and more fetuses, medically indicated preterm birth of medical origin (Twin-twin transfusion syndrome, severe preeclampsia, placenta abruption, placenta previa, prenatal bleeding); 4. non-RCT experiments.
1.3 Outcome measures and data item extraction
Two researchers extracted information related to the study characteristics and test results from each of the included literature. The main outcome was preterm delivery (ptd) before 34 weeks gestation, preterm delivery before 37 weeks, miscarriage a before 28 weeks (China officially defines miscarriage as occurring before 28 weeks' gestation). Secondary outcomes included spontaneous preterm delivery(sptd) before 34 weeks, spontaneous preterm delivery before 37 weeks, spontaneous miscarriage before 28 weeks(SM), preterm prelabor rupture of membranes(PPROM),preterm prelabor rupture of membranes before 34 week, delivery week (DW),vaginal bleeding(VB),chorioamnionitis(C),vaginal infection(VI),vaginal discharge (VD),C-section, intrauterine death or stillbirth, neonatal death , low-birth weight (≤2500g), very low birth weight (<1500g), Respiratory distress syndrome (RDS),Intraventricular hemorrhage(IVH),Necrotizing Enterocolitis (NE),Retinopathy (RE),Sepsis (S).
1.4 Risk assessment of bias
Cochrane collaborative tools were used to assess the risk of bias in individual studies, including: 1.selection bias; 2. implement bias; 3. detection bias; 4. attribution bias; 5. Reporting bias; 6. Other bias (including measuring bias; sampling bias and follow- up bias) (See details in the table2: bias of included literature assessment table). The quality of evidence for primary and secondary outcomes were assessed by using the GRADE approach, which takes into account 5 domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The GRADE approach categorizes the certainty of the evidence into 4 levels: (1) high: we are very confident that the true effect lies close to that of the estimate of the effect, and further research is unlikely to change our confidence in the estimate other effect; (2) moderate: we are moderately confident in the effect estimate, and the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; (3) low: our confidence in the effect estimate is limited, and the true effect may be substantially different from the estimate of the effect; and (4) very low: we have very little confidence in the effect estimate, and the true effect is likely to be substantially different from the estimate of effect.
|
Name |
selection bias |
implement bias |
detection bias |
attribution bias |
reporting bias |
Other bias |
|
Berghella2017 |
- |
+ |
- |
- |
- |
+ |
|
Goya2015 |
- |
- |
- |
- |
- |
- |
|
Nicolaided 2016 |
- |
- |
- |
- |
- |
- |
|
Liem2013 |
- |
- |
- |
- |
- |
- |
|
Merced2019 |
- |
- |
- |
- |
- |
+ |
|
Norman2021 |
- |
- |
- |
- |
- |
+ |
|
Dang 2019 |
? |
- |
- |
- |
? |
+ |
Table 2: The Bias of included Literature assessment table
1.5 Data processing and analysis
Researchers used Revman 5.3 to analyze the data. It belonged to two categorical outcome variables and relative rate (RR) was used as the effect indicator. For the outcome index belonging to the continuous variables, the standards mean difference (SMD) was used as the effect indicator.95% confidence interval was calculated to evaluate the strength of the association between cervical pessary and the risk of adverse pregnancy-related outcomes. The RR values were calculated by the Z test. The P-value of <0.05 was defined as meaningful. Random-effects and fixed-effects models were applied in this meta-analysis. To assess inter-study heterogeneity, the Q test was applied to calculate I2. The I2 values were defined as 25%, 50%, and 75%, representing low, moderate, and high heterogeneity, respectively. When high heterogeneity was observed, random-effects models were used to pool results, and a fixed-effect model. When the heterogeneity is too high, there should be further excluded clinical and methodological heterogeneity, and a random effect model is used for analysis. If there was evidence of statistical heterogeneity (I2>50%), it is necessary to explore the possible sources by using sensitivity and subgroup analyses to search for evidence of bias or methodological differences among trials. Researchers used the exclusion method article by piece exclusion literature method for sensitivity analysis. Differences in the elimination results and the original merger results were also assessed. Publication bias was visually judged by drawing funnel plots.
Results
Results of literature search
A total of 7 literature studies and 3120 patients in all were included in this paper. 4 studies containing data of patients with CL≤25m. 7 studies include data of patients with CL≤38mm.
2.2 Primary and secondary outcome summary
.A meta-analysis was performed for all of the literature
First, we performed meta-analyses on all included literature to compare the efficacy of cervical support in improving pregnancy outcomes with neonatal outcomes (see table3), It was found that the patients in the experimental group (cervical pessary group) had a longer deliver week (RR 0.25, P<0.00001), higher incidence of vaginal discharge (RR5.14, P<0.00001) and vaginal bleeding (RR 1.56, P<0.00001) than in the control group, which was statistically significant. As neonates, in experimental groups, the incidence of low birth weight (RR 0.9, P<0.0001), NE (RR0.57, P=0.01) and neonatal septicemia (RR 0.64, P=0.03) were significantly lower than control group, which were statistically significant. Compared DW, vaginal discharge, vaginal bleeding, low birth weight, S, remarkable heterogeneity could be seen. The sensitivity analysis was performed article by article, and the exclusion literature name and the p values after analysis are shown in the table 3 below. The funnel map suggests publication bias in part of the study.
*It indicates that the statistical results were statistically significant
Table 3: A meta-analysis was performed for all of the literature
2.2.2 Subgroup analysis was performed based on the CL
During the process of literature inclusion, the researchers found differences in the CL of the included patients, and to avoid the outcome bias caused by different CL, the subgroup analysis was performed.
Results of the subgroup analysis based on CL≤38mm rows are shown in table 4. It can be seen that cervical pessary was better than the control group of preventing spontaneous premature delivery before 34 weeks (RR0.77, P=0.03) and premature delivery before 34 weeks (RR0.72 , P=0.004), prolonged delivery week (RR 0.37, P<0.00001), reducing the incidences of low birth weight (RR0.74, P<0.00001), neonatal mortality (RR 0.50, P=0.01), neonatal necrotic enterocolitis (RR0.33, P=0.0004) and neonatal sepsis (RR0.64, P=0.03). All the results were statistically significant. However, the incidence of increased vaginal discharge and vaginal bleeding in the cervical pessary group was significantly higher than in the control group. Some studies funnel plots suggest publication bias.
*It indicates that the statistical results were statistically significant
Table 4: Subgroup analysis was performed based on the CL≤38mm
Results of the subgroup analysis based on the ≤25mm line of CL are shown in table 5.Due to insufficient data, comparisons were made only between premature delivery before 34 weeks (RR 0.53, P=0.0001), spontaneous premature delivery before 34 weeks (RR 0.73, P=0.04), low weight birth (RR 0.62, P<0.00001). Results showed that cervical pessary was better in reducing spontaneous preterm birth <34 weeks and preterm birth <34, decreased the born of lower weight infants, and the results were statistically significant. Some study funnel plots suggested publication bias.
2.2.3 Subgroup analysis was performed based on the type of cervical pessary.
Because of Bioteque cervical pessary in Berghella2017, which could cause performance bias, the result of subgroup analysis after excluding Berghella2017 show in table 6 that the patients in the experimental group (merely Arabin cervical pessary group) had a longer deliver week (RR 0 . 2 5 , P<0.00001), higher incidence of vaginal discharge (RR6.35, P<0.00001), C- section (RR1.1, P=0.04), vaginal bleeding (RR 1.56, P<0.00001), which was statistically significant. For neonates, in experimental groups, the incidences of low birth weight (RR 0.9, P<0.0001), NE (RR0.54, P=0.01) and S (RR0.57, P=0.009) were lower, which was statistically significant. Remarkable heterogeneity could be seen. The sensitivity analysis was performed article by article, and the exclusion literature name and the p values after analysis are shown in the table 6 below. After sensitivity analysis, the ptd <34 weeks, DW, VD, PPROM, DE, low birth weight was statistically significant, and the P value of sptd <34 weeks and S changed, but were not statistically significant. The funnel map suggests publication bias in part of the study.Results of the subgroup analysis based on CL ≤38mm rows are shown in table 7. It can be seen that Arabin cervical pessary was better than the control group of preventing ptd<34 (RR0.69, P=0.002) and sptd<34 (RR0.76, P=0.03), prolonged delivery week(RR0.37, P<0.00001), increased VD (RR3.57, P<0.00001)and VB(RR1.56, P<0.00001), decreased incidence of PPROM (RR2.17, P=0.02),reducing neonatal mortality(RR0.42, P=0.006),the incidences of low birth weight(RR 0.74, P<0.00001), NE (RR0.29, P=0.0002), S(RR 0.57, P=0.009),which was statistically significant. Remarkable heterogeneity could be seen. The sensitivity analysis was performed article by article. Funnel plots show the publication bias in part of the studies.
Results of the subgroup analysis based on the CL≤25mm are as same as table 5. Due to insufficient data, comparisons were made only between premature delivery before 34 weeks (RR0.53, P=0.0001), spontaneous premature delivery before 34 weeks (RR0 . 73 , P=0.04), low weight birth (RR0.62, P<0.00001). Results showed that merely Arabin cervical pessary was better
Obstetrics and Gynecology Research Vol. 6 No. 1– March 2023. 11
reducing spontaneous preterm birth <34 weeks and preterm birth <34, decreased the born of lower weight infants, and the results were statistically significant. Some study funnel plots suggested publication bias. Remarkable heterogeneity could be seen. The sensitivity analysis was performed article by article, and the exclusion literature name and the p values after analysis are shown in the table 5 below. After sensitivity analysis, sptd<34 keep his statistically significant, but low birth weight was not.
(*It indicates that the statistical results were statistically significant
Table 5: Subgroup analysis was performed based on the CL≤25mm
*It indicates that the statistical results were statistically significant
Table 6: Subgroup analysis was performed based on the Arabin cervical pessary
(*It indicates that the statistical results were statistically significant)
Table 7: Subgroup analysis was performed based on the Arabin cervical pessary and CL ≤38mm
2.3 Quality evaluation and bias evaluation
These literatures were assessed for the risk of bias (as table 2 and picture2). Considering the particularity of the study, that the patients in the experiment knew all about their intervention after participating in the experiment, the researchers default that patient’s blindness are low-risk, and only evaluate the blind method of the researchers and the results assessors. The high uncertain risk of Merced 2019, Norman 2021 and Berghella 2017. Dang’s high uncertain risk is from missing visits, and it has uncertain selection bias and reporting bias. Berghella 2017 has high preform bias. The results of GRADE approach categorizing the certainty of the evidence are in table 3-7. During analysis, we found that the quality of evidences could be influenced by Berghella 2017 because of his bias from patients’ selection. Besides, the bias from Merced 2019, Norman 2021 and Dang 2019 could influence the certificate evidence quality. All in all, the quality of evidences in table 3-5 is low. But after subgroup analysis, it is obvious that the quality of evidences has improved.
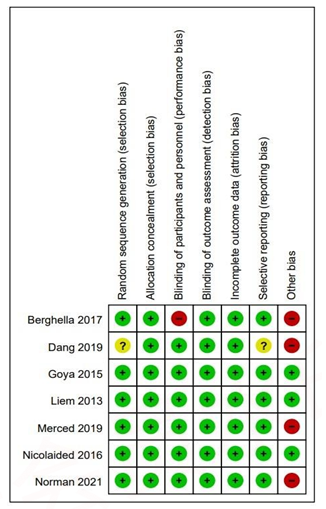
Picture 2: Risk bias assessment
Discussion
Main findings and interpretation
The results found that the efficacy of cervical pessary in twin patients suggested that cervical support prolonged the gestational week of twin patients and reduced the incidence of low weight birth, NE and the incidence of neonatal sepsis. In 2012, the CL
≤25 mm can be considered as short cervix by singleton guidelines published by American Obstetricians and Gynecologists (ACOG)[22].However, there were also studies using a CL of less than the 25th percentile (≤38mm)[23,24].Therefore, the researchers used these two sets of digital row subgroup analysis, respectively. The results suggested that in twin patients with
≤38mm of CL, cervical pessary reduced preterm birth <34 weeks, decreased rate of spontaneous premature delivery <34 weeks, prolonged delivery week, reduced neonatal mortality, neonatal necrotizing enterocolitis, and neonatal sepsis; For patients with CL ≤25mm, although the data are insufficient, limited data still suggest that cervical pessary is better than conventional treatment in reducing preterm birth rate <34 weeks, spontaneous preterm birth <34 weeks, and reducing the incidence of low- weight infants. Although, increased vaginal secretions and higher vaginal bleeding rate were higher in the experimental group when ≤38mm of the CL was observed, there was no significant difference in the incidence of vaginitis and chorioamnionitis compared with the control groups. This shows that cervical pessary can effectively reduce the rate of preterm birth before 34 weeks in twin patients with CL less than 38mm, effectively prolong pregnancy week, reduce neonatal mortality, neonatal necrotizing enterocolitis and neonatal sepsis, and effectively improve adverse maternal pregnancy outcome. Considering type of cervical pessary, merely Arabin cervical pessary prolonged the gestational week of twin patients and reduced the incidence of low weight birth, necrotizing enterocolitis and neonatal sepsis, but it also increased the incidences of vaginal discharge, C- section and vaginal bleeding without any changed of vaginal infection and chorioamnionitis. The results suggested that in twin patients with ≤38mm of CL, cervical pessary reduced preterm birth <34 weeks, spontaneous preterm delivery before 34 weeks and incidence of PPROM, prolonged delivery week, decreased neonatal mortality, neonatal necrotizing enterocolitis, and neonatal sepsis, but increased the incidences of VD and VB; For patients with CL ≤25mm, although the data are insufficient, limited data still suggest that cervical pessary is better than conventional treatment in reducing preterm birth rate <34 weeks, spontaneous preterm birth <34 weeks, and reducing the incidence of low-weight infants. Although, increased vaginal secretions and higher vaginal bleeding rate were higher in the experimental group. Importantly, while Arabin cervical pessary do increase vaginal discharge and vaginal bleeding rate, but there is no difference of vaginal infection and chorioamnionitis, which means cervical pessary is safe to twin-pregnancy women. Comparing our data, different CL seems to do not influence the effect of cervical pessary, especially on sptb<34 weeks, ptb<34weeks and low birth weight, but patients with CL ≤38mm have great effect and less side effect. The effect of cervical pessary in CL≤25 mm is still need more research. The results of the subgroup analysis were significantly improved after excluding Berghella 2017, and the level of evidence was also significantly increased, which proved that the subgroup analysis was effective.
3.2 Sensitivity analysis
During the course of the sensitivity analysis, the researchers found the phenomena of altered P values after the sensitivity analysis. After analyzing the sources of heterogeneity one by one, the researchers thought that the reasons for the heterogeneity were: 1. The data gap is too large; 2. There is a publication bias. 3.Existing bias in 7 research, particularly Berghella 2017.4. There are other potential unmeasured confounders. Researchers found several factors could cause confounders such as cervical surgery history, miscarriage history, difference race, the time of pregnancy or delivery, ART history, time of placing or removing cervical pessary, vaginal progesterone. Particularly, vaginal progesterone has been proven to prevent preterm birth. It is possible to cover the effect of cervical pessary. Otherwise, combined treatment of cervical pessary plus vaginal progesterone is uncertain. One retrospective cohort study of twin pregnancies draws a conclusion that cervical pessary combined with vaginal progesterone could prolonged pregnancy and reduce risk of adverse neonatal outcomes[25]. In 2020, a retrospective study of 57 patients with (dichorionic diamniotic twin (DCDA) showed that a cervical pessary combined with vaginal progesterone reduced the rate of preterm birth in patients [26]. There is one study showed that cervical pessary combined with vaginal progesterone could prolonged pregnancy, reduce prematurity rate and a low rate of perinatal complications[27]. However, a meta-analysis[28] and a RCT [29]in 2016 showed that combined treatment did not decrease the risk of preterm birth compared with cervical pessary in singletons with short CL. Therefore, it is not sure if vaginal progesterone could enhance or weaken the influence of cervical pessary to twin pregnancy. More clinical trials are needed to prove the efficiency of combined treatment. As for Berghella 2017, it was published as a small RCT research[30]. In stand of Arabin cervical pessary, Berghella chooses Bioteque cup cervical pessary included 46 women. After subgroup based on type of cervical pessary, comparing data, all the difference seems to indicate that the different type of cervical pessary had similar effects .However, Kyvernitakis believes that there are differences in the appearance of Bioteque and Arabin, and these may have different effects[31].
3.3 Current research
Twin gestations are different from singleton patients, because of their excessive uterine enlargement, intrauterine pressure increases too much, beyond the limit that the cervix can bear, easy to lead to cervical insufficiency, and then cause premature birth. For twin patients, cervical pessary is still controversial. Leim2013 was the first to study the treatment effect of cervical support in twin pregnancy patients through RCT experiments, and proposed that cervical uterine care could not effectively prevent adverse perinatal outcome or premature birth in multiple pregnant women, but its subgroup analysis proved that cervical pessary of the cervix in twin patients can reduce adverse perinatal outcome of ≤ 38mmm[32].This provided later researchers with ideas to study the relationship between different cervical length and the efficiency of cervical pessary. In 2016, a retrospective analysis revealed that cervical pessary placement reduced the rate of preterm delivery that occurred before 36 and 34 weeks[15]. A network meta-analysis published in 2021 suggested that cervical pessary, progesterone and cerclage do not show a significant effect in reducing the rate of PTB or perinatal morbidity in twins[21]. Contradictory findings also exist in the RCT study. A RCT experiment published by Goya in 2015 for the first time that cervical pessary reduced the rate of preterm delivery by 34 weeks in twin patients with a CL ≤25mm[33].However, in 2016, Kypros believes that cervical pessary does not reduce the preterm rate in twin patients with cervical insufficiency[34]. In 2017, by comparing treated patients with cervical pessary, cervical cerclage and vaginal progesterone, a meta-analysis proposed that only vaginal progesterone extended the gestational week, but not statistical significance[35]. In 2019, an RCT experiment proposed that cervical pessary reduced the rate of preterm birth and improved pregnancy outcomes in patients with twin gestation [16]. The latest meta-analysis in 2020 does not support the use of cervical pessary to prevent premature birth or improve perinatal outcomes in twin short cervix and unselected twin pregnancies[17]. It cannot deny that it[17] is inspired to singletons. However, this paper studied high-risk pregnant women, not twin pregnant women alone, and it included only two studies about twin pregnancy, the data are so grossly insufficient that leads to a bias in their findings. About Xiong YQ [36], I have read this document when I collected the literature, and it has some guiding significance for this research. However, the differences between this article and this paper are as follows
The control group differs, our study excluded patients with cervical cerclage, and Yi-Quan Xiong did not. 2. We contain 7 studies and 4 in Xiong. 3. In Xiong's study, no subgroup analysis was performed based on cervical length, which may lead to biased results. As Saccone G [37] said, the Arabin pessary does not reduce the rate of spontaneous preterm delivery or improve perinatal outcome to singleton pregnancies with a TVU CL ≤25mm at 20+0 -24+6 weeks. But Laia Pratcorona proved that Arabin cervical pessary did significantly reduce the spontaneous preterm birth rate <37 weeks, threatened preterm labor recurrence, and the preterm premature rupture of membranes rate[38]. However, Saccone G had only 3 RCT, and did not classify patients according to the risk of PTB. Actually, merely research divided patients as the risk of PTB. Our team think the patients with high-risk of PTB should be paid more attention than low risk patients. Because for singleton pregnancies with high-risk of PTB, several researches have shown cervical pessary cannot improve the maternal outcomes and fetal outcomes [17,39]. As for Saccone G[40], it tries to explain the reasons why the pessary was effective in the Goya and Liem trials and not in the Nicolaides trial. For example, proficiency of the doctor in placing the cervical pessary, imbalance in the number of patients in multiple study centers, time to remove the cervical pessary, percentage of patients with a previous history of SPTB, and statistical methods such as randomization. Otherwise, our team believe that different CL could cause different result. As table 1. Dang chooses the patients whose CL≤38mm, which was firstly shown in Leim’s research. Because of insufficient number of patients, Leim altered the cut off of cervical length to the 25th percentile. Owing to there is not clear classification of short cervix, it is possible that patients with CL≤38mm but CL≥25mm has some ability to pay for itself to prevent PTB occurrence in middle pregnancy. Therefore, those patients have better maternal outcome and fetal outcome. Is it over-medication when patients with CL≤38mm but CL≥25mm take cervical pessary? We cannot agree. Firstly, there is no consensus on short cervix. In 2019, research has shown that CL≤36.5 mm and ≤33.5 mm at 20-24 weeks of gestation could predict preterm birth <32 weeks and <34 weeks respectively[41].Then, G Pagani put forward that the optimal cut-off value for predicting PTB was 36 mm (sensitivity, 64.1%; specificity, 62.8%; positive predictive value, 13.5%; negative predictive value, 95.1%; accuracy, 62.9%), and more than one-third (36%) of PTB cases delivering < 32 weeks had a normal CL (CL≥20mm[42])in mid-gestation [43]. Finally, as the fetus grows or the number of fetus increases, the risk of PTB is increasing[44]. Therefore, it is reasonable when patients with CL≤38mm but CL≥25mm take cervical pessary. As for Jin Zhen[45]published in 2019, there are several differences with us. The main meta-analysis show that cervical pessary could prolong pregnancy and reduce the rate of tocolysis and corticosteroids. However, subgroup-analysis of twin pregnant patients show cervical pessary could not decrease the preterm birth rate before 28 weeks and 34 weeks[45]. In all 8 research articles included, only 3 RCT are about twin pregnant patients. More RCT are needed to prove this conduct. As for D'Antonio [21] published in 2021, this net meta-analysis included cervical pessary, any type of progesterone, and cervical cerclage, total 26 studies. They insisted that cervical pessary, progesterone and cerclage do not show a significant effect in reducing the rate of PTB or perinatal morbidity in twins, either when these interventions are applied to an unselected population of twins or in pregnancies with a short cervix. However, cervical cerclage is an invasive way, which could cause the preterm birth and PPROM. As for cervical pessary, our data show it is safe to twin pregnant patients. Otherwise, Wetta et al [46]believed that placement of pessary in the vagina did not result in any complicated adverse effects. The most common side effects were increased vaginal secretions, pain and discomfort among others. On investigation, Goya et al [47] found that the increase in vaginal discharge was not due to infection but due to stimulation caused by the placement of foreign body in the vagina. He surmised that vaginal pessary did not cause adverse effects in pregnant women and if the patient experienced unbearable pain, she could request removal of the pessary. In the 190 patients studied, only one had the pessary removed. Also, 95% of the patients still recommended the use of cervical pessary to others. This is why we excluded the patients accepted cervical cerclage.
3.4 Contraindications in placement of the pessary
In table 1, only Norman 2021, Berghella 2017 ,and Merced 2019 clearly illustrate that exclusion patients with bulging fetal membranes at the time of recruitment[16] [48],PROM[48] [18,23,33]and cervix dilation[16]. Others are no detail available. We noticed this difference and we decided to obey China Guidelines for the clinical management of twin pregnancies (updated for 2020) to make a criteria[8].Chinese guideline recommends that cervical cerclage may prolong the pregnancy and reduce the incidence of preterm labor. pregnancy and reduce the incidence of preterm labour in twin pregnancies with CL< 15 mm or cervical dilatation >10mm. SOGC said patients with CL< 15 mm, there may be an advantage to cerclage[10]. Otherwise, thanks to Monari F’s case report[49] , we noticed the importance of GBS (+) even though low bacterial load. Although further research has shown that there is evidence to suggest that preterm birth is associated with maternal GBS colonization, especially where there is evidence of ascending infection (bacteriuria)[50]. But guidelines [51-54] recommends patients with asymptomatic bacteriuria (≥105 cfu/ml) should take treatment[53,54]. There is not consensus about asymptomatic bacteriuria (<105 cfu/ml), which deserve to be paid more attention. All in all, based on guidelines, consensus and clinical experience, PROM, cervical dilation >10 mm, vaginal infection, and several particular situations (patients who needed to receive fetoscopy, abnormal fetal development, medically indicated preterm birth of medical origin such as twin-twin transfusion syndrome, severe preeclampsia, placenta abruption, placenta previa, prenatal bleeding, etc.al.) should be contraindications in placement of the pessary. As for CL <15mm without cervical dilation, we think there are several factors influence placement success rate of cervical pessary, such as race, medical proficiency, patients ‘personal medical history, PPROM history, maternity history, cervical operation, choriogenin, ect.al. Therefore, currently, we need more RCTs to measure the safety of cervical pessary based on race, different CL, PPROM history, maternity history, etc.al.
3.5 Long-term effects of cervical pessary
In terms of the long-term effects of cervical pessary, only Noor E [55]followed up participants for up to four years based on the Leim study. The results showed that the intervention group CL≤38mm, but no difference in abnormal growth and development outcomes between the two groups. Van published his RCT research which evaluated the effect of a cervical pessary on the outcome of subsequent pregnancies and maternal quality of life four years after twin pregnancy among 408 women [56].The results showed that no long term effects of pessary use on the outcome of subsequent pregnancies and maternal quality of life. However, there were a large number of missed visits in the study, so at present, there is still insufficient data to prove that cervical care can lead to long-term adverse outcomes in mothers.
3.6 Efficacy and economic benefits of cervical pessary
In 2014, Leim concluded that the cost of treatment in the cervical pessary group was comparable to that of the control group when comparing costs alone. However, when the cervical length was less than 38 mm, the placement of a cervical pessary not only prolonged the gestational cycle and reduced adverse neonatal outcomes, but also, was less costly than in the control group [57]? In 2020, one study[58] has proposed that after comparing the efficacy and economic benefits of cervical pessary with vaginal progesterone, cervical care improved adverse pregnancy outcomes and reduced costs. The connection between pessary and his economic effect still requires sufficient data support.
3.7 Strengths and limitations
7 RCT studies were included with a total of 3120 patients who performed a subgroup analysis based on different CL and type of cervical pessary. The results proved that cervical pessary could prolong the delivery weeks. Particularly, it effectively reduces the preterm birth rate of twins before 34 weeks for patients with CL less than 38mm, effectively prolong gestational week, reduce neonatal mortality, neonatal necrotic enterocolitis, and neonatal sepsis, and effectively improve the adverse pregnancy outcome. There are shortcomings in this research. First, even if more than 3,000 patients were included, the results were still affected by insufficient sample size and uneven sample distribution, resulting in altered results after sensitivity analysis. Second, only one of the seven studies included was about the efficacy comparison of cervical pessary placement and vaginal progesterone, which brought some bias to our study. At the same time, the researchers regretted that the inability to compare the treatment effect of cervical pessary with vaginal progesterone to prevent premature birth in twin patients had failed. Furthermore, only one study included was from Asia, and researchers similarly regret the inability to perform a race-based subgroup analysis. Otherwise, the subjects were unselected twin pregnancies and had no clear requirements for the mode of pregnancy (ART or non-ART), choriogenin, medical history (with a history of miscarriage, delivery and cervical surgery), which may bias the results. For this part of the patients, additional attention is needed. Alternatively, timing differences in the inclusion literature exist to the current lack of uniform guidelines. It is seen that most of the pessary were placed between 16 – 24 weeks, but Merced was at 24 – 34 weeks. Norman chooses patients with CL < 35mm. Those reasons for this difference are selection bias due to the different subjects selected each study.
3.8 Implications for practice and research
Despite the multiple regrets, our approach is scientific, and the results are valid. This paper reverses the conclusion proposed in the previous meta-analysis and guidelines that "cervical pessary cannot effectively prolong gestational weeks and prevent preterm birth in twin pregnancies” and proves the effectiveness of cervical trust placement in patients with twin pregnancies.
Conclusion
- Cervical pessary can extend the gestational week of short-cervix twin pregnancy without clinical symptoms, reduce the premature birth rate before 34 weeks of gestation, improve pregnancy outcome, reduce neonatal mortality, reduce neonatal enterocolitis incidence, neonatal sepsis incidence, and improve neonatal
- For patients with a cervical length less than 38mm, cervical pessary can be performed to extend the gestational
- For patients with cervical length less than 25mm, cervical pessary can effectively prolong the gestational age and improve the maternal and fetal
- Cervical pessary is safe for patients with twin
- Although, different CL seems to do not affect the effect of cervical pessary, especially on sptb<34 weeks, ptb<34 weeks and low birth weight, but patients with CL ≤38mm have great effect and less side effect, so we suggest that twin-pregnant-patients with CL≤38mm should consider to take cervical pessary in advance. Patients with CL≤25mm could take cervical pessary in order to prevent preterm birth before 34 weeks, but side effect of cervical pessary to patients with CL≤25 mm is still need more
- In terms of long-term efficacy, there is no evidence of cervical support placement on the long-term maternal
- In terms of economic benefits, cervical support is better than vaginal progesterone, but the conclusion still needs more research to
- The influence from different type of cervical pessary needs more
Acknowledgement
We are grateful to Mr. Wu, Mrs. Ma and Mrs. Huang for their contribution to this article on data collecting, writing, and polishing this paper. Mrs. Wang approved this project and participated in all parts. Mrs. Ma and Mrs. Huang were helped in data collecting. Mr. Wu polished this paper and provided several precious advice about data analysis. Wang bo, Sun xin and Lin lin are brilliant doctor and share them precious clinical experience about short CL with us, which inspired us and encouraged our work. Mrs. Huang recheck this paper at last. This work has registered in PROSPERO. This study is not sponsored by any individuals or organizations, and there are no conflicts of interest or ethical challenges. There are no conflicts of interest between any researchers.
References
- Song P, Theodoratou E, Li X, et Causes of death in children younger than five years in China in 2015: an updated analysis. Journal of global health. 2016 Dec;6(2): 020802.
- Lynch A M, Wagner B D, Hodges J K, et The relationship of the subtypes of preterm birth with retinopathy of prematurity. Am J Obstet Gynecol. 2017 Sep;217(3): 354.e1-354.e8.
- Catov J M, Scifres C M, Caritis S N, et Neonatal outcomes following preterm birth classified according to placental features. American journal of obstetrics and gynecology. 2017 Apr;216(4): 411.e1-411.e14.
- Monari F, Chiossi G, Ballarini M, et Perinatal outcomes in twin late preterm pregnancies: results from an Italian area-based, prospective cohort study. Ital J Pediatr. 2022 Jun 16;48(1): 101.
- Houlihan C, Poon L C, Ciarlo M, et Cervical cerclage for preterm birth prevention in twin gestation with short cervix: a retrospective cohort study. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2016 Dec;48(6): 752-756.
- Huang X, Saravelos S H, Li T C, et al. Cervical cerclage in twin pregnancy. Best practice & research Clinical obstetrics & gynaecology. 2019 Aug;59: 89-97.
- Vogel J P, Chawanpaiboon S, Moller A B, et al. The global epidemiology of preterm birth. Best Pract Res Clin Obstet 2018 Oct; 52: 3-12.
- Guidelines for the clinical management of twin pregnancies (updated for 2020). Chinese Journal of Perinatal 2020 (08):505-516.
- Berghella V, Rafael T, Szychowski J, et al. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: a meta-analysis. Obstetrics and 2011;117(3): 663-671.
- Brown R, Gagnon R, Delisle MF. No. 373-Cervical Insufficiency and Cervical Cerclage. J Obstet Gynaecol Can. 2019 Feb;41(2): 233-247.
- Arabin B, Alfirevic Z. Cervical pessaries for prevention of spontaneous preterm birth: past, present and future. Ultrasound Obstet 2013 Oct;42(4): 390-399.
- Mendoza Cobaleda M, Ribera I, Maiz N, et al. Cervical modifications after pessary placement in singleton pregnancies with maternal short cervical length: 2D and 3D ultrasound evaluation. Acta Obstet Gynecol Scand. 2019 Nov;98(11): 1442-1449.
- Pratcorona L, Goya M, Merced C, et al. Cervical pessary to reduce preterm birth <34 weeks of gestation after an episode of preterm labor and a short cervix: a randomized controlled trial. Am J Obstet Gynecol. 2018 Jul;219(1): 99 e1-99
- Saccone G, Maruotti GM, Giudicepietro A, et al. Effect of Cervical Pessary on Spontaneous Preterm Birth in Women With Singleton Pregnancies and Short Cervical Length: A Randomized Clinical Trial. Jama. 2017 Dec 19;318(23): 2317-2324.
- Di Tommaso M, Seravalli V, Arduino S, et al. Arabin cervical pessary to prevent preterm birth in twin pregnancies with short cervix. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and 2016 Aug;36(6): 715-718.
- Merced C, Goya M, Pratcorona L, et al. Cervical pessary for preventing preterm birth in twin pregnancies with maternal short cervix after an episode of threatened preterm labor: randomised controlled Am J Obstet Gynecol. 2019 Jul;221(1):55 e1-55 e14.
- Conde-Agudelo A, Romero R, Nicolaides KH. Cervical pessary to prevent preterm birth in asymptomatic high- risk women: a systematic review and meta-analysis. Am J Obstet 2020 Jul;223(1): 42-65.e2.
- Nicolaides K H, Syngelaki A, Poon LC, et al. Cervical pessary placement for prevention of preterm birth in unselected twin pregnancies: a randomized controlled Am J Obstet Gynecol. 2016 Jan;214(1):3 e1-9.
- ACOG Practice Bulletin No.142: Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014 Feb;123(2 Pt 1): 372-379.
- The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Annals of Internal Medicine. 2009.
- D'Antonio F, Berghella V, Di Mascio D, et al. Role of progesterone, cerclage and pessary in preventing preterm birth in twin pregnancies: A systematic review and network meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021 Jun;261: 166-177.
- Practice bulletin 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012 Oct;120(4):964-73.
- Dang V Q, Nguyen L K, Pham T D, et al. Pessary Compared With Vaginal Progesterone for the Prevention of Preterm Birth in Women With Twin Pregnancies and Cervical Length Less Than 38 mm: A Randomized Controlled Obstet Gynecol. 2019 Mar;133(3): 459-467.
- Liem S M, Schuit E, van Pampus M G, et al. Cervical pessaries to prevent preterm birth in women with a multiple pregnancy: a per-protocol analysis of a randomized clinical Acta Obstet Gynecol Scand. 2016 Apr;95(4): 444-451.
- Fox N S, Gupta S, Lam-Rachlin J, et al. Cervical Pessary and Vaginal Progesterone in Twin Pregnancies With a Short Obstet Gynecol. 2016 Apr;127(4): 625-630.
- França M S, Hatanaka A R, Andrade Junior V L, et al. Cervical Pessary Plus Progesterone for Twin Pregnancy with Short Cervix Compared to Unselected and Non-Treated Twin Pregnancy: A Historical Equivalence Cohort Study (EPM Twin Pessary Study). Rev Bras Ginecol Obstet. 2020 Oct;42(10): 621-629.
- Daskalakis G, Zacharakis D, Theodora M, et al. Safety and efficacy of the cervical pessary combined with vaginal progesterone for the prevention of spontaneous preterm J Perinat Med. 2018 Jul 26;46(5): 531-537.
- Liu J, Song G, Meng T, et Vaginal progesterone combined with cervical pessary in preventing preterm birth: a meta-analysis. J Matern Fetal Neonatal Med. 2021 Sep;34(18):3050-3056.
- Karbasian N, Sheikh M, Pirjani R, et al. Combined treatment with cervical pessary and vaginal progesterone for the prevention of preterm birth: A randomized clinical J Obstet Gynaecol Res. 2016 Dec;42(12): 1673-1679.
- Berghella V, Dugoff L, Ludmir J. Prevention of preterm birth with pessary in twins (PoPPT): a randomized controlled Ultrasound Obstet Gynecol. 2017 May;49(5): 567-572.
- Kyvernitakis I, Arabin Re: Prevention of preterm birth with pessary in twins (PoPPT): a randomized controlled trial. Ultrasound Obstet Gynecol. 2017 Sep;50(3): 408-409.
- Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): a multicentre, open-label randomized controlled trial. Lancet. 2013 Oct 19;382(9901): 1341-
- Goya M, de la Calle M, Pratcorona L, et al. Cervical pessary to prevent preterm birth in women with twin gestation and sonographic short cervix: a multicenter randomized controlled trial (PECEP-Twins). Am J Obstet 2016 Feb;214(2): 145-152.
- Nicolaides K H, Syngelaki A, Poon LC, et al. Cervical pessary placement for prevention of preterm birth in unselected twin pregnancies: a randomized controlled Am J Obstet Gynecol. 2016 Jan;214(1):3.e1-9.
- Jarde A, Lutsiv O, Park CK, et al. Preterm birth prevention in twin pregnancies with progesterone, pessary, or cerclage: a systematic review and meta-analysis. 2017 Jul;124(8):1163-1173.
- Xiong Y Q, Tan J, Liu Y M, et al. Cervical pessary for preventing preterm birth in singletons and twin pregnancies: an update systematic review and meta-analysis. J Matern Fetal Neonatal 2020 Jan 16: 1-10.
- Saccone G, Ciardulli A, Xodo S, et al. Cervical Pessary for Preventing Preterm Birth in Singleton Pregnancies With Short Cervical Length: A Systematic Review and Meta-analysis. J Ultrasound Med. 2017 Aug;36(8): 1535-
- Pratcorona L, Goya M, Merced C, et al. Cervical pessary to reduce preterm birth <34 weeks of gestation after an episode of preterm labor and a short cervix: a randomized controlled Am J Obstet Gynecol. 2018 Jul;219(1):99.e1-99.e16.
- Care A, Nevitt S J, Medley N, et al. Interventions to prevent spontaneous preterm birth in women with singleton pregnancy who are at high risk: systematic review and network meta-analysis. 2022 Feb 15;376: e064547.
- Saccone G, Ciardulli A, Xodo S, et al. Cervical pessary for preventing preterm birth in twin pregnancies with short cervical length: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2017 Dec;30(24):2918-
- Zuo X F, Du Y F, Yang J, et al. Predictive value of cervical length measured by transvaginal ultrasound during the second and the third trimester of pregnancy for preterm birth in twin pregnancies. Zhonghua Fu Chan Ke Za Zhi. 2019 May 25;54(5): 318-323.
- Conde-Agudelo A, Romero R, Hassan S S, et al. Transvaginal sonographic cervical length for the prediction of spontaneous preterm birth in twin pregnancies: a systematic review and metaanalysis. Am J Obstet Gynecol. 2010 Aug;203(2):128.e1-12.
- Pagani G, Stagnati V, Fichera A, et al. Cervical length at mid-gestation in screening for preterm birth in twin Ultrasound Obstet Gynecol. 2016 Jul;48(1): 56-60.
- Hiersch L, Rosen H, Okby R, et al. The greater risk of preterm birth in triplets is mirrored by a more rapid cervical shortening along gestation. Am J Obstet 2016 Sep;215(3):357.e1-6.
- Jin Z, Chen L, Qiao D, et al. Cervical pessary for preventing preterm birth: a meta-analysis. J Matern Fetal Neonatal 2019 Apr;32(7): 1148-1154.
- Wetta L A, Biggio J R, Jr. Cervical pessary use and preterm birth. Clin Obstet Gynecol. 2014 Sep;57(3): 607-
- Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): an open-label randomised controlled Lancet. 2012 May 12;379(9828): 1800-1806.
- Norman J E, Norrie J, MacLennan G, et al. The Arabin pessary to prevent preterm birth in women with a twin pregnancy and a short cervix: the STOPPIT 2 Health Technol Assess. 2021 Jul;25(44): 1-66.
- Monari F, Salerno C, Torcetta F, et al. Intrapartum stillbirth for sepsis complicating Arabin cervical pessary placement in a twin pregnancy. Minerva Obstet 2021 Jun;73(3): 384-387.
- Bianchi-Jassir F, Seale A C, Kohli-Lynch M, et al. Preterm Birth Associated With Group B Streptococcus Maternal Colonization Worldwide: Systematic Review and Meta-analyses. Clin Infect Dis. 2017 Nov 6;65(suppl_2): S133-s142.
- Dagklis T, Sen C, Tsakiridis I, et al. The use of antenatal corticosteroids for fetal maturation: clinical practice guideline by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine foundation. J Perinat 2022 May 25;50(4): 375-385.
- Allen V M, Yudin M H. No. 276-Management of Group B Streptococcal Bacteriuria in Pregnancy. J Obstet Gynaecol 2018 Feb;40(2): e181-e186.
- Prevention of Group B Streptococcal Early-Onset Disease in Newborns: ACOG Committee Opinion, Number Obstet Gynecol. 2020 Feb;135(2): e51-e72.
- Perinatal Medicine Branch of the Chinese Medical Association, Obstetrics and Gynecology Section of the Chinese Medical Expert consensus on the prevention of perinatal group B streptococcal disease (China). Chinese Journal of Perinatal Medicine.2021;24(8): 561-566.
- Simons N E, van de Beek C, van der Lee J H, et al. Child outcomes after placement of a cervical pessary in women with a multiple pregnancy: A 4-year follow-up of the ProTWIN trial. Acta Obstet Gynecol Scand. 2019 Oct;98(10): 1292-1300.
- van Limburg Stirum E V J, Zegveld S J, Simons N E, et al. Consequences of cervical pessary for subsequent pregnancies: follow-up of randomized clinical trial (ProTWIN). Ultrasound Obstet Nov 26 (2021).
- Liem S M, van Baaren G J, Delemarre F M, et al. Economic analysis of use of pessary to prevent preterm birth in women with multiple pregnancy (ProTWIN trial). Ultrasound Obstet 2014 Sep;44(3): 338-345.
- Le K D, Nguyen L K, Nguyen L T M, et al. Cervical pessary vs vaginal progesterone for prevention of preterm birth in women with twin pregnancy and short cervix: economic analysis following randomized controlled trial. Ultrasound Obstet 2020 Mar;55(3): 339-347.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 