Metastatic Large Cell Neuroendocrine Carcinoma of the Endometrium: A Case Report and Literature Review
Gonzalez-Bosquet E3*, Gaba L1, Saco MA2, Gil-Ibañez B3, Fuster P3, Glickman A3, Torne A3
1Department of Oncology, Hospital Clinic, University of Barcelona, Spain
2Department of Pathology, Hospital Clinic, University of Barcelona, Spain
3Department Gynecology Oncology, Hospital Clinic, University of Barcelona, Spain
*Corresponding Author: Gonzalez-Bosquet E, Department Gynecology Oncology, Hospital Clinic, University of Barcelona, Spain
Received: 19 November 2018; Accepted: 19 December 2018; Published: 24 December 2018
Article Information
Citation:
Gonzalez-Bosquet E, Gaba L, Saco MA, Gil-Ibañez B, Fuster P, Glickman A, Torne A. Metastatic Large Cell Neuroendocrine Carcinoma of the Endometrium: A Case Report and Literature Review. Obstetrics and Gynecology Research 1 (2018): 094-100.
View / Download Pdf Share at FacebookAbstract
Neuroendocrine neoplasm occurs predominantly in the lungs, but can be occasionally found in the gastrointestinal and genitourinary tracts [1]. When this neoplasia affects the genital tract, usually involve the uterine cervix and the ovary [2]. Neuroendocrine tumors are classified as poorly-differentiated and well differentiated, and further categorized into small and large cell neuroendocrine carcinomas. Approximately only 90 cases of small cell neuroendocrine carcinoma of the endometrium have been reported [3,4]. Studies of large cell endometrial neuroendocrine carcinoma (LCNEC) are even less common, with only 16 cases documented [1,5,6]. Our case concerns a 58-year-old woman with a metastatic LCNEC arising from the endometrium. We, correspondingly, also reviewed the literature and emphasize the most important diagnostic and therapeutic aspects of this rare clinical entity.
Keywords
<p>Neuroendocrine Carcinoma</p>
Article Details
Case report
A 58-year-old woman was referred to our hospital with postmenopausal vaginal bleeding. Her obstetric history included two cesarean sections, the last of them due to a twin gestation obtained by in vitro fertilization. She experienced onset of menopause at age 52 and was treated for 5 years with hormone replacement therapy for her menopausal symptoms. Her gynecological history included endometriosis and miomatosis. The woman reported smoking two packs of cigarettes per year.
The gynecological examination showed a vaginal solid tumor of 2 cm of diameter located on the middle part of the anterior
vaginal wall. Upon palpation, the uterus was enlarged, and the cervix was mobile. A subsequent rectal examination ruled out parametrial involvement. A biopsy of the vaginal tumor and the endometrium was then performed. The histological analysis of the vagina and endometrium biopsy revealed a LCNEC grade 3, with a Ki67 index of 45% and 24 mitosis per 10 high power fields (Figure 1 and 2). A magnetic resonance (MRI) was performed observing an enlarged uterus with a poorly defined tumor of 3 cm that diffusely infiltrated the myometrium, enlarged pelvic nodes and bone lesions in the sacrum and acetabulum; suggestive of a malignant uterine neoplasm with lymphatic and bone metastases.
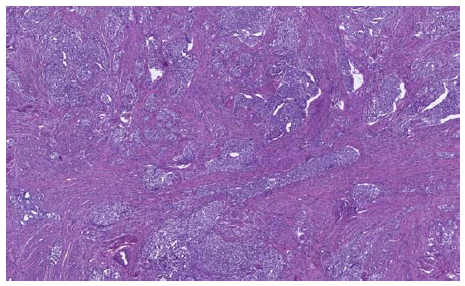
Figure 1: Well demarcated nest and island of large atypical cells with organoid pattern, infiltrating uterine corpus (H&E 40x).
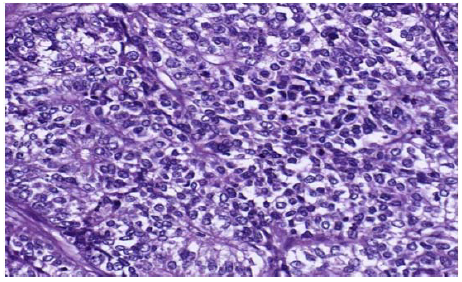
Figure 2: Large tumor cells with pleomorphic and hyperchromatic nuclei and scanty cytoplasm showing occasional rosette-like structures (H&E 200x).
Tumor marker levels were requested in blood. The values of these markers were: CEA 8.3 µg/L (reference level rl<5), Ca125 200 U/ml (rl<35) Ca19.9 52 U/ml (rl<37) , SCC 8.4 ng/ml (rl<2.5) , neuron specific enolase 69 ng/mL (rl<25) and Chromogranin A 1526 ng/mL (rl<450).
A 18Fluorine fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) was performed in order to rule out other affected organs. This exam confirmed uterine tumor (SUV of 9.7), left pelvic and inter aorto-cava lymphadenopathies (SUV of 3.7), and bone lesions in coxis and left iliac pelvis (SUV 8.8) and detected multiple and bilateral pulmonary lesions suggestive of metastases (SUV of 11.4) (Figure 3).
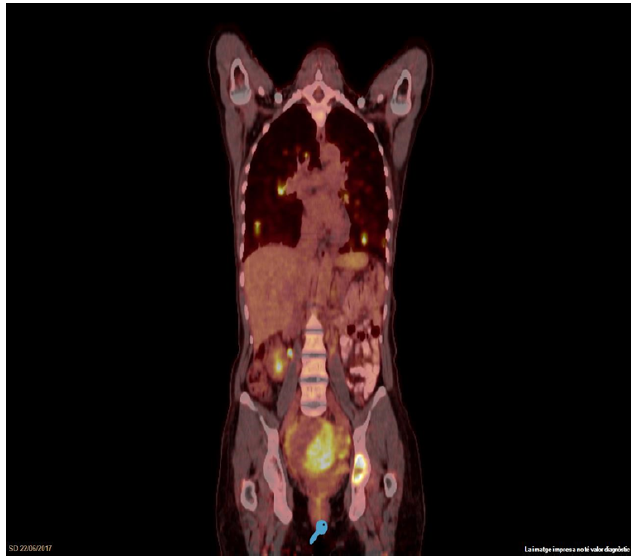
Figure 3: 18Fluorine fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) before first line chemotherapy
She was diagnosed as a stage IVb LCNEC of endometrium, according to the 2008 International Federation of Gynecology and Obstetrics (FIGO) staging. Octreoscan performed before beginning treatment revealed somatostatin receptor positive tissue in the endometrium.
Based on these findings, the patient received 6 cycles of chemotherapy with cisplatin and etoposide. Another PET/TAC scan was performed, four months after the beginning of chemotherapy, to evaluate the response to treatment. Pulmonary lesions were not detectable, and a demining of the pelvic pathological lesions (uterus [SUV of 2.42], lymphoid and bone [SUV of 3.8]) was observed (Figure 4). Tumor markers values after finishing chemotherapy were normal: Ca 125 36 U/mL, SCC 2.2 ng/mL, neuron specific enolase 12 ng/mL, except CEA 5.9 ng/ml and Chromogranin A 1180 ng/mL.
Our multidisciplinary oncology committee decided to perform a debulking surgery, including a hysterectomy and the removal of the vaginal tumor and enlarged pelvic lymph nodes, six months after diagnosis. The histologic analysis of the uterus and lymph nodes revealed a high grade LCNEC, affecting endometrium, lymph nodes and vagina. The tumor was positive to chromogranin and synaptophysin in 80% and 50% of neoplastic cells respectively. Lanreotide (a synthetic somatostatin analog) autogel 120 mg/28 days, as maintenance treatment, was prescribed due to an octreoscan captation before surgery.
One month later, the patient was admitted in the hospital due to hemoptisis. A pulmonary angio-CT was performed revealing multiple cavitated pulmonary nodules. Second line chemotherapy with Topotecan was indicated. 18 months after
the initial diagnosis the patient is alive, with persistent illness. Pulmonary lesions, lymph nodes and bone metastases are stable. The patient is still undergoing topetecan treatment.
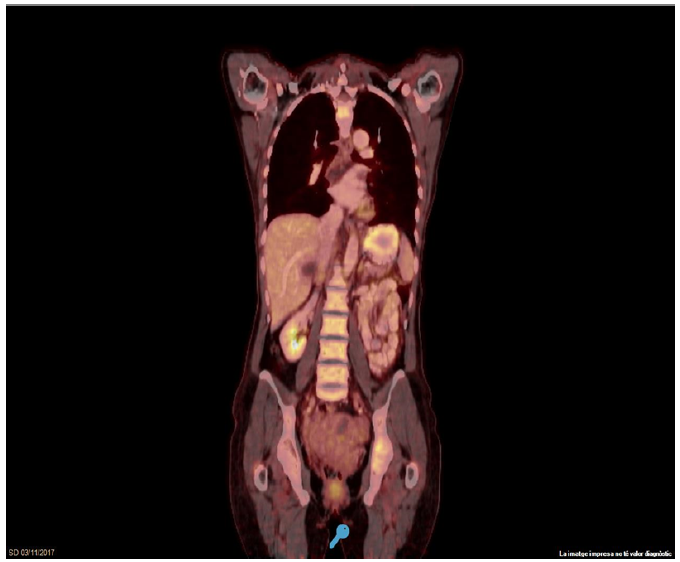
Figure 4: 18Fluorine fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) after 6 cycles of chemotherapy with cisplatin and etoposide
Discussion
In 2014 for the first time, neuroendocrine tumors were included in the histological classification of uterine corpus tumors in the WHO’s categorization of tumors of female reproductive organs [7]. According to the WHO classification of lung tumors, [8] LCNEC are diagnosed based on large cell carcinoma; large cell size with low nuclear to cytoplasm ratio, > 10 mitotic counts in 2 mm2 of viable tumor and the presence of neuroendocrine histology (organoid pattern with formation of nests, palisading, rosettes, or trabeculae with peripheral palisading), as well as one or more immunohistochemical positive neuroendocrine markers (chromogranin, synaptophysin, or CD56). In our case, the tumor was positive to chromogranin and synaptophysin in 80% and 50% of tumoral cells, respectively. 16 cases of endometrial LCNEC described in literature demonstrated at least two positive-stained neuroendocrine markers in the immunohistochemical assays [1].
It is difficult to give a preoperatory definitive histologic diagnosis on small specimens [1,5]. In our case, this was possible as we were able to obtain more material from two biopsies of the endometrium and vagina.
The age of diagnosis of the 16 cases described in literature, range from 40 to 88 years old with a mean of 63.4 years old [1], the majority of which were postmenopausal, like our case (58-years old). The most common initial symptom was postmenopausal bleeding (12/17 cases), like our patient’s case.
Smoking and endometrial LCNEC has yet to be investigated thoroughly. Only one study reported a patient with LCNEC who had smoked two packs of cigarettes per day for more than 30 years [9]. Our patient smoked only two packets of cigarettes per year, which would not appear to be consequential.
Makihara et al observed MR findings of LCNEC which seemed to mimic MRI findings in other poorly differentiated endometrial adenocarcinomas and uterine sarcomas [10].
Blood tumor marker Ca-125 could be elevated in cases of LCNEC [1]; in our case Ca-125 was elevated to 200. Tumor markers levels could be used for monitoring treatment response. Treglia et al observed that 18F-FDG PET/TAC may provide useful prognostic information in patients with high-grade neuroendocrine tumors, like our patient’s case [11].
It is clear that multi-modality approach is required for the treatment of this rare tumors with a poor prognosis.
There is no surgical standard for this rare histology and treatment depends on stage of the tumor. As in our case, hysterectomy and bilateral salpingo-oophorectomy is the surgical procedure more commonly used (11/16) [1]. There are only 4 recorded cases of radical hysterectomy being performed. Lymph node dissection is performed in 9 of the 16 cases described in literature [1]; in our case we performed a pelvic debulking of enlarged suspicious pelvic lymph nodes. Omentectomy was performed in 8 cases of the 16 described in literature [1]. Although complete surgical staging with omentectomy and pelvic and paraaortic lymphadenectomy is required for accurate staging of uterine cancer, Nguyen et al observed 8 of the 13 reported cases of endometrial LCNEC presented in advanced FIGO stage III or IV disease. Given the poor prognosis of the disease, even following surgical debulking, some authors may consider administering neoadjuvant chemotherapy when a preoperative diagnosis is possible [12], as we conducted on our patient.
There is limited data concerning adjuvant or neoadjuvant treatment of LCNEC of the endometrium, also in first line setting. Platinum and Etoposide based chemotherapy is generally used, by extrapolating data from LCNEC of the lung, since data for cervical and uterine endocrine tumors is limited [13,14]. We used Etoposide and Platinum as first line therapy, with partial response of the disease. After relapse, we treated the patient with second line chemotherapy with Topotecan, based on LCNEC recommendations. Other therapies, in second line chemotherapy, reported by other authors are; cyclophosphamide/doxorubicin/Vincristine (CAV) and irinotecan/platinum (IP) [10,14-16).
As was our case, two authors have reported the use of somatostatin analog with combination with chemotherapy for the treatment of two advanced cases of endometrial neuroendocrine tumors. One case demonstrated a partial response, while a second patient exhibited a progression of the disease [6,17]. Astatine-211-labeled octreotide (somatostatin analog) has been described as a potential radiotherapeutic agent for neuroendocrine lung tumors with promising results [18].
Radiotherapy is also used by other authors as adjuvant treatment for LCNEC, 7 of the 16 patients treated with radiotherapy, 3 survived > 12 months and 4 lived without disease relapse [1].
No prognosis data is available for LCNEC of the endometrium. Even for early stages appears to have an aggressive course with a strong propensity for distance mestastasis and rapid recurrence [12]. Of the 17 cases described in literature, including our case, 11 were stage 3 or 4 at diagnosis, 8 patients died between 1-19 months (mean 10) after diagnosis and 9 remain alive; two of them with a recurrence or persistence. In all cases, follow up is short (less two years).
Conclusion
Endometrial LCNEC is a very rare endometrial tumor with poor prognosis and represents a challenge in the clinical practice. Adjuvant therapy with chemotherapy and/or radiotherapy appears to improve survival rates. Cytoreductive surgery including; hysterectomy bilateral salpingo-oophorectomy, and debulking of affected pelvic or paraaortic lymphnodes is the most common surgical treatment. PET/TAC is usefull in the management of these aggressive tumors. More studies are needed to establish more efficient models of treatment to improve the survival rates of endometrium LCNEC.
References
- Tu YA, Chen YL, Lin MC, Chen CA, Cheng WF. Large cell neuroendocrine carcinoma of the endometrium: A case report and literature review. Taiwanese Journal of Obstet Gynecol 57 (2018): 144-149.
- Albores-Saavedra J, Martinez-Benitez B, Luevano E. Small cell carcinomas and large cell carcinomas of the endometrium and cérvix: polypoid tumors and those arising in polyps may have a favorable prognosis. Int J Gynecol Pathol 27 (2008): 333-339.
- Rouzbahman M, Clarke B. Neuroendocrine tumors of the gynecologic tract: select topics. Semin Diagn Pathol 30 (2013): 224–233.
- Atienza-Amores M, Guerini-Rocco E, Soslow RA, et al. Small cell carcinoma of the gynecologic tract: a multifaceted spectrum of lesions. Gynecol Oncol 134 (2014): 410–418.
- Deodhar KK, Kerkar RA, Suryawanshi P, et al. Large cell neuroendocrine carcinoma of the endometrium: an extremely uncommon diagnosis, but worth the efforts. J Cancer Res Ther 7 (2011): 211–213.
- Shahabi S, Pellicciotta I, Hou J, Graceffa S, Huang CS, Samuelson RN et al. Clinical utility of chromogranin A and octreotide in large cell neuroendocrine carcinoma of the uterine corpus. Rare Tumors 3 (2011): e41.
- Ono K, Yokota NR, Yoshioka E, Noguchi A, Washimi K, Kawachi K et al. Metastatic large cell neuroendocrine carcinoma of the lung arising from the uterus: A pitfall in lung cáncer diagnosis. Pathology Researche a Practice 212 (2016): 654-657.
- Travis WD, Brambilla E, Nicholson AC, Yatabe Y, Austin JH, Beasly MB et al. The 2015 World Health Organization Classification of lung tumors: impact of genetic, clinical and radiologic advances since 2004 classification. Torac Oncol 10 (2015): 1243-1260.
- Erhan Y, Dikmen Y, Yucebilgin MS, Zekioglu O, Mgoyi L, Terek MC. Large cell neuroendocrine carcinoma of the uterine corpus metastatic to brain and lung: case report and review of the literature. Eur J Gynaecol Oncol 25 (2014): 109-112.
- Maquilara N, Maeda T, Nishimura M, Deguchi M, Sonoyama A, Nakamayasi K et al. Large cell neuroendocrine carcinoma originating from the uterine endometrium: a report on magnetic resonance features of 2 cases with very rare and aggressive tumor. Rare tumor 4 (2012): e37.
- Treglia G, Kroiss AS, Piccardo A, Lococo F, Santhanam P, Imperiale A. Role of positron emission tomography in thyroid and neuroendocrine tumors. MinervaEndocrinol 43 (2018): 341-355.
- Nguyen MLT, Han L, Minors AM, Bentley-Hibbert S, Pradhan TS, Pua TL et. Rare large cell neuroendocrine tumor of the endometrium. A case report and review of the literature. International Journal of surgery case reports 4 (2013): 651-655.
- Gardner GJ, Reidy-Lagunes D, Gehring PA. Neuroendocrine tumors of the gynecologic tract: a Society of Gynecologic Oncology (SGO) clinical document. Gynecol Oncol 122 (2011): 190.
- Matsumoto H, Nasu K, Kai K, Nishida M, Narahara H, Nishida H. Combined large-cell neuroendocrine carcinoma and endometrium adenocarcinoma of the endometrium: a case report and survey of related literature. J obstet Gynaecol Res 42 (2016): 206-210.
- Shepherd FA, Evans WK, MacCormick R, Field R, Yau JC. Cyclophosphamide, doxorubicin, and vincristine in etoposide-and cisplatin-resistant small cell lung cancer. Cancer treat Rep 71 (1987): 941-944.
- O´Brien ME, Ciuleanu TE, Tsekov H, Shparyk Y, Cucevi a B, Juhasz G et al. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol 24 (2006): 5441-5447.
- Verschraegen CT, Matei C, Loyer E, Malpica A, Tornos C, Kudelka AP et al. Octreotide induced remission of a refractory small cell carcinoma of the endometrium. International Journal of Gastrointestinal Cancer 9 (1999): 80-85.
- Zhao B, Qin S, Chai L, Lu G, Yang Y, Cai H, Yuan X, Fan S, Huang Q, Yu F.Evaluation of astatine-211-labeled octreotide as a potential radiotherapeutic agent for NSCLC treatment. Bioorg Med Chem 26 (2018): 1086-1091.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 