Oligohydramnios and Its Maternal and Neonatal Outcomes: A Single Centre Study
Jinat Fatema1*, Tanzina Iveen Chowdhury2, Bidisha Chakma3, Mehera Parveen4, Kamrunnahar5, A. K. M Shahidur Rahman6, Tripti Rani Das7
1Medical Officer, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
2Assistant Professor, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Medical Officer, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
4Medical Officer, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
5Junior Consultant, Department of Obstetrics and Gynaecology, Sir Salimullah Medical College Mitford Hospital, Dhaka, Bangladesh
6Medical Officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
7Professor and Former Chairman, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding author: Dr. Jinat Fatema, Medical Officer, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
Received: 25 January 2024; Accepted: 30 January 2024; Published: 09 February 2024
Article Information
Citation: Fatema J, Chowdhury TI, Chakma B, Parveen M, Kamrunnahar, Rahman AKMS, Das TR. Oligohydramnios and Its Maternal and Neonatal Outcomes: A Single Centre Study. Obstetrics and Gynecology Research. 7 (2024): 08-15.
View / Download Pdf Share at FacebookAbstract
Background:
Oligohydramnios refers to amniotic fluid volume that is less than expected for gestational age. Oligohydramnios is a common complication of all pregnancies and has several consequences on pregnancy outcomes.
Objectives:
This study was aimed to assess the maternal and neonatal outcomes of pregnancy associated with oligohydramnios.
Methods:
This observational study was carried out at Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. A total of 50 pregnant women with oligohydramnios were enrolled. Data were collected by face-to-face interview. Their clinical examination and relevant investigations were done. Fetal outcomes were recorded accordingly. Collected data were analyzed following standard procedure.
Results:
In this study the mean(±SD) age of the study patients was 27.62±3.66 years. Multiparous was more common than primiparous (56% versus 44%). Of them, 60% study patients were 34-36 weeks of gestational age followed by 32% were 37-39 weeks and 8% were 40-42 weeks. Causes of oligohydramnios showed that; premature rupture of membrane (PROM) was associated with 28% study patients followed by placental insufficiency ((18%), intra-uterine growth retardation (IUGR) (14%), congenital anomalies (10%) and post-dated pregnancies (8%). Caesarean section rate was comparatively higher among women with oligohydramnios. Among 50 study patients only 16 patients had meconium-stained liquor which was 32%. A high rate (48.93%) of low birth weight (LBW) babies was observed among women with oligohydramnios. APGAR score was below 7 at 5 minutes among 48.93% babies, birth asphyxia and neonatal sepsis were high in babies of women with oligohydramnios. There were 5(10%) early neonatal death and 3(6%) still born.
Conclusion:
Oligohydramnios is common in multiparous. Caesarean section rate is higher among women with oligohydramnios. Low birth weight (LBW) babies are frequent in women with oligohydramnios. Birth asphyxia and neonatal sepsis are common morbidity among babies of women with oligohydramnios.
Keywords
<p>Pregnancy; Oligohydramnios; Fetal Outcome; Maternal Outcome</p>
Article Details
1. Introduction
Oligohydramnios is defined as a single reading of the amniotic fluid index (AFI) below 5 cm or 3 readings below 8 cm [1,2]. Although it affects only 4-5.5% of all pregnancies, oligohydramnios is an important problem due to its severe complications which include- antepartum and intrapartum fetal death, cord prolapse or compression, compression related limb deformities, and pulmonary hypoplasia [1]. The mechanism of amniotic fluid production and turnover are complex. It is produced soon after the amniotic sac forms at about 12 days after conception [2]. Several factors including fetal swallowing, micturition, respiratory tract secretion and transudation from maternal serum across the fetal membranes or from maternal circulation in the placenta, work in combination to produce a normal amniotic fluid that bathes the fetus and is necessary for its proper growth and development [3,4]. It cushions the fetus from physical trauma, permits fetal lung growth, and provides a barrier against infection [3]. Oligohydramnios is secondary to either an excess loss of fluid or 'a decrease in fetal urine production or excretion [4,5]. Normal amniotic fluid volume (AFV) varies according to the gestational age [5]. The average volume increases with gestational age, peaking at 800-1000 ml, which coincides with 36-37 weeks of gestation [6]. AFV increases steadily throughout most of the pregnancy, with a volume of about 30 ml at 10 weeks gestation and a peak of about 1L at 34-36 weeks gestation [5-7]. AFV decreases in the late third trimesters, with a mean AFV of 800 ml at 40 weeks of gestation [5-7]. The causes of oligohydramnios are the premature rupture of the fetal membrane (PROM), congenital abnormalities of the fetal urinary tract like renal agenesis, urethral obstruction, fetal polycystic kidney, placental insufficiency, twin-twin transfusion syndrome, post maturity, certain maternal health problems as high blood pressure and certain medications [8]. Chromosomal abnormalities, structural malformations, malformations of urogenital system are commonly associated with oligohydramnios that adversely affect the neonatal outcome [9]. Obstetrician providing health care often face a situation in which pregnant women is noted to have oligohydramnios both clinically and sonographically. Clinically in oligohydramnios the uterine size is much smaller than the period of amenorrhea and uterus is full of fetal size because of scanty liquor [9]. Sonographically accurate diagnosis of oligohydramnios become possible by ultrasonographic evaluation of amniotic fluid index (AFI) during pregnancy from 20 weeks to 40 weeks of pregnancy [10]. About 8% of pregnant women can have low levels of amniotic fluid, with about 4% being diagnosed as oligohydramnios [6]. If an amniotic fluid index (AFI) shows a fluid level of <5 cm (or <5th percentile), the absence of a fluid pocket 2-3 cm in depth, or a fluid volume of <500 ml at 32-36 weeks of gestation, then a diagnosis of oligohydramnios would be suspected [7,10-11]. In ultrasonography, normal amniotic fluid index is 8.1-20 cm. the patient with AFI between 5.1-8 cm have moderate oligohydramnios and the patient who have AFI less than or equal to 5 cm, have severe oligohydramnios [6-7,10]. The oligohydramnios can occur at any stages of pregnancy, but it is more common in the last trimester [12]. If oligohydramnios occurs at the early stages of pregnancy, the prognosis is poor [8]. If the pregnancy is overdue by two (2) weeks or more, the patient may be at risk for low amniotic fluid level since fluids can decrease by half, once pregnancy reaches at 42 weeks of gestation [12]. Oligohydramnios can cause complication in about 12% of pregnancies that go past 41 weeks of gestation [10]. Oligohydramnios identified during the antepartum period of pregnancy is associated with a variety of adverse neonatal outcome such as neonatal death, meconium-stained amniotic fluid, abnormal fetal heart tracing and required cesarean section for fetal distress in labor [8]. It was reported that oligohydramnios is a common complication of pregnancy that have poor maternal and fetal outcomes [4,9-10,13-15]. Proper diagnostic and monitoring facilities and standard protocol in the management of oligohydramnios can improve the maternal and neonatal outcomes. In this background current study was aimed to assess the maternal and neonatal outcomes of pregnancy associated with oligohydramnios.
2. Methodology
This prospective observational study was conducted at Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. The study protocol was approved by the ethical review committee, BSMMU, Dhaka, Bangladesh. A total of fifty (50) pregnant woman having oligohydramnios were included in this study by purposive sampling technique following selection criteria. Pregnant women with 34-42 weeks of pregnancy, sonographycally diagnosed as oligohydramnios were included. Pregnancy with intra-uterine death (IUD), multiple pregnancy and oligohydramnios of <34 week or >42 weeks of gestation were excluded from this study.
2.1. Study procedure
After selection of the study patients the purpose, procedure and benefits of the study were explained to them. Informed written consent was taken from each study patient. Then a detail case history was taken and relevant clinical examinations of all study patients were done accordingly. Their last menstrual period, expected date of delivery, gestational age with oligohydramnios (by ultrasonogram) and antenatal checkups were recorded. For each study patient a separate data collection sheet was used to maintain confidentiality. The highest levels of confidentiality along with optimum ethical standards were maintained during the analysis of the data.
2.2. Diagnosis of oligohydramnios
Oligohydramnios is defined as an amniotic fluid index (AFI) <5th percentile, as normal amniotic fluid volume changes with gestational age [16]. It has been described as:
- Decreased amniotic fluid volume.
- Amniotic fluid volume <500 ml at 32 to 36 weeks of gestation.
- Maximum vertical pocket (MVP) <2 cm.
- Amniotic fluid index (AFI) <5 cm or < 5th percentile, AFI <6.8 cm at term.
2.3. APGAR (appearance, pulse, grimace, activity and respiration) score [17-18]:
Assessment of the condition of the baby was done by using APGAR score in 1 minute and 5 minutes after delivery [17]. Scoring table is displaying below [18]
|
Sign |
0 |
1 |
2 |
|
Respiratory effort |
Absent |
Slow, irregular |
Good crying |
|
Hear rate |
Absent |
Slow (below 100/minute) |
Over 100/minute |
|
Muscle tone |
Flaccid |
Flexion of extremities |
Active body movement |
|
Reflex irritability |
No response |
Grimace |
Cry |
|
Color |
Blue, pale |
Body pink extremities blue |
Complete pink |
Interpretation:
- Total score= 10
- No depression if score= 7-10
- Mild depression if score= 4-6
- Severe depression if score= 0-3
2.4. Data analysis
All collected data were checked and edited first. Then data were processed with the computer-based software “Statistical Package for Social Sciences (SPSS)” for windows version 26. Qualitative data were expressed as mean with standard deviation (±SD) and quantitative data were expressed as frequency with percentage.
3. Results and Observation
This study was intended to assess various mode of presentation and outcome of pregnancy associated with oligohydramnios. Total 50 pregnant women with oligohydramnios were enrolled. The mean±SD age of the study patients was 27.62±3.66 years. Of them, 6% were age group less than 20 years, 34% was between 20-25 years, 44% were 26-30 years and 16% were 31-35 years (Table- 1). Of them; maximum (56%) study patients were multiparous followed by 44% were nulliparous (Figure-1). In this study, majority (60%) patients were between 34-36 weeks of gestational age followed by 32% were in 37-39 weeks of gestational age and 8% were in 40-42 weeks of gestational age (Figure-2).
|
Age in years |
Number of patients (n) |
Percentage (%) |
|
Mean±SD |
27.62±3.66 years |
|
|
<20 |
3 |
6 |
|
20-25 |
17 |
34 |
|
26-30 |
22 |
44 |
|
31-35 |
8 |
16 |
Table-1: Age distribution of the study patients (N= 50)
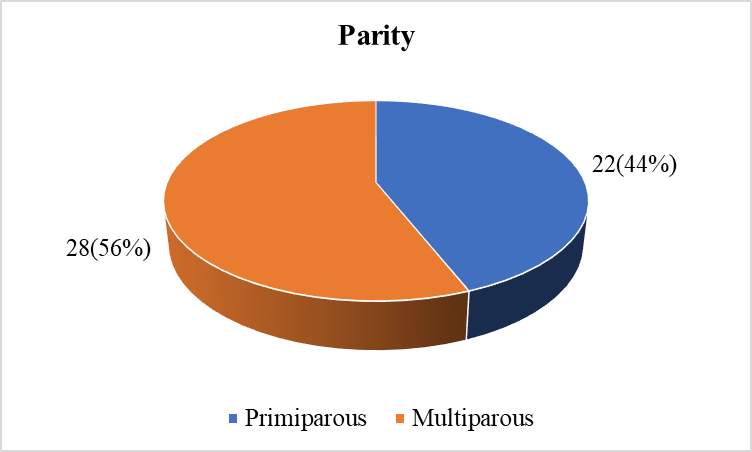
Figure-1: Parity of the study patients (N= 50)
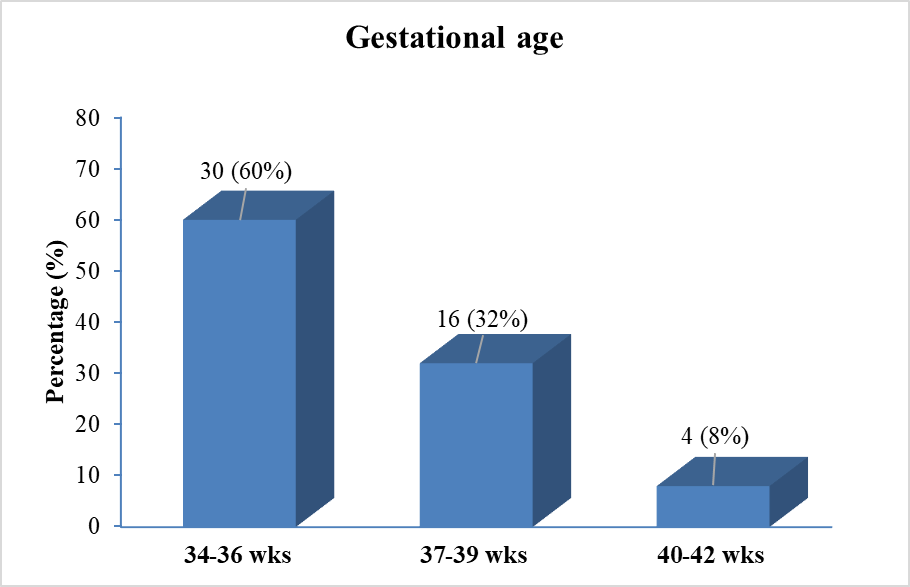
Figure-2: Distribution of the study patients according to gestational age (N= 50)
Among the study population; on the basis of amniotic fluid index (AFI) 32% patients exhibited borderline oligohydramnios, while a substantial percentage (68%) of study patients experienced severe oligohydramnios (Table-2).
|
Amniotic fluid index (AFI) |
Number of patients (n) |
Percentage (%) |
|
5-8 cm (Moderate oligohydramnios) |
16 |
32 |
|
<5 cm (Severe oligohydramnios) |
34 |
68 |
Table-2: Distribution of study patients on the basis of amniotic fluid index (AFI) (N= 50)
In this study, premature rupture of membrane (PROM) was identified as the most common cause of oligohydramnios affecting 28% of study patients. Congenital anomalies of the fetus contribute to oligohydramnios in 10% of study cases. Postdated pregnancy, intra-uterine growth retardation (IUGR) and placental insufficiency each account for 8% 14% and 18% of occurrences respectively. Notably, 22% of study cases present oligohydramnios without any apparent cause (Table-3).
|
Causes of oligohydramnios |
Number of patients (n) |
Percentage (%) |
|
PROM |
14 |
28 |
|
Congenital anomalies of fetus |
5 |
10 |
|
Postdated pregnancy |
4 |
8 |
|
PIH (placental insufficiency) |
9 |
18 |
|
IUGR |
7 |
14 |
|
Without any apparent cause |
11 |
22 |
Table-3: Causes associated with oligohydramnios among the study patients (N= 50)
Regarding the mode of delivery; 68% study patients needed caesarean section (C/S) and rest 32% was vaginal delivery (Table-4).
|
Mode of delivery |
Number of patients (n) |
Percentage (%) |
|
Vagina delivery |
14 |
28 |
|
Assisted vaginal delivery |
2 |
4 |
|
Caesarean section (C/S) |
34 |
68 |
|
Elective |
20 |
40 |
|
Emergency |
14 |
36 |
Table-4: Mode of delivery among the study patients (N=50)
Analyzing the indications of caesarean section (C/S) revealed that, maximum (52.94%) had fetal distress followed by 35.29% had history of previous caesarean section and 11.76% had fetal mal-presentation (Table-5).
|
Indications of caesarean section (C/S) |
Number of patients (n) |
Percentage (%) |
|
Fetal distress |
18 |
52.94 |
|
History of previous C/S |
12 |
35.29 |
|
Mal-presentation |
4 |
11.76 |
Table-5: Indication of caesarean section (n= 34)
Table-6 showing the mode of deliveries took place according to the gestational age; 10%, 8% and 2% normal vaginal delivery (NVD) occurred in the gestational age group between 34-36 completed weeks, 37-39 gestational weeks and >40 gestational weeks respectively. Although in all gestational age groups caesarean section (C/S) rate was higher (Table-6).
|
Gestational age at the time of delivery |
Mode of delivery |
Total |
||||
|
NVD |
C/S |
|||||
|
No |
% |
No |
% |
No |
% |
|
|
34-36 completed weeks |
5 |
10 |
20 |
40 |
25 |
50 |
|
37-39 completed weeks |
4 |
8 |
16 |
32 |
20 |
40 |
|
>40 weeks |
1 |
2 |
4 |
8 |
5 |
10 |
Table-6: Gestational age at the time of delivery with mode of delivery (N= 50)
In this study; there were 16% babies had very low birth weight (VLBW: birth weight less than 1.5 kg) and 10% had low birth weight (LBW: birth weight between 1.5 kg to 2.5 kg) baby, but 4% was still born in the gestational age group 34-36 completed weeks. In the group of 37-39 completed weeks there were 40% healthy babies and 20% LBW babies; but 2% was still born. While in the group of >40 weeks gestational age; there were no LBW, VLBW or still born and 8% was healthy babies (Table-7).
|
Gestational age at the time of delivery |
Fetal outcomes |
|||||||
|
Healthy |
LBW |
VLBW |
Still born |
|||||
|
No |
% |
No |
% |
No |
% |
No |
% |
|
|
34-36 completed weeks |
- |
5 |
10 |
8 |
16 |
2 |
4 |
|
|
37-39 completed weeks |
20 |
40 |
10 |
20 |
- |
- |
1 |
2 |
|
>40 weeks |
4 |
8 |
- |
- |
- |
- |
- |
- |
Table-7: Distribution of fetal outcomes along with gestational age (N= 50)
Among the study women, color of the liquor at the time of delivery showed; 68% was normal color, 24% was meconium-stained liquor and 8% was thick meconium (Table-8).
|
Color of liquor |
Number of patients (n) |
Percentage (%) |
|
Normal color liquor |
34 |
68 |
|
Meconium-stained liquor |
12 |
24 |
|
Thick meconium |
4 |
8 |
Table-8: Color of the liquor at the time of delivery (N= 50)
In this study among 47 alive new born babies, 31.91%% new born baby had low birth weight (LBW: birth weight between 1.5 kg to 2.5 kg), 51.06%% baby had normal birth weight (birth weight >2.5 kg) and 17.02% had very low birth weight (VLBW: birth weight <1.5 kg.) (Table-9). Of them; 48.94% fetus had APGAR score ≤5 and 51.06% fetus had APGAR score >5 at one minute. On the other hand, 51.06% fetus had APGAR score >7 and 48.94% fetus had ≤7 APGAR score at five minutes (Table-9).
|
Variables |
Number of patients (n) |
Percentage (%) |
|
Birth weight (kg) |
||
|
<1.5 kg |
8 |
17.02 |
|
1.5 kg to 2.5 kg |
15 |
31.91 |
|
>2.5 kg |
24 |
51.06 |
|
APGAR score |
||
|
APGAR score at 1 minute |
||
|
≤5 |
23 |
48.94% |
|
>5 |
24 |
51.06% |
|
APGAR score at 5 minutes |
||
|
>7 |
24 |
51.06% |
|
≤7 |
23 |
48.94% |
Table-9: Fetal birth weight (kg) and APGAR score among the new born babies in this study (n= 47)
In this study out of 50 deliveries 3 (6%) were still born and 23 (46%) fetuses suffered from neonatal complications. Among them 5 (10%) fetuses had early neonatal death and rest 18 (36%) fetuses suffered from morbidities like- birth asphyxia (12%), neonatal sepsis (14%), neonatal jaundice (6%) and meconium aspiration syndrome (2%) (Table-10). It was observed that the babies with congenital defects died soon after delivery or were still born and those babies who got admitted in neonatal ward had early neonatal death due to severe septicemia.
|
Fetal outcomes |
Number of patients (n) |
Percentage (%) |
|
Morbidity |
18 |
36% |
|
Birth asphyxia |
8 |
16% |
|
Neonatal sepsis |
6 |
12% |
|
Neonatal jaundice |
3 |
6% |
|
Meconium aspiration syndrome |
1 |
2% |
|
Mortality |
8 |
16% |
|
Early neonatal death |
5 |
10 |
|
Still born |
3 |
6 |
Table-10: Distribution of fetal outcomes (n= 50)
4. Discussion
Oligohydramnios is a condition of decreased amniotic fluid volume relative to gestational age. Amniotic fluid (AF), which is a part of baby’s life support system, is produced soon after the amniotic sac is formed at approximately 12 days after conception [2]. The amniotic fluid index (AFI) ≤5 (or less than the 5th percentile) or the absence of pocket measuring at least 2 × 1 cm is defined as oligohydramnios [7,16,19]. Estimating of AFI by ultrasonogram can predict the risk of fetus [11]. Oligohydramnios is a common complication of pregnancy and its incidence is up to 5% of all pregnancies [20]. This current study aimed to assess the maternal and neonatal outcomes of pregnancy associated with oligohydramnios.
A total of fifty (50) pregnant women with oligohydramnios were enrolled in this study. The mean age of the study patients was 27.62±3.66 years. This mean age of women with oligohydramnios was matched with related previous studies [1,7,21-22]. In this study multiparous was more common than that of primiparous (56% versus 44%). This finding was consistent with similar previous studies [10,12,23]. However, few previous studies observed that maximum number of patients with oligohydramnios were primigravida [21, 24]. This variation could be due to different sample sizes. Current study found 60% study patients were 34-36 weeks gestational age followed by 32% was 37-39 weeks and 8% was 40-42 weeks gestational age. This finding was supported by a couple of previous study [25-26]. In this current study, 32% study patients exhibited borderline oligohydramnios, and 68% study patients experienced severe oligohydramnios. This result was comparable with a couple of related previous studies [27-29]. In a related study on amniotic fluid index, 32% had border line oligohydramnios and 68% had severe oligohydramnios, which was similar to this current study [28].
In this study the possible relationship among the causes of oligohydramnios showed that premature rupture of membrane (PROM) was associated with 28% study patients, followed by relationship with placental insufficiency, intra-uterine growth retardation (IUGR), congenital anomalies and postdated pregnancies were 18%, 14%, 10% and 8% respectively. This information provides valuable insights into the diverse etiological factors associated with oligohydramnios in the studied population. Chamberlain et al., showed a direct relationship between assessed amniotic fluid volume and IUGR [28]. Another study reflects that majority of congenital anomalies associated with oligohydramnios involves the urinary tract anomalies [30]. The prevalence of congenital anomalies and aneuploidy varies between 4.5%-37% and 0%-4.4% respectively [29-31].
In this study caesarean section rate was higher among women with oligohydramnios. In this context, Chauhan et al., found that AFI ≤5 cm was associated with an increase incidence of fetal distress indicated for caesarean section [12]. But Magnn et al., found 15.2% caesarean section deliveries among 341 oligohydramnios [23]. In another study, Volxman et al., also found an increase rate of caesarean section for fetal distress among oligohydramnios patients [32]. It was reported that, caesarean section rate was high in oligohydramnios group [23-24,26,32]. This high rate of caesarean section among patients with oligohydramnios may due to our limited facilities (instrumental) for partum and intrapartum fetal monitoring. In our study, major indications of caesarean section were, fetal distress followed by previous caesarean section and fetal mal-presentation. This result was an agreement of similar previous studies [12,32]. In this current study; only 20% normal vaginal delivery (NVD) occurred in the different gestational age groups (34-36 weeks, 37-39 weeks and >40 weeks) due to PROM or congenital anomalies. However, in all gestational age groups caesarean section (C/S) rate was higher mostly due to fetal distress. Among the study population in the gestational age group 34-36 completed weeks; 16% babies had very low birth weight (VLBW) and 10% babies had low birth weight (LBW), but only 4% was still born. In the gestational age group 37-39 weeks; there were 40% healthy babies, 20% LBW babies and only 2% was still born. In the gestational age group >40 weeks; there were no LBW, VLBW or still born and 8% was healthy babies.
In this study among 50 patients only 16 patients had meconium-stained liquor which was 32%. In a previous study among 147 oligohydramnios patients: meconium-stained liquor was found only in 9 patients which was 6% [10] It was documented that meconium-stained liquor less often complicated the pregnancy with oligohydramnios [10]. It was also reported that, no obvious relation between meconium-stained liquor and oligohydramnios [23].
In this study a high rate of low birth weight (LBW) babies (birth weight 1.5 kg to 2.5 kg was 56%) were observed. So, the current study though reflects the relation between oligohydramnios and low birth weights. This observation was consistent with related previous studies [7,33-34]. In contrast, one previous study among 79 oligohydramnios patients showed that, low birth weight babies were only 10% [23]. Another study made observations over 147 oligohydramnios patients and found 41(35%) babies with low birth weight [10]. In our study; almost half (48.94%) fetus had APGAR score ≤5 and 51.06% fetus had APGAR score >5 at one minute. On the other hand, 51.06% fetus had APGAR score >7 and 48.94% fetus had ≤7 APGAR score at five minutes. These findings were in a line of related previous studies [16, 32-33, 35]. In this context Shankar et al., reported that there is an association of severe oligohydramnios with APGAR score <7 [8].
In this current study out of 50 deliveries; 23 (46%) fetuses suffered from neonatal complications. Among them 36% fetuses suffered from morbidities like- birth asphyxia, neonatal sepsis, neonatal jaundice and meconium aspiration syndrome. These findings were reflected in related previous studies [29-33]. Regarding mortality, there were 5(10%) early neonatal death and 3(6%) still born. These still born were due to preterm babies with congenital defects in severe oligohydramnios. Early neonatal deaths were mainly due to septicemia in low-birth-weight babies. Chamberlain et al., showed that perinatal mortality is directly not only to gestational age at preterm but also with severity of the oligohydramnios [28]. Another study on 17 patients with oligohydramnios showed perinatal fetal mortality rate was 6% [36]. De Carolis et al., also showed perinatal mortality within the first week of life was 23% in pregnancies associated with oligohydramnios [37]. In accordance, Ogunyemi D and Thompson reported perinatal mortality was 18% among women having oligohydramnios [38]. Therefore, the fetal mortality of this current study was supported by related previous studies [34-38].
Conclusion
The current study concluded that, oligohydramnios is more common among multiparous than primiparous. The most of the cases of oligohydramnios are associated with premature rupture of membrane, placental insufficiency, intra-uterine growth retardation congenital anomalies of the fetus and postdated pregnancy. The rate of caesarean delivery is high among women with oligohydramnios. The indication of caesarean section is mainly due to fetal distress. Low birth weight babies and APGAR score below 7 babies are frequent in women with oligohydramnios. The birth asphyxia and neonatal sepsis are common neonatal morbidity in babies of women with oligohydramnios.
Limitations of the study
It was a single center study with a relatively small sample size.
Recommendation
A multicenter study with a larger number of samples should be done to confirm the result of this current study. Outcome measures could be compared between pregnant women of normal amniotic fluid volume with those of oligohydramnios. Follow up of neonates for a longer period should be done to assess the outcomes specially those who developed complication.
Conflicts of interest
The authors declared no conflict of interest regarding this publication.
References
- Butt FT, Ahmed B. The role of antepartum transabdominal amnioinfusion in the management of oligohydramnios in pregnancy. The Journal of Maternal-Fetal & Neonatal Medicine 24 (2011): 453-457.
- Ahmar R, Parween S, Kumari S, et al. Neonatal and maternal outcome in oligohydramnios: a prospective study. Int J Contemp Pediatr 5 (2018): 1409-1413.
- Ross MG, Beloosesky R, Queenan JT. Polyhydramnios and Oligohydramnios. Management of High-Risk Pregnancy: An Evidence-Based Approach 14 (2007): 316-325.
- Ulkumen BA, Pala HG, Baytur YB, et al. Outcomes and management strategies in pregnancies with early onset oligohydramnios. Clin Exp Obstet Gynecol 42 (2015): 355-357.
- Edmonds DK, editor. Dewhurst's textbook of obstetrics & gynaecology. Blackwell Pub.; 2007 Sep 20. ISBN-978-1-4051-6I 11-4.
- Baron C, Morgan MA, Garite TJ. The impact of amniotic fluid volume assessed intrapartum on perinatal outcome. American journal of obstetrics and gynecology 173 (1995): 167-174.
- Ibrahim HA, Zween ZM. Oligohydramnios and fetal outcome in term pregnancy. Zanco Journal of Medical Sciences (Zanco J Med Sci) 24 (2020): 347-353.
- Shenker L, Reed KL, Anderson CF, et al. Significance of oligohydramnios complicating pregnancy. American journal of obstetrics and gynecology 164 (1991): 1597-1600.
- Ross MG, Beloosesky R, Queenan JT. Polyhydramnios and Oligohydramnios. Management of High-Risk Pregnancy: An Evidence-Based Approach 14 (2007): 316-325.
- Casey BM, McIntire DD, Bloom SL, et al. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks’ gestation. American journal of obstetrics and gynecology 182 (2000): 909-912.
- Phelan JP, Smith CV, Broussard P, et al. Amniotic fluid volume assessment with the four-quadrant technique at 36-42 weeks' gestation. The Journal of reproductive medicine 32 (1987): 540-552.
- Chauhan SP, Sanderson M, Hendrix NW, et al. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a meta-analysis. American journal of obstetrics and gynecology 181 (1999): 1473-1478.
- Manning FA, Hill CM, Platt LD. Qualitative amniotic fluid volume determination by ultrasound: antepartum detection of intrauterine growth retardation. American journal of obstetrics and gynecology 139 (1981): 254-258.
- Sarno Jr AP, Ahn MO, Brar HS, et al. Intrapartum Doppler velocimetry, amniotic fluid volume, and fetal heart rate as predictors of subsequent fetal distress: I. An initial report. American journal of obstetrics and gynecology 161 (1989): 1508-1514.
- Seeds AE. Current concepts of amniotic fluid dynamics. American Journal of Obstetrics and Gynecology 138 (1980): 575-586.
- Locatelli A, Zagarella A, Toso L, et al. Serial assessment of amniotic fluid index in uncomplicated term pregnancies: prognostic value of amniotic fluid reduction. The Journal of Maternal-Fetal & Neonatal Medicine 15 (2004): 233-236.
- Catlin EA, Carpenter MW, Brann IV BS, et al. The Apgar score revisited: influence of gestational age. The Journal of pediatrics 109 (1986): 865-868.
- Hegyi T, Carbone T, Anwar M, et al. The Apgar score and its components in the preterm infant. Pediatrics 101 (1998): 77-81.
- Kehl S. Single deepest vertical pocket or amniotic fluid index as evaluation test for predicting adverse pregnancy outcome (SAFE trial): a multicenter, open-label, randomized controlled trial. Zeitschrift fur Geburtshilfe und Neonatologie 222 (2018): 28-30.
- Moore TR. Clinical assessment of amniotic fluid. Clinical obstetrics and gynecology 40 (1997): 303-313.
- Ahmar R, Parween S, Kumari S, Kumar M. Neonatal and maternal outcome in oligohydramnios: a prospective study. Int J Contemp Pediatr 5 (2018): 1409-1413.
- Tajinder K, Ruchika S. Feto-Maternal Outcome in Pregnancies with Abnorma l AFI. IOSR Journal of Dental and Medical Sciences 15 (2016): 71-75.
- Magann EF, Kinsella MJ, Chauhan SP, et al. Does an amniotic fluid index of≤ 5 cm necessitate delivery in high-risk pregnancies? A case-control study. American journal of obstetrics and gynecology 180 (1999): 1354-1359.
- Jagatia Krishna, Singh Nisha, Patel Sachin. Maternal and fetal outcome in oligohydramnios- Study of 100 cases. International Journal of Medical Science and Public Health 2 (2013): 724-727.
- Casey BM, McIntire DD, Bloom SL, et al. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks’ gestation. American journal of obstetrics and gynecology 182 (2000): 909-912.
- Jandial C, Gupta S, Sharma S, et al. Perinatal outcome after antepartum diagnosis of oligohydramnios at or beyond 34 weeks of gestation. JK Sci 9 (2007): 213-214.
- Yazsi A. The relation of intrapartum amniotic fluid index to perinatal outcomes. Kafkas J Med Sci 1 (2011): 1-7.
- Chamberlain PF, Manning FA, Morrison I, et al. Ultrasound evaluation of amniotic fluid volume: I. The relationship of marginal and decreased amniotic fluid volumes to perinatal outcome. American journal of obstetrics and gynecology 150 (1984): 245-249.
- Shipp TD, Bromley B, Pauker S, et al. Outcome of singleton pregnancies with severe oligohydramnios in the second and third trimesters. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology 7 (1996): 108-113.
- Meizner IS, Glezerman MA. Cordocentesis in the evaluation of the growth-retarded fetus. Clinical obstetrics and gynecology 35 (1992):126-137.
- Hill LM, Breckle R, Wolfgram KR, et al. Oligohydramnios: ultrasonically detected incidence and subsequent fetal outcome. American journal of obstetrics and gynecology 147 (1983): 407-410.
- Voxman EG, Tran S, Wing DA. Low amniotic fluid index as a predictor of adverse perinatal outcome. Journal of perinatology 22 (2002): 282-285.
- Patil SV, Shaikmohammed FZ. Study of Oligohydramnios and its perinatal outcome. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 8 (2019): 2705-2709.
- Figueroa L, McClure EM, Swanson J, et al. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries. Reproductive Health 17 (2020): 1-7.
- Kreiser D, el-Sayed YY, Sorem KA, et al. Decreased amniotic fluid index in low-risk pregnancy. The Journal of reproductive medicine 46 (2001): 743-746.
- Tranquilli AL, Giannubilo SR, Bezzeccheri V, et al. Transabdominal amnioinfusion in preterm premature rupture of membranes: a randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology 112 (2005): 759-763.
- De Carolis MP, Romagnoli C, De Santis M, et al. Is there significant improvement in neonatal outcome after treating pPROM mothers with amnio-infusion?. Neonatology 86 (2004): 222-229.
- Ogunyemi D, Thompson W. A case controlled study of serial transabdominal amnioinfusions in the management of second trimester oligohydramnios due to premature rupture of membranes. European Journal of Obstetrics & Gynecology and Reproductive Biology 102 (2002): 167-172.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 