Pheochromocytoma in Pregnancy: Looking Beyond Preeclampsia and Gestational Physiological Changes
Huyam Ghazi Ahmed Mahmoud1, Amira Abdellatif Hassan1*, Sakeriya Farah1, Ziena Abdullah1, Awad Elkarim1
1Princess Alexandra Hospital, UK
*Corresponding Author: Amira Abdellatif Hassan, Princess Alexandra Hospital, UK.
Received: 28 November 2023; Accepted: 07 December 2023; Published: 07 December 2023
Article Information
Citation: Huyam Ghazi Ahmed Mahmoud, Amira Abdellatif Hassan, Sakeriya Farah, Ziena Abdullah, Awad Elkarim. Pheochromocytoma in Pregnancy: Looking Beyond Preeclampsia and Gestational Physiological Changes. Obstetrics and Gynecology Research. 6 (2023): 295-298
View / Download Pdf Share at FacebookAbstract
Pheochromocytoma is a rare neuroendocrine tumor that arises from the adrenal medulla, resulting in the excessive release of catecholamines such as adrenaline and noradrenaline. This case report describes a 34-year-old woman who experienced severe hypertension and other symptoms three months after giving birth. Despite her physical examination appearing normal, further tests revealed a large adrenal mass. The diagnosis of pheochromocytoma, a type of neuroendocrine tumor, was confirmed. The patient's blood pressure was stabilized, and she underwent surgery to remove the tumor. This case highlights the importance of considering rare secondary causes of hypertension, especially in peripartum patients with a history of gestational diabetes and uncontrolled blood pressure. Early diagnosis and appropriate management are crucial in addressing these underlying conditions and relieving hypertensive symptoms.
Keywords
<p>Hypertension; Pheochromocytoma; Suprarenal mass; Catecholamine</p>
Article Details
Introduction
Pheochromocytoma is a catecholamine-secreting tumor originating from chromaffin cells of medullary region of adrenal gland or sympathetic ganglia. Pheochromocytomas accounts for 0.2 to 0.4% of hypertensive disorders and it may lead to severe or lethal hypertensive crisis [1,2]. Its prevalence during pregnancy is approximately 0.0002% [3,4]. Timely diagnosis of this disease and its proper management can lessen maternal and fetal mortality and morbidity from around 50% to less than 5% and 15%, respectively [5-10]. During pregnancy pheochromocytoma might not have any specific signs and symptoms. It is less prevalent than other hypertensive disorders during pregnancy. Also, specific symptoms such as paroxysmal attacks of sweating, palpitation, and blood pressure crisis are probably lower among pregnant women compared to non-pregnant woman [8]. A literature review shows that 90% of pregnant women demonstrate symptoms of pheochromocytomas right before delivery [8]. Thus, this may result in delayed diagnosis, putting the mother and child at risk.
Case presentation:
We present the case of a 34-year-old woman who had two prior pregnancies, the first of which was an uncomplicated vaginal delivery at 42 weeks, while the second pregnancy necessitated an emergency caesarean section at 37 weeks + 6 days due to uncontrolled preeclampsia, for which she received intravenous magnesium sulphate. Additionally, she had been diagnosed with gestational diabetes mellitus (GDM) at the 20th week of gestation, which required insulin administration for management. Post-delivery, she was discharged on a regimen of labetalol 100 mg twice daily for hypertension.
Approximately three months after delivery, the patient began experiencing troublesome symptoms. These included postural headaches with no palpitations or sweating, episodes where she felt as though she might faint, and hypotensive episodes. Her condition became particularly concerning when she presented to the emergency department with a severe frontal and occipital headache, accompanied by an alarmingly high systolic blood pressure of 212 mmHg.
Apart from a distressed and flushed appearance, her physical examination was largely unremarkable. Fundoscopy was normal with no papilledema. Her laboratory results as shown in table 1. A chest X-ray and brain computed tomography revealed normal results. The patient was admitted and received intravenous Labetalol and continued Labetalol tablets which controlled her Blood pressure. To explore potential secondary causes of hypertension, a series of blood tests and imaging were conducted. Transabdominal ultrasound imaging revealed an 8 x 4.5 cm right adrenal mass that appeared heterogeneous with some punctate hyperechogenic foci. A subsequent MRI of the adrenals confirmed this finding, characterizing the mass as an 8 x 7 x 5 cm well-defined right supra-renal mass, causing indentation and displacement of the right kidney, with no signs of liver infiltration. Notably, the left adrenal gland displayed normal appearances (Image 1).
The 24-hour urinary catecholamines and metanephrines displayed substantially raised Nor metadrenaline levels, which were 23umol/24hr and repeated 32umol/24hr (0.00-3.30) hence strongly suggestive of a neuroendocrine tumour. Finally, the diagnosis of pheochromocytoma was confirmed. Subsequently the patient had been followed up in the endocrinology clinic. After stabilizing her blood pressure, the labetalol treatment was discontinued, and she commenced treatment with Phenoxybenzamine 10 mg twice daily to manage her hypertension. Surgical intervention was deemed necessary to remove the neuroendocrine tumor, emphasizing the critical role of prompt diagnosis and appropriate management in addressing the underlying condition and alleviating her hypertensive symptoms (Image 2). This case underscores the importance of considering rare secondary causes of hypertension, particularly in peripartum patients with a history of gestational diabetes mellitus and uncontrolled blood pressure.
|
Full Blood Count |
Renal Profile |
LFTs |
|
Hb 180 (↑) |
Na 140 |
Alb 57 |
|
WBC 7.6 |
K 5.4 |
Bili 9 |
|
Plt 520 (↑) |
Urea 6.2 |
ALP 139 (↑) |
|
MCV 81 |
Creatinine 93 |
ALT 41 (↑) |
|
PCV 0.541 (↑) |
eGFR 60 |
|
|
Neut 4.3 |
||
|
CRP <1 |
Table 1
Discussion:
Pheochromocytomas are characterized by a classical triad of symptoms, namely headaches, sweating, and palpitations. These symptoms typically manifest episodically and tend to worsen as the tumour increases in size. It's noteworthy that the majority of these tumours are benign and typically arise sporadically, but up to 35% of cases are associated with hereditary syndromes like multiple endocrine neoplasia type 2 (MEN), Neurofibromatosis Type 1, or Von Hippel-Lindau syndrome.
Pheochromocytomas are known to synthesize and release catecholamines, including adrenaline, noradrenaline, and occasionally dopamine. These catecholamines are subsequently metabolized into metanephrines and normetanephrines, which are inactive metabolites, by the enzyme catechol-O-methyltransferase.
In terms of diagnosis, suspicion should arise in any patient presenting with the classical triad or having characteristics such as resistant hypertension, an early onset of hypertension, a family history of the condition, or co-existing endocrine disorders like Cushing's syndrome, impaired glucose tolerance, or diabetes (Algorithm 1). Pheochromocytomas may also be incidentally discovered during imaging studies.
Managing pheochromocytomas during pregnancy involves a cautious approach, with the administration of phenoxybenzamine for a duration of 10-14 days. However, it's important to be aware that this medication crosses the placenta and may result in perinatal depression in the mother and transient hypotension in the neonate.
• The timing of surgery for pheochromocytomas is a subject of debate and depends on several factors, including gestational age, response to treatment, accessibility of the tumour, and the presence or absence of fetal distress. Notably, it's essential to exercise caution during anaesthesia administration, as it can trigger hypertensive crises. General anaesthesia is considered the safest option for the fetus, particularly during the second trimester of pregnancy
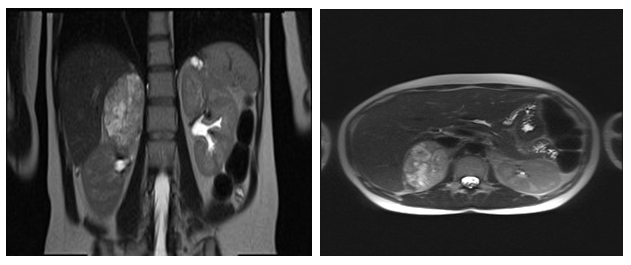
Image 1
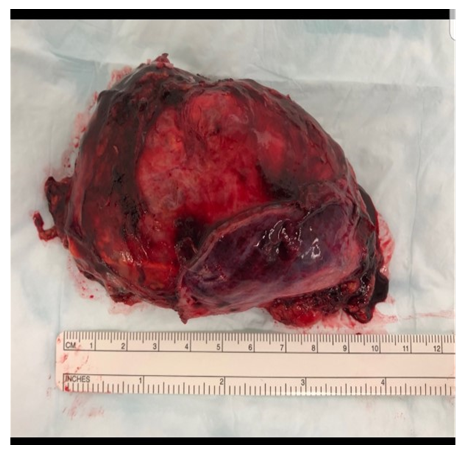
Image 2
Conclusion:
Diagnosing peripartum pheochromocytoma is challenging and extremely important, as it is rare and the clinical picture mimics that of preeclampsia, the most common form of hypertension occurring in pregnancy. It is crucial to diagnose pheochromocytoma during pregnancy to prevent fetal and maternal morbidity and mortality and to prevent precipitating life-threatening hypertensive crisis, as specific treatment is required in the management of both hypertension and delivery.
This case underscores the variability and complexity of medical conditions that can arise during pregnancy. While the patient's first pregnancy proceeded without significant issues, her second pregnancy was complicated by Emergency C-section for uncontrolled preeclampsia (PET) and was diagnosed with gestational diabetes mellitus (GDM) and delivered a full-term delivery.
The accurate diagnosis of her underlying medical condition only occurred in the postnatal period when her hypertensive symptoms worsened. It is widely acknowledged that postnatal care is often unvalued and underfunded. This case highlights the importance for ongoing medical surveillance and thorough evaluation, extending beyond the immediate perinatal phase, to uncover and address underlying medical conditions that might otherwise remain undetected. Timely diagnosis and intervention are paramount for the well-being of both the mother and the new-born, highlighting the significance of comprehensive postnatal care.
Although rare, pheochromocytoma can cause severe peripartum hypertension. Screening for pheochromocytoma, ideally with plasma-free metanephrines, should be considered in cases of medication resistant peripartum hypertension [9].

Algorithm 1
Learning points:
· While preeclampsia constitutes the commonest cause of hypertension in pregnancy, a broader approach remains crucial to avoid overlooking secondary causes such as pheochromocytoma
· It is imperative to consider investigating secondary causes of hypertension in pregnancy, particularly among those with inadequate or refractory response to conventional standard treatment.
· The prompt recognition and effective management of pheochromocytoma during pregnancy are crucial for preserving the well-being of both the mother and the foetus and to ameliorate the risk of life-threatening hypertensive crisis.
References
- Anagnostis P, Karagiannis A, Tziomalos K, et l. Endocrine hypertension: diagnosis and management of a complex clinical entity. Curr Vasc Pharmacol 8 (2010): 646–660.
- Karagiannis A, Mikhailidis DP, Athyros VG, et al. Pheochromocytoma: an update on genetics and management. Endocr Relat Cancer 14 (2007): 935–956.
- Harper MA, Murnaghan GA, Kennedy L, et al. Phaeochromocytoma in pregnancy. Five cases and a review of the literature. Br J Obstet Gynaecol 96 (1989): 594–606.
- Harrington JL, Farley DR, van Heerden JA, et al. Adrenal tumors and pregnancy. World J Surg 23 (1999): 182–186.
- Ahlawat SK, Jain S, Kumari S, et al. Phaeochromocytoma associated with pregnancy: case report and review of the literature. Obstet Gynecol Surv 54 (1999): 728-737.
- Schenker JG, Granat M. Phaeochromocytoma and pregnancy – an updated appraisal. Aust N Z J Obstet Gynaecol. 22 (1982): 1-10.
- Oishi S, Sato T. Phaeochromocytoma in pregnancy: a review of the Japanese literature. Endocr J 41 (1994): 219-225.
- Sarathi V, Lila AR, Bandgar TR, et al. Phaeochromocytoma and pregnancy: a rare but dangerous combination. Endocr Pract 16 (2010): 300-399
- Am J Hypertens. © 2005 American Journal of Hypertension, Ltd. 18 (2005): 1306-1312.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 