Sutureless Excision of Benign Bartholin’s Gland Cyst using Hydrodissection and Bipolar Forceps Haemostasis
Ramkrishna Purohit1*, Jay Gopal Sharma2, Devajani Meher2, Rupam Sarkar2
1Director, Department of Obstetrics and Gynaecology, Purohit General Hospital, Odisha, India
2Department of Obstetrics & Gynaecology, Purohit General Hospital, Odisha, India
*Corresponding Author: Dr. Ramkrishna Purohit, Director, Department of Obstetrics and Gynaecology, Purohit General Hospital, Shakti Nagar, Bargarh, pin-768028, Odisha, India
Received: 23 July 2021; Accepted: 02 August 2021; Published: 11 August 2021
Article Information
Citation:
Ramkrishna Purohit, Jay Gopal Sharma, Devajani Meher, Rupam Sarkar. Sutureless Excision of Benign Bartholin’s Gland Cyst using Hydrodissection and Bipolar Forceps Haemostasis. Obstetrics and Gynecology Research 4 (2021): 180-185.
View / Download Pdf Share at FacebookAbstract
Aim: To avoid recurrence and scarring following surgical treatment, the present study demonstrated a sutureless excision of the Bartholin’s gland cyst or abscess using hydro-dissection and bipolar coagulation hemostasis.
Materials and methods: In a retrospective case series, we studied consecutive cases who had received surgical treatment of the Bartholin’s gland cyst or abscess for benign indications in our private hospital.
Results: Of the total 28 cases, Seven cases received incision and drainage of the Bartholin’s abscess, 21 cases underwent excision of Bartholin’s cyst or abscess by the described procedure using hydro-dissection and bipolar coagulation haemostasis.No suture was used for layer closure of the wound. There were no major intraoperative complications. All cases experienced less postoperative pain. Spontaneous apposition of the vaginal wound margins was observed 24 hours after operation in all cases. None of the cases developed a postoperative hematoma, severe cellulitis, or abscess of the operation site requiring readmission. Postoperative-ly, five cases developed postoperative pyrexia, that sub-sided with broad-spectrum antibiotics. None of the cases developed severe postoperative scarring at the operation site following sutureless excision. None of the cases complained of difficulty in sexual function after 6 weeks. The median operation time was 17 min (13–23 min). None of the 21 cases reported recurrence of the cyst or abscess. All those seven cases who received incision and drainage of Bartholin’s abscess developed recurrence.
Conclusion: Sutureless excision of Bartholin’s gland cyst using hydro-dissection with bipolar coagulation hemostasis can be performed to avoid postoperative scarring and recurrence.
Keywords
Bartholin’s Cyst Recurrence, Scarring following Bartholin Cyst Excision, Hydro-dissection of Bartholin’s Cyst, Hemostasis during Bartholin Gland Excision
Bartholin’s Cyst Recurrence articles Bartholin’s Cyst Recurrence Research articles Bartholin’s Cyst Recurrence review articles Bartholin’s Cyst Recurrence PubMed articles Bartholin’s Cyst Recurrence PubMed Central articles Bartholin’s Cyst Recurrence 2023 articles Bartholin’s Cyst Recurrence 2024 articles Bartholin’s Cyst Recurrence Scopus articles Bartholin’s Cyst Recurrence impact factor journals Bartholin’s Cyst Recurrence Scopus journals Bartholin’s Cyst Recurrence PubMed journals Bartholin’s Cyst Recurrence medical journals Bartholin’s Cyst Recurrence free journals Bartholin’s Cyst Recurrence best journals Bartholin’s Cyst Recurrence top journals Bartholin’s Cyst Recurrence free medical journals Bartholin’s Cyst Recurrence famous journals Bartholin’s Cyst Recurrence Google Scholar indexed journals Scarring following Bartholin Cyst Excision articles Scarring following Bartholin Cyst Excision Research articles Scarring following Bartholin Cyst Excision review articles Scarring following Bartholin Cyst Excision PubMed articles Scarring following Bartholin Cyst Excision PubMed Central articles Scarring following Bartholin Cyst Excision 2023 articles Scarring following Bartholin Cyst Excision 2024 articles Scarring following Bartholin Cyst Excision Scopus articles Scarring following Bartholin Cyst Excision impact factor journals Scarring following Bartholin Cyst Excision Scopus journals Scarring following Bartholin Cyst Excision PubMed journals Scarring following Bartholin Cyst Excision medical journals Scarring following Bartholin Cyst Excision free journals Scarring following Bartholin Cyst Excision best journals Scarring following Bartholin Cyst Excision top journals Scarring following Bartholin Cyst Excision free medical journals Scarring following Bartholin Cyst Excision famous journals Scarring following Bartholin Cyst Excision Google Scholar indexed journals Hydro-dissection of Bartholin’s Cyst articles Hydro-dissection of Bartholin’s Cyst Research articles Hydro-dissection of Bartholin’s Cyst review articles Hydro-dissection of Bartholin’s Cyst PubMed articles Hydro-dissection of Bartholin’s Cyst PubMed Central articles Hydro-dissection of Bartholin’s Cyst 2023 articles Hydro-dissection of Bartholin’s Cyst 2024 articles Hydro-dissection of Bartholin’s Cyst Scopus articles Hydro-dissection of Bartholin’s Cyst impact factor journals Hydro-dissection of Bartholin’s Cyst Scopus journals Hydro-dissection of Bartholin’s Cyst PubMed journals Hydro-dissection of Bartholin’s Cyst medical journals Hydro-dissection of Bartholin’s Cyst free journals Hydro-dissection of Bartholin’s Cyst best journals Hydro-dissection of Bartholin’s Cyst top journals Hydro-dissection of Bartholin’s Cyst free medical journals Hydro-dissection of Bartholin’s Cyst famous journals Hydro-dissection of Bartholin’s Cyst Google Scholar indexed journals Hemostasis during Bartholin Gland Excision articles Hemostasis during Bartholin Gland Excision Research articles Hemostasis during Bartholin Gland Excision review articles Hemostasis during Bartholin Gland Excision PubMed articles Hemostasis during Bartholin Gland Excision PubMed Central articles Hemostasis during Bartholin Gland Excision 2023 articles Hemostasis during Bartholin Gland Excision 2024 articles Hemostasis during Bartholin Gland Excision Scopus articles Hemostasis during Bartholin Gland Excision impact factor journals Hemostasis during Bartholin Gland Excision Scopus journals Hemostasis during Bartholin Gland Excision PubMed journals Hemostasis during Bartholin Gland Excision medical journals Hemostasis during Bartholin Gland Excision free journals Hemostasis during Bartholin Gland Excision best journals Hemostasis during Bartholin Gland Excision top journals Hemostasis during Bartholin Gland Excision free medical journals Hemostasis during Bartholin Gland Excision famous journals Hemostasis during Bartholin Gland Excision Google Scholar indexed journals vulval pain articles vulval pain Research articles vulval pain review articles vulval pain PubMed articles vulval pain PubMed Central articles vulval pain 2023 articles vulval pain 2024 articles vulval pain Scopus articles vulval pain impact factor journals vulval pain Scopus journals vulval pain PubMed journals vulval pain medical journals vulval pain free journals vulval pain best journals vulval pain top journals vulval pain free medical journals vulval pain famous journals vulval pain Google Scholar indexed journals dyspareunia articles dyspareunia Research articles dyspareunia review articles dyspareunia PubMed articles dyspareunia PubMed Central articles dyspareunia 2023 articles dyspareunia 2024 articles dyspareunia Scopus articles dyspareunia impact factor journals dyspareunia Scopus journals dyspareunia PubMed journals dyspareunia medical journals dyspareunia free journals dyspareunia best journals dyspareunia top journals dyspareunia free medical journals dyspareunia famous journals dyspareunia Google Scholar indexed journals vaginal articles vaginal Research articles vaginal review articles vaginal PubMed articles vaginal PubMed Central articles vaginal 2023 articles vaginal 2024 articles vaginal Scopus articles vaginal impact factor journals vaginal Scopus journals vaginal PubMed journals vaginal medical journals vaginal free journals vaginal best journals vaginal top journals vaginal free medical journals vaginal famous journals vaginal Google Scholar indexed journals vaginal skin articles vaginal skin Research articles vaginal skin review articles vaginal skin PubMed articles vaginal skin PubMed Central articles vaginal skin 2023 articles vaginal skin 2024 articles vaginal skin Scopus articles vaginal skin impact factor journals vaginal skin Scopus journals vaginal skin PubMed journals vaginal skin medical journals vaginal skin free journals vaginal skin best journals vaginal skin top journals vaginal skin free medical journals vaginal skin famous journals vaginal skin Google Scholar indexed journals V- vaginal wall articles V- vaginal wall Research articles V- vaginal wall review articles V- vaginal wall PubMed articles V- vaginal wall PubMed Central articles V- vaginal wall 2023 articles V- vaginal wall 2024 articles V- vaginal wall Scopus articles V- vaginal wall impact factor journals V- vaginal wall Scopus journals V- vaginal wall PubMed journals V- vaginal wall medical journals V- vaginal wall free journals V- vaginal wall best journals V- vaginal wall top journals V- vaginal wall free medical journals V- vaginal wall famous journals V- vaginal wall Google Scholar indexed journals rectum articles rectum Research articles rectum review articles rectum PubMed articles rectum PubMed Central articles rectum 2023 articles rectum 2024 articles rectum Scopus articles rectum impact factor journals rectum Scopus journals rectum PubMed journals rectum medical journals rectum free journals rectum best journals rectum top journals rectum free medical journals rectum famous journals rectum Google Scholar indexed journals
Article Details
1. Introduction
Recurrenceof theBartholin’scystandscarringof the vaginal wallfollowingvariousconventional surgical proceduressuch asdrainageof anabscessor marsupia-lization, etc.causean unpleasant situation for thepatient and thecouple[1].Infectionof theBartholin’sgland cyst andformationof theabscesscausessevere vulval pain and dyspareunia.Theexcisionof theBartholin’s glandcyst orabscesswith layer closurecausesscarring of the vaginal wall andsubsequentdyspareunia. To avoid scarring of the vaginal wall andrecurrence followingthe surgical treatment [2, 3],we demonst-ratedthe below described operative procedure to excise theBartholin’s cystorabscess with thegland, and studieditsfeasibility.
2. Materials and Methods
In a retrospectivestudyin our private hospital from December 2017 through November 2020westudied consecutive caseswho hadundergonesurgical treatment of the Bartholin’s gland cyst orabscessfor benign indications. Weexcludedexcisionof other cysts of the vagina or vulva from thestudy. Each patient signed informed consent beforeoperation.Purohit general hospital ethics committee approved thestudy on dt. 2.6.20 (Referenceno-04/2020/PGHIEC).We wanted to know the feasibility of the excision of the Bartholin’s cyst or abscess by the following described procedure.
2.1 Procedure
Fourdropsof injection adrenaline(1:1000)weremixed with 40 ml of normal saline [4].Thesolutionwas infilt-rated subcutaneously into the loosetissuesaround the cyst orabscessto facilitate thedevelopmentof the tissue dissection plane and toreduce intraoperative bleeding.Medial to the hymen fold, a linear incision of 2.5–3.0 cm wasmadeby a surgical knife to incise the vaginal skin.The incision margins weregrasped andstretched byAlli’sforceps tomake asplit.The cleavage between the vaginal skin and the cyst wall was established by artery forceps orscissors using the open and close technique of dissection to expose the cyst wall.
The exposedcystwallwasgraspedby another Alli’s forcepsandpulled gentlyin the medially down-ward direction.Then,the tipof the index finger wasinsertedinto thecleavagebetween the vaginal margin and thecystwall (Figure 1),and thetensecyst was gradually dissected above downwards out of the loose subcutaneous andparavaginalfasciausingthe tactile feel.No sharpdissectionwasused. Vessels and tough cords of the tissue encountered on the way during the blunt dissection were coagulated using bipolar forceps coagulation(40-45 W)and separated from the cyst wall using scissors(Figure2)to cause bloodless enucleation.Medially downward traction of thecystand bluntdissection byfingergradually easedcomplete sca-ling of thecystwiththe glandout of the loose parava-ginalbedoftissues.The labial or vaginal skin was not excised at any stage of the operation.No mops wereused toclean blood duringdissection.Normal saline spray by a syringe of 20 ml with suction aspiration was used to keep the operation site clean.
In the case of an open cyst or an open abscess, normal saline lavage with suction aspiration was done to clear the contents.The tip of an artery forceps was used to grasp the cyst wall margin and pulled in the medially downward direction in a similar fashion as described before for the intact cyst.The tip of the surgeon’s left index finger was placed inside the lumen of the cyst or abscess (Figure3) to define the outer limit of the cyst wall and then, the blunt dissection procedures were carried out bythe right index finger in a similar aforementioned fashion for an intact cyst.
After removal of thecyst, incision margins were retracted byAlli’s forcepstoexposebleeder, if any inside thewoundbed and were cauterized using bipolarforcepscoagulation (40-45 W)toachieve complete hemostasis. Suturing of the wound cavity in layers or closure of the wound margins was not done.No gauze packing was used inside the wound to cause hemostasis, but a betadine lotion-soaked ribbon gauze pack was placed in the vagina(outside the wound)for approximately 4–6 h tokeepboth incision margins inpositionand tokeepthe woundcompressed. Postope-ratively, thepatientwas givenbroad-spectrum antibio-tics. She was examined vaginally by one finger 24 h after the operation to find hematoma if any and before sending her to the home.She was further advised to have sitz baths and the local application of betadine ointment for 2 weeks at home.They were followed up after 6weeksand 6months.

Figure 1: Shows Bartholin's cyst (C) dissection by index finger (F) from above downwards. V- vaginal wall.

Figure 2: Shows an intact Bartholin's cyst (C) following excision.
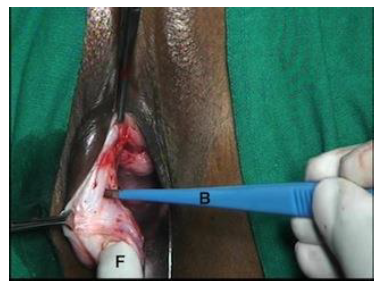
Figure 3: Shows the excision in a case of an open cyst using bipolar forceps haemostasis (B). F-Index finger tip inside an open cyst.
3. Results
Thetotalnumber ofcaseswas28. All patients were between 22 and 40 years of age, and were married.
Sevencasesof 28 hadundergoneincision and drain-ageof theBartholin’sabscessas an emergency measure toprovidereliefof severe vulvar pain. 21 cases of 28 underwent excision of Bartholin’s cyst or abscess owing to vulval swelling, pain, and dyspareunia.Of them, fourcaseshadahistoryof spontaneous rupture of theabscess within 24hoursbefore theoperation, and twocasesunderwentBartholin’sabscessexcisiondur-ing thepregnancy.
AllcasesunderwentunilateralBartholin’s cyst gland excisionby the described procedure.No other surgical proceduresuch asmarsupialization or Word catheter wasperformedin anycase.Therewasno major intra-operative complication.None of the caseshad severe intraoperativebleeding. Fivecasesdeveloped postop-erative pyrexia, whichsubsidedafter 48hoursof broad-spectrum antibiotic administration.Allcases experi-encedless postoperative pain.None of cases had burn ulcer of skin. Spontaneous apposition of the vaginal wound margins wasseen24hours afteroperationin allcases.None of the cases developeda postoperative hematoma, injury to the rectum, severe cellulitis, or abscess of operation site requiring readmission. None of the cases developed severe postoperative scarring at the operation site and subsequent dyspareunia.After 6 weeks following theoperation, no difference between the leftand the right vaginal wall was observed except a light scar mark on the site of the incision.
Histopathological study of the excised gland did not show malignancy in any of the cases.None of the cases complained of difficulty in sexual function subsequently after 6 weeks.The median operation timewas17min (13–23min).Hospital stay ranged from 1 to 2days. None of the 21 cases reported recurrence after excision of the cyst or abscess. Allthose sevencaseswho receivedincision anddrainageofBartholin’s abscess developedrecurrenceof the cyst orabscess.
4. Discussion
Infiltrationof the normal saline mixed solution with injection adrenaline(1:1000)around the Bartholin’s cystcausedtemporary hemostasis and helped to developa bloodless soft tissue dissection plane. Thehydrodissectionalsoassistedthe progress of blunt dissection byfingerusing tactile feel to enucleate through theskinsplitthe firm Bartholin’s gland mass(cyst orabscess)entirely from the loose para-vaginalfascia.Bipolar forceps coagulation hemostasis avoided the use of sutures to ligate bleeder if any, and thus, avoided the development of subsequent suture-induced scarring of the vaginal wall.
Incontrastto conventional surgical methods ofexcision, no layer closure wasneededin thisstudyas both incision margins fall on each other afterremovalof the space-occupyingsubcutaneouscyst. Non-recurrence of Bartholin’s cyst after the excision indicated complete excision by the present procedure. Methods of fistulization of Bartholin’s cyst such as marsu-pialization, Word catheter, and incision and drainage, though are simple have the disadvantages of frequent recurrence, scarring, dyspareunia, persistent drainage, and hemorrhage [1, 5, 8, 9].
Similar tofindingsby anotherstudy [6, 7],the present one-time initial surgicalexcisiontreatment of the Bartholin’s glandin eithercystor abscess stage can bedone.The excision avoided the botherations of recurrence in this study - finding similar to other studies [2, 3, 8,9]. Exci-sion usingbipolar hemostasis avoided layer closure by sutures and theformationof excessive scarring of the vaginal wall andsubsequent dyspareunia. Similar to theearlierstudy, theexcisionmethod did not hamper thesexualfunction ofwomenof thisstudy [9].
Contribution to Authorship
All authors qualified for authorship.
Disclosure of Interests
All authors have nothing disclosure of interest to declare.
Funding
No external funding was received for the study.
Acknowledgements
The authors would like to thank Vijay Babar for statistical assistance in the planning of the study.
References
- Reif P, Ulrich D, Bjelic-Radisic V. Management of Bartholin’s cyst and abscess using the Word catheter: implementation, recurrence rates and costs. Eur J Obstet Gynecol Reprod Biol 190 (2015): 81-84.
- Ozdegirmenci O, Kayikcioglu F, Haberal. Prospective randomized study of marsupialization versus silver nitrate application in the management of bartholin gland cysts and abscesses. J Minim Invasive Gynecol 16 (2009): 149-152.
- Wechter ME, Wu JM, Marzano D, et al. Management of Bartholin duct cysts and abscesses: a systematic review. Obstet Gynecol Surv 64 (2009): 395-404.
- Purohit RK. Purohit technique of vaginal hysterectomy a new approach. BJOG 110 (2003): 1115-1119.
- Gennis P, Li SF, Provataris J. Jacobi ring catheter treatment of Bartholin’s abscesses. Am J Emerg Med 23 (2005): 414-415.
- Kallam AK, Kanumury V, Bhimavarapu N. A report of two cases of ‘giant bartholin gland cysts’ successfully treated by excision with review of literature. J Clin Diagn Res 11 (2017): pd11-pd13.
- Lee MY, Dalpiaz A, Schwamb R. Clinical pathology of Bartholin’s glands: a review of the literature. Curr Urol 8 (2015): 22-25.
- Claire Cardaillac, Vincent Dochez, Pauline Gueudry, et al. Surgical management of Bartholin cysts and abscesses in French university hospitals. J Gynecol Obstet Hum Reprod 48 (2019): 631-635.
- Begum Aydogan Mathyk, Berna Aslan Cetin, Hale Cetin, et al. Sexual function after Bartholin gland abscess treatment: A randomized trial of the marsupialization and excision methods. Eur J Obstet Gynecol Reprod Biol 230 (2018): 188-191.


 Impact Factor: * 3.2
Impact Factor: * 3.2 Acceptance Rate: 76.63%
Acceptance Rate: 76.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 