A Study of Assessment of Neonatal Pain and the Practices in Pain Management amongst Health Care Workers in An NICU of A Tertiary Care Center
Manali Shinde1, Chhaya Valvi2, Isha Deshmukh3*, AA Kinikar4
1Resident in Pediatrics, BJGMC, Pune, India
2Professor, Pediatrics, BJGMC, Pune, India
3Assistant Professor, BJGMC, Pune, India
4Professor & HOD, BJGMC, Pune, India
*Corresponding Author: Isha Deshmukh, Assistant Professor, BJGMC, Pune, India
Received: 12 August 2022; Accepted: 03 October 2022; Published: 31 October 2022
Article Information
Citation: Manali Shinde, Chhaya Valvi, Isha Deshmukh, AA Kinikar. A Study of Assessment of Neonatal Pain and the Practices in Pain Management amongst Health Care Workers in An NICU of A Tertiary Care Center. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 495-501.
View / Download Pdf Share at FacebookAbstract
Background: Newborn infants experience acute pain during routine medical procedures. Evidence demonstrates that controlling pain in the newborn period can be beneficial, improving physiologic, hormonal and behavioral outcomes. Multiple validated scoring systems exist to assess pain in a neonate; however, there is no standardized or universal approach which can help in managing pain. Healthcare facilities should have a neonatal pain control program. The first step is to minimize the total number of iatrogenic events which can cause pain. If a procedure cannot be avoided, a graded approach to manage pain using non-pharmacological and pharmacological methods is recommended. Despite the recommendations and guidelines based on evidence, contemporary research shows that the problem of pain among patients in NICUs in various centers is still an important and neglected problem. Today we have adequate evidence that shows how repetitive painful procedures have short [1] and long term [2] adverse consequences for the developing neonatal brain. Despite this, adequate pain management is still not observed [3].
Aims and objectives: The aim of this study was to assess the level of knowledge of the medical personnel and their perception of the issue of pain in neonatal patients along with their awareness about evaluation and treatment of pain in a neonatal unit. Also, to assess awareness and use of pharmacological and non-pharmacological methods for pain management.
Methods: A descriptive, cross sectional study was carried out among NICU staff. The questions were inspired by questionnaire used in some studies. [4, 5] Primary data was collected using predesigned questionnaire with open ended questions using Google Forms was circulated using emails. The collected data was retrieved as an excel file. Statistical analysis was done on
Keywords
<p style="text-align:justify">Executive functions, Dietary fat intake, Perceived stress, prenatal distress, Emotion control</p>
Article Details
Introduction
Socio-demographic Characteristics
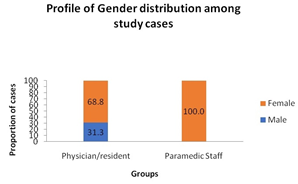
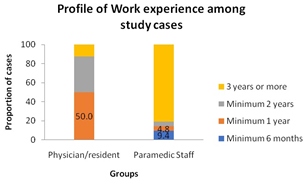
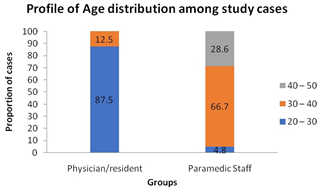
86.8 % of respondents were females, 100 % of paramedic staff and 68.8 % residents. The highest numbers of respondents were between 20-30 years age group in case of residents (87.5%) whereas in 30-40 years of age group in paramedic staff (66.7%). Majority of staff had professional experience for more than 3 years of working in the NICU. (81%) whereas majority residents had experience of at least 1 year (50 %) (Figures 1-3).
The detailed socio-demographic characteristics of the study group are presented in Tables 1-4.
|
Parameters |
Physician/resident (N =16 ) |
Paramedic Staff (N = 21) |
p value |
|
Age (Years) (%) 20 – 30 30 – 40 40 – 50 |
14 (87.5) 02 (12.5) -- |
01 (04.8) 14 (66.7) 06 (28.6) |
<0.001 |
|
Gender (%) Male Female |
05 (31.3) 11 (68.8) |
-- 21 (100.0) |
0.006 |
|
Work experience in NICU (%) Less than 6 months Less than 1 year Less than 2 years 3 years or more |
-- 08 (50.0) 06 (37.5) 02 (12.5) |
02 (09.4) 01 (04.8) 01 (04.8) 17 (81.0) |
<0.001 |
By Chi-square test, p = 0.016, p<0.05 Significant.
Table 1: Demographic Data of the study population
Correlation Analysis:
|
Age Groups |
Average total perception (N = 37) |
|
20 – 30 years |
18.80 ± 02.27 |
|
30 – 40 years |
18.56 ± 03.08 |
|
40 – 50 years |
18.67 ± 05.13 |
By Pearson Correlation Co-efficient, r = -0.024, p = 0.889, p>0.05 Not Significant
Table 2: Correlation of Age with Perception of Pain Management.
|
Gender |
Average total perception (N = 37) |
|
Male |
18.80 ± 03.77 |
|
Female |
18.66 ± 03.05 |
By Pearson Correlation Co-efficient, r = -0.016, p = 0.925, p>0.05 Not Significant.
Table 3: Correlation of Gender with perception of pain management.
|
Work experience |
Average total perception (N = 37) |
|
Minimum 6 months |
20.50 ± 00.71 |
|
Minimum 1 year |
18.44 ± 02.35 |
|
Minimum 2 years |
18.00 ± 03.27 |
|
3 years or more |
18.84 ± 03.55 |
By Pearson Correlation Co-efficient, r = -0.019, p = 0.913, p>0.05 Not Significant.
Table 4: Correlation of work experience with perception of pain management.
The p value was insignificant but if we take bigger sample size, we might find a significant value and results.
Assessment of Health care professional’s perceptions of neonatal pain
A detailed summary of 5 aspects of their perceptions of neonatal pain is presented in Table 5.
|
Questions |
Physician/ residents (N =16) |
Paramedical staff (N=21) |
|||
|
Yes |
No |
Yes |
No |
||
|
Knowledge and Beliefs about Neonatal Pain |
Neonates are capable of experiencing pain. |
15(93%) |
1(7%) |
16(76.2) |
5(23.8%) |
|
Pain in the neonatal period has long-term adverse effects. |
10(62.6%) |
6(37.4%) |
14(66.6) |
7(33.4%) |
|
|
Neonates, especially preterm infants are less sensitive to pain than older children and adults because of the immature nervous system. |
10(62.6%) |
6(37.4%) |
9(42.8%) |
12(57.2%) |
|
|
Minor procedures, such as orogastric tube placement and oral suctioning can cause pain. |
12(75%) |
4(25%) |
11(52.4%) |
10(47.6%) |
|
|
Preterm neonates are at a greater risk of neuro-developmental impairment due to repeated painful procedures in their NICU stay. |
12(75%) |
4(25%) |
16(76.2%) |
5(23.8%) |
|
|
Perceptions of Pain Assessment Tool in the Neonatal Intensive Care Unit |
We use a neonatal pain assessment scale/ tool in our NICU on daily basis. |
- |
16(100%) |
5(23.3%) |
16(76.7%) |
|
I feel confident with my skills in recognizing and assessing the signs of neonatal pain. |
- |
16(100%) |
12(57.1%) |
9(42.9%) |
|
|
I think we are managing neonatal pain according to protocols. |
3(18.8%) |
13(81.2) |
12(60%) |
8(40%) |
|
|
Use of Pharmacological and non pharmacological methods |
Non pharmacological pain management like cuddling and giving sucrose swabs is effective in managing pain. |
15(93.8%) |
1(6.2%) |
17(85%) |
3(15%) |
|
Pain management is not necessary because many invasive procedures can be done quickly. |
2(12.5%) |
14(87.5%) |
5(25%) |
21(75%) |
|
|
I feel confident with my skills in pain management using non-pharmacological interventions in neonates |
7(42.8%) |
9(57.2%) |
14(66.6%) |
7(33.4%) |
|
|
Oral sucrose is an effective way to approach to neonatal pain. |
12(75%) |
4(25%) |
12(57.2%) |
9(42.8%) |
|
|
Family/Culture Perspectives in Pain Management |
Parents are emotionally affected by the pain their infant may be experiencing. |
16(100.0%) |
- |
21(100%) |
- |
|
Parents should be involved in the care and comfort of their infant during painful procedures. |
11(68.8%) |
5(31.3%) |
9(42.9%) |
12(57.1%) |
|
|
Kangaroo mother care and breast feeding can help us as a non-pharmacological way to manage neonatal pain. |
16 (100%) |
- |
21(100%) |
- |
|
Table 5: Aspects of their perceptions of neonatal pain.
Knowledge and Beliefs about Neonatal Pain
A significant number of participants in the study group (N=31; 86 %,) realized that neonates are capable of experiencing pain, the majority of those (N=2; 66.6%) also believed that pain in the neonatal period will have long term side effects. The nearly half of the health care workers (N=19; 52.7%) thought that preterm infants are less sensitive to pain than older children and adults because of the immature nervous system. A significant number of responders thought minor procedures like OGT insertion and oral suctioning can cause pain. (N=23, 63.8%). Moreover, the respondents agreed with the statement that pain experienced in the neonatal period has long-term adverse effects like impaired neurodevelopment due to repeated painful procedures in their NICU stay. (N=28, 77.7%)
Use of Pain Assessment Tools/scales
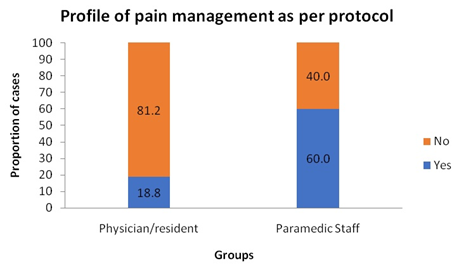
Majority of health care workers had not received any training while joining about neonatal pain assessment. Out of 37 workers, only 5 workers (13.8%) agreed that they use some scales and using protocols for neonatal pain assessment in daily practices but 15 (41.6%) % of all were confident about recognizing and assessing signs of neonatal pain out of which 3 (20%) were residents and 12 (80%) were paramedical staff. All 100 % residents and 76.7 % staffs agreed that they did not use the recommended tools for pain monitoring in this group of patients (Figure 4).
|
Parameters |
N = 36 |
|||
|
Physician/resident (N = 16) |
Paramedic staff (N = 20) |
|||
|
I think we are managing neonatal pain according to protocols. |
N |
% |
N |
% |
|
Yes |
03 |
18.8 |
12 |
60.0 |
|
No |
13 |
81.2 |
08 |
40.0 |
By Chi-square test, p = 0.013, p<0.05 Significant
Use of Pharmacological and Non-Pharmacological methods
The respondents agreed that pharmacological and non-pharmacological interventions are necessary and they can efficiently reduce the pain, despite the fact that many invasive procedures may be carried out quickly. (N=35, 94%). The analysis of their responses demonstrated that neonatal pain is indeed treated in most of the centers in the form of injectable Midazolam during painful procedures and paracetamol suppositories in post OP patients. Most of the respondents (64.86%) agreed that non pharmacological methods including oral sucrose swabs would definitely help in alleviate the pain and they were confident in using them. According to 32 health care workers (86.48%); non-pharmacological pain management like cuddling and giving sucrose swabs is effective in managing pain.
Family Involvement and Cultural Aspects
All 100 %participants agreed that parents are emotionally affected by the pain their infants face during painful procedures but 17 (45.94%) were of the opinion that parents shouldn’t be present and get involved in pain management during painful procedures considering emotional liability of mothers. On the contrary, all 100 % of the participating subjects agreed that kangaroo mother care and breast feedingis an efficient non-pharmacological method for neonatal pain relief after the painful procedure is completed.
Daily procedures and assessment of pain
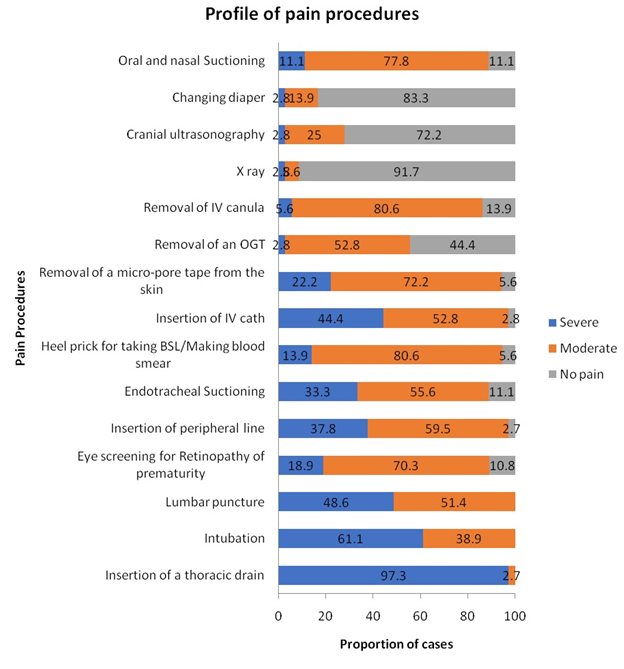
When health care workers were told to rate the pain a neonate might be experiencing during routine procedures they face, it was observed that the average neonate was experiencing severe pain on daily basis especially in high dependency unit. Insertion of an IV access was graded as severe pain by 44.4% of the health care workers whereas 80.6 % labelled heel pricks as moderately severe for blood sugar level monitoring. Acts which might seem less painful but carried out daily like removal of IV catheter (80.6 %), removal of a micropore from skin (72.2 %) weregraded as moderately severe procedures. Hence planning the sampling in advance and minimum frequency of these procedures to reduce the pain is advisable.
Results
Our study analyzed the level of knowledge of medical personnel and observations regarding prophylaxis of pain and therapy in tertiary care neonatal intensive care units. The results clearly showed that the majority of participants have a sufficient level of knowledge of pain. However, in most of the hospitals there are no proper assessment tools. This is definitely an area where we can improvise. It should be emphasized that long-term chronic pain or long-lasting repetitive nociceptive impulses in this population may result in cognitive, motor, behavioral and personality disturbances [6, 7, 8]. Out of 28 (75.67%) confronted that they hadn’t undergone any lecture based on the neonatal pain assessment since joining / in past 3 years.
The results of our study show that the training for newly employed nurses/midwives was insufficient and that no adequate postgraduate educational programs were available [9, 10]. The level of knowledge and the skills of respondents who use pain assessment scales in their routine practice are also unsatisfactory. Almost half of the studied subjects were not confident in the identification of pain indicators (Figure 5).
Discussion
Newborn infants experience pain just as older children and adolescents experience pain; however, clinicians’ ability and approach to assessing and managing neonates is inadequate and controversial. Newborn infants experience acute measurable physiologic, metabolic, and hormonal, behavioral responses to pain [11]. They also experience long-term effects, including negative effects on neurologic and behavioral development. This is because they face pain during a very crucial time period of neurologic maturation [12]. In fact, preterm infants have demonstrated an exaggerated acute response to pain and behavioral and sensory long-term outcomes were worse when compared to term neonates [13, 14]. Available evidences have demonstrated that controlling pain in the newborn period improves physiological, behavioral, and hormonal outcomes. [11, 12]… Additionally, there is a lack of understanding of how neonates perceive pain and the resulting adverse outcomes that occur when pain remains untreated [12]. Thus, it is the need of today’s neonatologist to have some standard guidelines. There is lack of a universal method to assess pain. Objective measurements including heart rate, blood pressure, and levels of salivary cortisol can be used, but most care providers usually rely on grimace, crying and facial expressions. Objectives methods are inconvenient in resource limited settings. There are multiple validated pain scales utilized by NICUs to assess pain. For example for term neonates: neonatal facial coding system (NFCS); the neonatal infant pain scale (NIPS); cry, required oxygen, increased vital signs, expression, sleeplessness scale (CRIES); neonatal pain, agitation, and sedation scale (N-PASS); COMFORT Scale; and Douleur Aigue Nouveau-ne (DAN) scoring system have all been described in the literature .The premature infant pain profile (PIPP) is a validated pain scoring system which is used for preterm neonates.
Non-pharmacologic therapies, which include oral sucrose or glucose, breast or bottle feeding, Kangaroo mother Care, non-nutritive sucking, swaddling or facilitated tucking. Of all non-pharmacologic therapies the use of oral sucrose is the most discussed method. The proposed hypothesis is that glucose (and its alternative forms, such as sucrose) are responsible for endogenous opioid release, through an unknown mechanism [15–17]. The use of sucrose in neonates, when compared to breast milk or pacifier use is also associated with a reduction in behavioral indicators of pain, such as crying and grimacing seen in painful procedures [18]. Breast feeding was also found to be useful in alleviating pain. Shah et al. demonstrated in a Cochrane review that breastfeeding can have an advantage for one-time painful procedures [19]. Careful positioning such as swaddling a neonate and facilitated tucking, which involves manually flexing a neonate’s arms and the legs have shown to be effective at reducing pain in neonates [20].
In pharmacological methods, EMLA which is a cream based formulation of lidocaine (2.5 %) and prilocaine (2.5 %) has been well established as effective in the neonatal population for reducing pain associated with minor procedures as a topical anesthetic agent. [21] Acetaminophen is one of the most commonly used systemic medications in the neonatal population due to its well-established effectiveness at pain reduction as well as its favorable side effect profile [21].
The optimization of pain management in the neonatal population is fundamentally aimed at reducing the total number of painful events. [22]. The clinicians reduce the number of painful events. The approach should include avoiding unnecessary painful procedures. Further, clinicians should reduce the number of bedside interruptions and daily examinations, if possible. Additionally, clinicians can anticipate the need for future studies and, with thoughtful planning, can coordinate studies to minimize the frequency pricks for withdrawing blood.
So, with help of this study it was proved that with a standardized approach to assess and manage pain, we hope to improve acute pain faced by the neonate, long-term neurologic and behavioral impairments, as well as parent and provider satisfaction. Ultimately, further research is needed regarding efficacy, safety profiles, and satisfaction scoring to better achieves these goals (Table 6).
Assessment of Training
|
Parameters |
N = 37 |
|||
|
Physician/resident (N = 16) |
Paramedic Staff (N = 21) |
|||
|
I have attended a lecture in past 3 years which has included information on neonatal pain assessment |
N |
% |
N |
% |
|
Yes |
07 |
43.8 |
02 |
09.5 |
|
No |
09 |
56.3 |
19 |
90.5 |
By Chi-square test, p = 0.016, p<0.05 Significant
Table 6: Profile of information on neonatal pain assessment.
Majority respondents wanted clinics every 3 monthly to update their knowledge and revise the scales to assess pain. So, it becomes very important to carry out adequate training on physiological and behavioral pain indicators in neonates considering these responses. The selection of an appropriate assessment tool depends on the clinical condition of the patient requiring intensive care. No single universal scale analyzing acute/procedure-related or chronic pain has been developed for this category of patients [9, 10]. Regardless of the type of measurement tool used, the percentage of personnel using it in routine clinical practice remains insufficient. This may result from inadequate training and a small number of staff responsible for carrying out such training [5]. Only 15.8% of respondents confirmed that the healthcare center where they are employed provided them a training session when they joined.
Conclusions
Our analyses indicate that health care workers obtained knowledge regarding neonatal pain by their own experience rather than proper training programs. According to the study subjects, pharmacological and non-pharmacological interventions undertaken in neonatal patients are effective in pain relief. The introduction of strategies to promote and extend the awareness among personnel of the neonatal pain monitoring scales is necessary. Implications of these practices with further studies concerning the control of neonatal pain evaluation, will allow the development of adequate training programs in this field. Unanimity in the pain scale will help by reducing chances of subjective assessment and will help in managing the pain without any discrepancy. Proper lectures creating awareness about assessment of pain, the long term effects on neonate in future and managing using adequate measures need to be scheduled every 3 monthly in our set up as rotation of residents and changing posting can be bothersome. We should try minimizing the procedures which can cause pain to a neonate by using proper techniques and planning. Pain, if managed adequately, can definitely help the baby to live a healthy and prosperous life in true senses.
References
- Grunau RE, Holsti L, Haley DW, Oberlander T, Weinberg J, et al. Neonatal procedural pain exposure predicts lower cortisol and behavioral reactivity in preterm infants in the NICU. Pain 113 (2005): 293-300.
- Hermann C, Hohmeister J, Demirakca S, Zohsel K, Flor H. Longterm alteration of pain sensitivity in school-aged children with early pain experiences. Pain 125 (2006): 278-285.
- Walker SM. Management of procedural pain in NICUs remains problematic. PaediatrAnaesth 15 (2005): 909-912.
- Bains, Sukhjeet Kumar, Praveen Sundaram, Venkataseshan Lang, Astri Saugstad Ola. A Comparison of Health Care Workers Assessment and Management of Pain between a Neonatal Intensive Care Unit in India and Norway. Journal of Palliative Care & Medicine (2016): 06. 10.4172/2165-7386.1000255.
- Popowicz H, Medrzycka-Dabrowska W, Kwiecien-Jagus K, Kamedulska A. Knowledge and Practices in Neonatal Pain Management of Nurses Employed in Hospitals with Different Levels of Referral-Multicenter Study. Healthcare (Basel). 9(2021): 48. Doi: 10.3390/healthcare9010048. PMID: 33466529; PMCID: PMC7824971.
- Valeri BO, Holsti L, Linhares MBM. Neonatal pain and developmental outcomes in children born preterm: A systematic review. Clin J Pain, 31 (2015): 355–362. [CrossRef]
- Brummelte S, Grunau RE, Chau V, Poskitt KJ, Brant R., Vinall J, Gover A, Synnes AR, Miller SP. Procedural pain and brain development in premature newborns. Ann. Neurol 71 (2012): 385–396. [CrossRef] [PubMed]
- Eckstein Grunau, R. Neonatal Pain in Very Preterm Infants: Long-Term Effects on Brain, Neurodevelopment and Pain Reactivity. Rambam Maimonides Med J 4 (2013). [CrossRef] [PubMed]
- Popowicz H, Olszewska J, M,edrzycka-Dabrowska W, Kwiecie ´n-Jagu´s K. Pain Scales in Neonates Receiving Mechanical Ventilation in Neonatal Intensive Care Units–Systematic Review. J. Pain Res (2020): 1883–1897. [CrossRef] [PubMed]
- Ranger M, Johnston CC, Anand KJ. Current controversies regarding pain Assessment in neonates. Semin. Perinatol. 31 (2007): 283–288. [CrossRef]
- Lago P, Garetti E, Merazzi D, et al. Guidelines for procedural pain in the newborn. Acta Pediatr (Oslo, Norway, 98(2009): 932-939. doi:10.1111/j.1651-2227.2009.01291.x. A fondational systematic review of procedural pain prevention and treatment of NICU neonatal patients.
- Anand KJ, Aranda JV, Berde CB, et al. Summary proceedings from the neonatal pain-control group. Pediatrics, 117(2006): S9–22.
- Frunau RVE. Long-term consequences of pain in human neonates. In: Anand JKS, Stevens BJ, McGrath PJ, editors. Pain in neonates. 3rd ed. Amsterdam: Elsevier; (2007): 55–76.
- Peterson BS, Vohr B, Staib LH, Cannistraci CJ, DOlberg A, Schenier KC, et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA, 284 (2000): 1939-1947.
- Blass E, Fitzgerald E, Kehoe P. Interactions between sucrose, pain and isolation distress. Pharmacol Biochem Behav, 26 (1987): 483-489.
- Blass EM, Shah A. Pain-reducing properties of sucrose in human newborns. Chem Sens, 20 (1995): 29-335.
- Ren K, Blass EM, Zhou QQ, Dubner R. Suckling and sucrose ingestion suppress persistent hyperalgesia and spinal FOS expression after forepaw inflammation in infant rats. Proc Natl Acad Sci USA, 94 (1997): 1471-1475.
- Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev (2010); 1:CD001069.
- Shah PS, Aliwalas LI, Shah V. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2006; 3:CD004950.
- Johnston C, Campbell-Yeo M, Fernandes A, Inglis D, Streiner D, Zee R. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst Rev. 2014
- Witt N, Coynor S, Edwards C, Bradshaw H. A Guide to Pain Assessment and Management in the Neonate. CurrEmerg Hosp Med Rep 4 (2016): 1-10. Doi: 10.1007/s40138-016-0089-y
- Sharek PJ, Powers R, Koehn A, Anand KJ. Evaluation and development of potentially better practices to improve pain management of neonates. Pediatrics, 118(2016): S78.


 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 