Effect of Maternity Waiting Home Service Utilization on Perinatal Health Outcomes in Public Hospitals of West Arsi Zone, Oromia Region: Institution Based Prospective Cohort Study
Negeso Gebeyehu Gejo1*, Abraham Endale Geleta2*, Maedot Ariaya Haymete3, Daniel Yohannes Bedecha1, Aman Urgessa Edaso1
1Department of Midwifery, Madda Walabu University, Shashamane Campus, Shashamane, Ethiopia
2Department of Public Health, Madda Walabu University, Shashamane Campus, Shashamane, Ethiopia
3Virginia Tech Carilion School of Medicine, Roanoke, VA, USA
*Corresponding Authors: Negeso Gebeyehu Gejo, Department of Midwifery, Madda Walabu University, Shashamane Campus, Shashamane, Southeast Ethiopia.
Abraham Endale Geleta, Department of Public Health, Madda Walabu University, Shashamane Campus, Shashamane, Southeast Ethiopia.
Received: 22 May 2025; Accepted: 29 May 2025; Published: 05 June 2025
Article Information
Citation: Negeso Gebeyehu Gejo, Abraham Endale Geleta, Maedot Ariaya Haymete, Daniel Yohannes Bedecha, Aman Urgessa Edaso. Effect of Maternity Waiting Home Service Utilization on Perinatal Health Outcomes in Public Hospitals of West Arsi Zone, Oromia Region: Institution Based Prospective Cohort Study. Journal of Pediatrics, Perinatology and Child Health. 9 (2025): 105-115.
View / Download Pdf Share at FacebookAbstract
Background: Maternity waiting homes (MWHs), also known as mother’s shelters, are structures built near healthcare facilities. The use of MWHs has been linked to reductions in maternal mortality. However, due to a lack of strong evidence in this area, conclusive evidence has not been able to be reached indicating definitively that MWHs lead to fewer perinatal deaths. Objective: The primary aim of this study was to assess the effect of maternity waiting home service utilization on perinatal health outcomes in public hospitals in West Arsi Zone, Oromia Region, from March 8 to June 1, 2022.
Methods: A prospective cohort study was conducted among 1606 mothers (803 maternity waiting home users and 803 non-users) who were admitted to public hospitals in the West Arsi Zone from March 8 to June 1, 2022. Simple random sampling methods were used to approach study participants. Epi-data version 3.1 and Stata version 16 were used for data entry and analysis, respectively. Both bivariable and multivariable generalized linear model analyses were done to identify associations between dependent and independent variables. Crude and adjusted relative risk with respective 95% confidence intervals were computed, and statistical significance was declared at p-value <0.05.
Result: There was a 39% reduced risk of developing perinatal complications in the exposed group when compared to the non-exposed group [RR = 0.61, 95% CL = 0.42, 0.88]. Multiparity [RR=1.42 95%Cl (1.17, 1.72), advanced maternal age [RR= 0.57 95%Cl (0.41, 0.97), and maternal complication [RR=1.59 95%Cl (1.34, 1.90)] were independent predictors for perinatal complications.
Conclusion and Recommendations: The present study found that maternity waiting home users had a reduced risk of developing perinatal complications when compared to non-users. Besides, advanced maternal age, multiparity, maternal complications, and transfer from another facility were independent predictors of perinatal complications. Strengthening maternity waiting home services is decisive to reducing perinatal complications.
Keywords
<p>Maternity Waiting Home, Perinatal Health Outcome, Public Hospitals, West Arsi Zone</p>
Article Details
Abbreviations:
ANC: Antenatal Care; APH: Antepartum Hemorrhage; C/S: Cesarean Section; EDHS: Ethiopian Demographic Health Survey; EPHI: Ethiopian Public Health Institute; MWHs: Maternity Waiting Homes; PNM: Perinatal Mortality; PROM: Premature Rupture of Membranes; PPH: Postpartum Hemorrhage; SDGs: Sustainable development Goals; WHO: World Health Organization; SVD: Spontaneous Vaginal Delivery
1. Introduction
Maternity waiting homes, also known as mother’s shelters, are structures built near healthcare facilities to minimize the critical barrier of distance to accessing maternal health services. They function as one possible medical intervention included in a range of services for the health of expectant mothers and newborns [1].
Among deaths that happened in children and young adolescents worldwide in 2018, 85% occurred in the first five years of life, constituting 5.3 million deaths, of which 2.5 million occurred in the first month of life [2]. In Ethiopia, the maternal mortality ratio is estimated at 412 per 100,000 live births, infant mortality at 48 deaths per 1,000 live births, the under-five mortality rate at 67 per 1000 live births, and neonatal mortality at 29 deaths per 1000 live births [3].
Of the six observational studies that assessed the impact of waiting houses for mothers on perinatal outcomes, four revealed improved outcomes among users compared with non-users. A Cochrane review of maternity waiting houses identified no randomized controlled trials [4]. The third Sustainable Development Goal (SDG) aims to halt preventable newborn and under-five child deaths as well as lower the global maternal mortality ratio to less than 70 per 100,000 live births [5].
So one strategy to lower newborn mortality is to increase institutional births; one way to do this is by creating and utilizing mother-and-child waiting homes [6]. The first maternity waiting homes were constructed in Ethiopia in 1976 [7], and as of right now, the Amhara area has the highest coverage (72%), followed by the Oromia region (56%), the Southern Nations, Nationalities, and Peoples' area (SNNPR) (57%), and the Gambella region (8%) [8].
The use of MWHs has been linked to reductions in perinatal mortality in Ethiopia, Ivory Coast, Liberia, and Zimbabwe [9]. However, due to a lack of strong evidence in this area, conclusive evidence has not been able to be reached indicating definitively that MWHs lead to fewer perinatal deaths. Furthermore, there is limited data on the effect of MWHs on perinatal outcomes in Ethiopia. Therefore, the aim of this study is to assess the effect of maternity waiting homes on perinatal outcomes in public health facilities in the West Arsi Zone, Oromia Region.
This study will provide valuable information for respective health institutions to improve the quality of MWHs and their expansion to other health facilities where the service has not been launched yet. Besides, this study will contribute to the existing body of knowledge and articulate the basis for other research on the effectiveness of MWH utilization, which will further play a role in averting maternal and childhood morbidity and mortality due to pregnancy-related complications (Figure 1).
2. Methods and Materials
2.1 Study area & period
The study was carried out in public hospitals in the West Arsi Zone. The zone is found in Oromia regional state, Ethiopia. In the zone, there are seven government hospitals: Shashemene Referral Hospital, Melka Oda General Hospital, Dodola General Hospital, Negele Arsi Primary Hospital, Kokosa Primary Hospital, Gambo Primary Hospital, and Loke Primary Hospital. There are three private hospitals (Negele Arsi General Hospital, Feya Primary Hospital, and Madda Walabu General Hospital). Additionally, there are 84 functional health centers, 351 functional health posts, 179 private clinics, 1 NGO clinic, and 95 pharmacy/drug shops. The study was conducted from March 8 to June 1, 2022.
2.2 Study design
An institutional-based prospective cohort study design was employed.
2.3 Source population
All mothers are admitted to public health facilities in the West Arsi Zone.
2.4 Study Population
Exposed: All randomly selected mothers who were admitted through MWHs of public hospitals in West Arsi Zone.
Non-exposed: All randomly selected mothers were admitted to the labor ward of public hospitals in the West Arsi Zone after being admitted directly to the labor ward without MWHs.
2.5 Inclusion and Exclusion Criteria
Inclusion criteria
Exposed: Mothers who were admitted through MWHs of public health facilities in the West Arsi Zone will be included in this study.
Non-exposed: Mothers who were admitted to the labor ward of public health facilities in West Arsi Zone after being admitted directly to the labor ward without MWHs will be included in this study.
Exclusion criteria
Mothers who were referred to other hospitals and don’t have any feedback later about their health status will be excluded, both exposed and non-exposed.
2.6 Sample Size determination
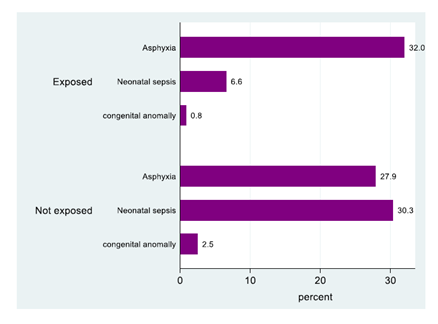
The sample size was calculated using the double proportion formula through Open Epi Info version 7.
Parameters:
n - Size of sample in each group
P1, P2–estimated population prevalence in the comparison groups
β = 1- Power; a power of 80% is used
Using the first objective and considering the following assumptions: 95% Cl, 80% power, 21.7% complicated perinatal outcomes among ANC users, 59.0 complicated perinatal outcomes among those who didn’t have ANC [10], an AHR of 0.61, and exposure to a non-exposed ratio of 1:1. The sample size calculated is 552 (exposed = 276 and non-exposed = 276).
Using the second objective and considering the following assumptions: 95% Cl, 80% power, 9.7% complicated maternal outcome among urban and 90.3% complicated maternal outcome among rural [10], an AHR of 1.79, and exposure to a non-exposed ratio of 1:1. The total sample size calculated is 1460 (730 exposed) and 730 (730 non-exposed).
Finally, the larger sample size was taken (the sample size was calculated using the second objective). Therefore, the total sample size in this study, after adding 10% for lost follow-up was 1,606 (803 exposed and 803 non-exposed).
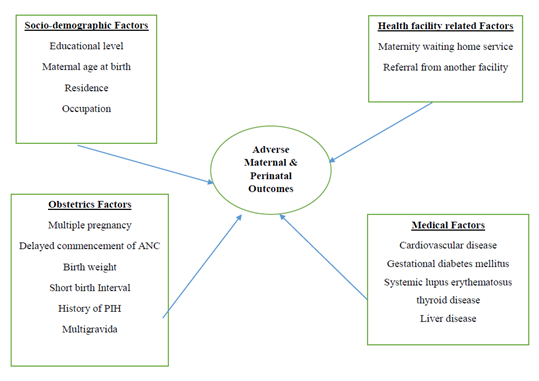
2.7 Sampling procedure
Firstly, out of seven public hospitals in the zone, five hospitals, namely Shashemene Referral Hospital, Melka Oda General Hospital, Dodola General Hospital, Negele Arsi Primary Hospital, and Gambo General Hospital, were selected using a simple random sampling technique. The four-month average number of women admitted through MWHs and directly to labor at each public hospital was identified. Considering the client flow per four months in the respective health institutions, the total sample size determined (1606) was distributed to each public hospital through probability proportional to size allocation. Finally, study participants were selected using a systematic random sampling technique (Figure 2).
2.8 Data collection tool and procedure
Data was collected using a combination of a pretested structured questionnaire through a face-to-face interview and a paired mother and neonatal chart review, which was used to retrieve medical information that could not be captured by the interview. The questionnaire was developed from related literature. The data was collected by five data collectors and supervised by three supervisors.
2.9 Data quality control
Two days of training were given to data collectors on the objectives of the study, sampling, and data extraction procedures. A test was conducted among 5% of the total sample size to check the validity and reliability of the instrument. Data collection was supervised daily by the supervisor and investigators to check consistency, clarity, and completeness.
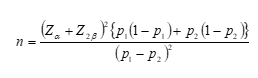
2.10 Study variables
Dependent Variable
Perinatal health outcomes (stillbirth or neonates who are diagnosed with one or more of the following complications; asphyxia, pneumonia, perinatal sepsis, or early neonatal death).
Independent Variables
Socio-demographic Factors: Educational level, maternal age at birth, residence, and occupation.
Medical Factors: cardiovascular disease, gestational diabetes mellitus, systemic lupus erythematosus, thyroid disease, and liver disease.
Obstetrics factors: multiple pregnancies, delayed commencement of ANC, birth weight, short birth interval, history of PIH, and multigravida.
Health Facility Related Factors: Maternity Waiting Home Service and Referral from Another Facility.
Operational & Term definition
MWH Utilizers: pregnant mothers who were admitted to the MWH service and waited until the start of labor.
Perinatal health outcomes: neonates who were diagnosed with either asphyxia, perinatal sepsis, stillbirth, or early neonatal death.
2.11 Data Management and analysis
Data Management
All the questionnaires were checked manually for completeness and will be cleaned, coded, and entered into Epi-data 3.1. Then, the data was exported to and analyzed using Stata version 16.
Data Analysis
Descriptive statistics such as frequencies, proportions, inter-quartile range, mean, median, and standard deviation were calculated to describe socio-demographic and other related variables of the study population and displayed using Tables, Figures, and Graphs.
A generalized linear model (GLM) for binary outcomes was applied for the regression analysis, as this will provide the proper effect size measure (RR) for relatively common outcomes. Both bivariable and multivariable generalized linear model analyses were used to determine the association of each independent variable with the dependent variable. Initially, variables with p < 0.25 in the bivariable generalized linear model were taken into the multivariable logistic regression model. Both crude and adjusted odds ratios with respective 95% confidence intervals and p values <0.05 will be used to measure the strength of the association between dependent and independent variables.
The analysis was done for perinatal health outcomes; those who developed perinatal complications were coded "1,” and those with no complications were coded "0”.
Multicollinearity between the independent variables was assessed using the variance inflation factor (VIF). The maximum VIF value was 1.11 for the perinatal health outcome model, which is close to 1 or less than 10, suggesting there was no multicollinearity problem. Hosmer and Lemeshow goodness of fit statistics were done for each model, and it was found to be a good fit (P = 0.06). The results were interpreted using RR as an effect measure.
2.12 Expected outcome
This study will provide valuable information for respective health institutions in the zone and zonal health departments to improve the quality of MWHs and its expansion to other health facilities where the service has not been launched yet. Besides, this study will contribute to the existing body of knowledge and articulate the basis for other research on the effectiveness of MWH utilization.
3. Result
3.1 Background characteristics of the study participants
In the current study, a total of 1606,803 maternity waiting home users (exposed) and 803 maternity waiting home non-users (non-exposed) were included. The median age of the respondents was 26 (IQR 24, 30). The age ranges from 15 to 38 years. Nearly one-fourth of study participants in the exposed group had no formal education. 179 (22.29%) and 154 (19.18%) study subjects in the non-exposed group had no formal education. Almost three-fourths of study subjects in the exposed group were housewives (596, 74.22%), and more than half of study subjects in the non-exposed group were housewives (553, 68.87%). 785 (97.76%) respondents in the exposed group were married, and 770 (95.89%) study subjects in the non-exposed group were married. All study subjects in the exposed group resided in the rural area 803 (100.0%) (Table 1).
|
Variable |
Category |
Exposed |
Non exposed |
Total n=1606 (%) |
|
No. (%) |
No. (%) |
|||
|
Maternal age |
<20 |
15 (1.87 ) |
46 (5.73) |
61 (3.79) |
|
20-35 |
763 (95.02) |
719 (89.54) |
1482 (92.28) |
|
|
>=35 |
25 (3.11) |
38 (4.73) |
63 (3.92) |
|
|
Marital status |
Married |
785 (97.76) |
770 (95.89) |
1555 (96.82) |
|
Single |
6 (0.75) |
4 (0.50) |
10 (0.62) |
|
|
Divorced |
12 (1.49) |
18 (2.24) |
30 (1.87) |
|
|
Widowed |
0 |
11 (1.37) |
11(0.68) |
|
|
Mother’s educational level |
No formal education |
179 (22.29) |
154 (19.18) |
333 (20.73) |
|
Read & write |
131 (16.31) |
103 (12.83) |
234 (14.57) |
|
|
Primary education |
263 (32.75) |
242 (30.14) |
505 (31.44) |
|
|
Secondary education |
98 (12.20) |
223 (27.77) |
321 (19.99) |
|
|
Diploma and more |
132 (16.44) |
81 (10.09) |
213(13.26) |
|
|
Husband’s educational level |
No formal education |
147 (18.31) |
141 (12.45) |
288 (17.93) |
|
Read & write |
100 (14.82) |
119 (54.34) |
219 (13.64) |
|
|
Primary education |
185 (18.68) |
150 (23.04) |
335 (20.86) |
|
|
Secondary education |
163 (24.91) |
200 (20.30) |
363 (22.60) |
|
|
Diploma and more |
208 (24.03) |
193 (48.13) |
401 (24.97) |
|
|
Mother’s Occupation |
Government employee |
64 (7.35) |
59 (7.97) |
123 (7.66) |
|
Merchant |
64 (7.97) |
86 (10.71) |
150 (9.34) |
|
|
Farmer |
54 (6.72) |
47 (5.85) |
101(6.29) |
|
|
Housewife |
596 (74.22) |
553 (68.87) |
1,149 (71.54) |
|
|
Daily laborers |
14 (1.74) |
48 (5.98) |
62 (3.86) |
|
|
Self employed |
16 (1.99) |
5 (1.31) |
21 (1.31) |
|
|
Place of residence |
Urban |
0 |
429 (100.0) |
429 (26.71) |
|
rural |
803 (68.32) |
374 (31.78) |
1,177 (73.29) |
Table 1: Socio-demographic characteristics of maternity waiting home users and non-users in the public hospitals of West Arsi Zone, 2022.
3.2 Reproductive and medical characteristics of respondents
Two hundred forty-one (30.01%) were primigravida in the exposed group, and nearly half of the study subjects in the non-exposed group were primigravida 330 (41.10%). Nearly one-quarter of the study subjects in the exposed group were in Paragraph 4 and above. 201 (25.03%) and 123 (15.31%) study participants in the non-exposed group were in para 4 and above. 60 (7.47) study participants in the exposed group had no ANC follow-up, 60 (69.77%), and 26 (3.24) study subjects in the non-exposed group had no ANC follow-up, 26 (30.23%) (Table 2).
Nearly one-fourth of the study subjects had experienced obstetric complications; previously, 188 (23.41%) and 98 (12.20%) study subjects in the non-exposed group had experienced obstetric complications. 27 (4.68%) study subjects in the exposed group had C/S previously; 27 (40.30%) and 40 (7.87%) study subjects in the non-exposed group had C/S previously (Table 2).
|
Variable |
Category |
Exposed No. (%) |
Non exposed No. (%) |
Total n=1606 (%) |
|
Gravidity |
1 |
241 (30.01) |
330 (41.10) |
571 (35.55) |
|
45750 |
356 (44.33) |
355 (44.21) |
711 (44.27) |
|
|
>=5 |
206 (25.65) |
118 (14.69) |
324 (20.17) |
|
|
Parity |
0 |
243 (30.26) |
334 (41.59) |
577 (35.93) |
|
45717 |
359 (44.71) |
346 (43.09) |
705 (43.89) |
|
|
>=4 |
201 (25.03) |
123 (15.32) |
324 (20.17) |
|
|
ANC visit |
0 |
60 (7.47) |
26 (3.24) |
86 (5.35) |
|
45717 |
479 (59.65) |
468 (58.28) |
947 (58.97) |
|
|
>=4 |
264 (32.88) |
309 (38.48) |
573 (35.68) |
|
|
History of C/S |
Yes |
27 (4.68) |
40 (7.87) |
67 (4.17) |
|
No |
550 (95.32) |
468 (92.13) |
1018 (63.38) |
|
|
Previous obstetrics complication |
Yes |
188 (23.41) |
98 (12.20) |
286 (17.80) |
|
No |
389 (48.44) |
410 (51.06) |
799 (49.75) |
|
|
Medical disease during pregnancy |
Yes |
16 (1.99) |
58 (7.22) |
74 (4.60) |
|
No |
787 (98.01) |
747 (92.78) |
1534 (95.51) |
|
|
Planned current pregnancy |
Yes |
708 (88.17) |
656 (81.69) |
242 (15.09) |
|
No |
95 (11.83) |
147 (18.31) |
1364 (84.93) |
Table 2: Reproductive and medical characteristics of maternity waiting home users and non-users in the public hospitals of West Arsi Zone, 2022.
3.3 Health service related characteristics of respondents
Seven hundred sixty-four (95.14%) study subjects in the exposed group had traveled 1-2 hours to reach the health facility, and more than three-fourths of the study participants in the non-exposed group had traveled 1-2 hours to reach the health facility (611, 76.09%). More than half of the study participants in the exposed group were transferred from other facilities, 431 (53.67%), and similarly, more than half of the study participants in the non-exposed group were transferred from another facility, 443 (55.17%).
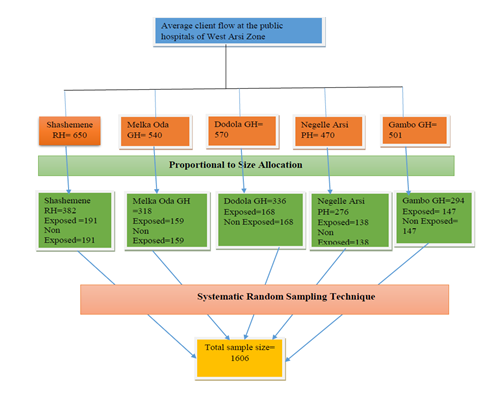
3.4 Perinatal characteristics and perinatal complication
Slightly more than half of study subjects had given birth to female neonates (416, 51.81%), and similarly, more than half of study subjects had given birth to female neonates (477, 59.70%). 49 (6.10%) perinatal complications were developed by exposed groups, and 74 (9.2%) perinatal complications were developed by non-exposed groups. Birth asphyxia was the major complication identified among exposed groups 39 (79.59%), whereas neonatal sepsis was the major complication identified among non-exposed groups 37 (50.0%) (Figure 3).
3.5 Maternity Waiting Homes Services
The median duration of stay at maternity waiting homes was 6 (IQR 4, 9). Almost all of the respondents in the exposed group had received health services. The most common health services given were health education, food, physical examinations, laboratory tests, and antibiotics (18.80%).
3.6 Bi-variable and Multi-Variable Generalized Linear Model Analysis of Perinatal health outcomes
Maternity waiting home utilization, maternal complications, maternal age, type of birth, parity, and sex of the newborn were factors that had p-values less than 0.20 during the bi-variable generalized linear model analysis. After controlling for possible confounders in the multivariable generalized linear model, maternity waiting home utilization, maternal complications, maternal age, and parity were statistically significantly associated with perinatal health outcomes at a p-value <0.05.
Maternity waiting home utilization was an independent risk for perinatal health outcomes. There was a 39% reduced risk of developing perinatal complications in the exposed group when compared to the non-exposed group [RR = 0.61, 95% CL = 0.42, 0.88]. Mothers who developed obstetric complications had a 1.96 times higher risk of developing perinatal complications than those who didn’t develop complications [RR = 1.96, 95% CL (1.39, 2.75)].
Mothers whose ages were 20–35 had a 54% reduced risk of developing perinatal complications compared to those whose ages were greater than 35 years [RR = 0.46, 95% CL (0.26, 0.82). Nulliparous women had an 88% reduced risk of developing perinatal complications compared to those who were para 4 and above [RR = 0.22, 95% CL = 0.12, 0.43%] (Table 3).
|
Variable |
Category |
Complicated No. (%) |
Uncomplicated No. (%) |
CRR (95% Cl) |
ARR (95% Cl) |
P-value |
|
Maternity home utilization |
Utilized (Exposed) |
49 (6.10) |
754 (93.90) |
0.66 (0.47, 0.93) |
0.61 (0.42, 0.88) * |
0..008* |
|
Not utilized (non-exposed) |
74 (9.22) |
729 (90.78) |
1 |
1 |
1 |
|
|
Maternal complication |
Yes |
52 (12.53) |
363 (87.47) |
2.10 (1.49, 2.95) |
1.96 (1.39, 2.75)* |
0.000* |
|
No |
71 (5.96) |
1,120 (94.04) |
1 |
1 |
1 |
|
|
Maternal age |
<20 |
6 (9.84) |
55 (90.16) |
0.44 (0.18, 1.07) |
1.39 (0.47, 4.08) |
0.55 |
|
20-35 |
103 (6.95) |
1,379 (93.05) |
0.31 (0.19, 0.51) |
0.46 (0.26, 0.82)* |
0.008* |
|
|
>35 |
14 (22.22) |
49 (78.78) |
1 |
1 |
1 |
|
|
Type of birth |
Singleton |
118 (7.63) |
1,429 (92.37) |
0.90 (0.38, 2.12) |
0.62 (0.26, 1.50) |
0.294 |
|
Twin |
5 (8.47) |
54 (91.53) |
1 |
1 |
1 |
|
|
Parity |
0 |
19 (3.29) |
558 (96.71) |
0.27 (0.16, 0.46) |
0.22 (0.12, 0.43)* |
0.000* |
|
45717 |
65 (9.22) |
640 (90.78) |
0.76 (0.53, 1.11) |
0.84 (0.54, 1.30) |
0.439 |
|
|
≥4 |
39 (12.04) |
285 (87.96) |
1 |
1 |
1 |
|
|
Sex of newborn |
Male |
64 (7.17) |
829 (92.83) |
1.15 (0.82, 1.62) |
0.88 (0.62, 1.25) |
0.481 |
|
Female |
59 (8.27) |
654 (91.73) |
1 |
1 |
1 |
|
|
RR-adjusted for maternal complication, maternal age, type of birth, parity and sex of newborn *Significant with multiple logistic regression at p-value ≤0.05 |
||||||
Table 3: Bivariable & Multivariable generalized linear model for the effect of maternity waiting home utilization on perinatal health outcomes, 2022 (n=1606).
4. Discussion
The primary aim of the current study was to determine the effect of maternity waiting home utilization on perinatal health outcomes. According to the present study, maternity waiting home users had a 39% reduced risk of developing a perinatal complication when compared to non-users. This finding is supported by a study done at the national level, which found that the direct obstetric complication rate was 49% lower at hospitals with maternity waiting homes compared to hospitals without maternity waiting homes [11].
The present study revealed that maternity waiting home users had a reduced risk of developing perinatal complications when compared to non-users. A similar finding was found in a study conducted in Yetebon, Ethiopia, in which MWH use was associated with a 77% lower risk of childbirth complications and a 94% lower risk of fetal and newborn complications [12]. Similarly, a study done in health facilities in Gurage Zone revealed that MWH users had lower odds of having delivery complications, which is consistent with the present study [13].
Likewise, a study carried out in the Tigray region revealed a similar finding to the present study, in which the incidence rates of perinatal death and complications were significantly lower among the maternal waiting home users than non-users [10]. The present study is also in line with a nested case-control study conducted at St. Luke Hospital in Wolisso, which showed the protective effect of maternity waiting home utilization on perinatal mortality and a more protective effect after adjusting for confounders. [14].
Similarly, a study conducted at the national level found a similar finding with the present study, in which perinatal mortality was 47% lower in hospitals with maternity waiting homes than those without maternity waiting homes [11].
A systematic review done in Africa found that utilizing MWHs has a significant effect on reducing PNM by 82.5%, which is consistent with the current study [15]. Another systematic review done in developing countries found that there was 73% less occurrence of stillbirth among users, which contributes to the reduction of 83% of stillbirths compared to non-users, which is also in line with the present study [16].
The present study showed that mothers whose ages were 20–35 had a 54% reduced risk of developing perinatal complications compared to mothers whose ages were greater than 35 years. This might be due to the fact that as women get older, the risk of getting chronic illnesses is high, and these diseases might expose the mother to developing obstetric complications.
This finding is consistent with the study carried out in Debre Tabor town, Ethiopia, which found that a mother’s age was associated with adverse pregnancy outcomes [17]. Similarly, a study conducted in North-West Ethiopia found a consistent finding with the present study, in which the odds of composite adverse perinatal outcomes were higher among advanced maternal-age women when compared to adults [18]. Similarly, a study carried out in China found a consistent finding: maternal age of 35 years or older was found to be significantly associated with at least one adverse outcome [19].
The present study also found that mothers who developed obstetric complications had a 1.96 times higher risk of developing perinatal complications than those who didn’t develop complications. This could be due to the fact that any complications for the mother will have a direct and significant effect on the fetus and newborn, as the fetus is solely dependent on maternal circulation for nutrition, gas exchange, and other physiological processes. This finding is supported by a study conducted in Northwest Ethiopia, which found that complications during pregnancy were also factors significantly associated with adverse perinatal outcomes. This finding is also in line with a study done in Gurage Zone, which revealed that women who did not use MWH were more likely to develop delivery complications, and women with delivery complications had higher odds of undergoing cesarean delivery and neonatal death [18].
The current study also found that nulliparous women had an 88% reduced risk of developing perinatal complications compared to those who were para 4 and above. This might be due to the fact that obstetric complications are likely to repeat themselves and are also related to advanced age.
A similar finding was found in a study carried out in the Sidama region, in which women with grand multiparity gave birth to babies with a higher risk of stillbirth and preterm birth [20]. This finding is also in line with a study carried out in Northern Tanzania, which found that grand multiparous women had increased odds of prelabour rupture of membranes, stillbirth, and preterm birth delivery as compared to women in the lower parity group [21]. Similarly, in a study carried out in China, multigravida was found to be significantly associated with at least one adverse outcome, which is consistent with the present study [19,22-39].
5. Strength and Limitations
Strengths
Use of a relatively large sample size with strong power.
Use of a prospective cohort study design that is strong at elucidating temporal relationships.
Employment of a generalized linear model to estimate relative risk as this is the proper effect size measure for relatively common outcomes.
Limitations
The incidence rate was not determined as the date and time of admission and complications are not clearly written in the women and neonates chart.
6. Conclusion
The present study found that maternity waiting home users had a reduced risk of developing perinatal complications when compared to non-users. Besides, advanced maternal age, multiparity, and maternal complications were independent predictors of perinatal complications. Moreover, maternity waiting home utilization had an evident impact on reducing perinatal complications.
7. Declarations
Acknowledgement
We would like to thank the Madda Walabu University Shashemene campus research, community engagement, and technology transfer coordination office for providing us with an unrivaled opportunity to carry out this research task. We are also grateful to our colleagues for their unreserved guidance and timely, relevant, and constructive comments from the course of the development of the proposal to the thesis write-up. At last, we would like to extend our sincere thanks to the study participants, data collectors, and respective officials of the hospitals, without whom this thesis wouldn’t have been realized.
Funding
Madda Walabu University funded the research, and it is open for the researchers to publish the manuscript. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The data sets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Before commencing data collection, the Ethical Review Committee of Madda Walabu University, Shashemane Campus provided approval. A letter of authorization was also received from the West Arsi Zone Health Office. In addition, verbal consent was obtained from study participants to confirm their willingness to participate after explaining the objective of the study. Respondents were notified about their right to refuse or terminate at any point of the interview. The information provided by each respondent was kept confidential.
Competing interests
The authors declared that there were no conflicts of interest.
Consent for publication
Not Applicable.
Strobe checklist
Not Applicable.
Authors' contributions
NG, AE and MAH conceptualized the idea, analyzed the data and drafted the manuscript. AU and DY improved the drafted manuscript and significantly revised the manuscript for methodological and scholarly essence. All authors have read and approved the final manuscript.
Supplementary Files: https://cdn.fortunejournals.com/supply/supplyjppch-12960.pdf
References
- Andina M, Figa-Talamanca I. Safe motherhood maternal waiting home a review of experience WHO. Geneva (1996).
- Hug L, Alexander M, You D, et al. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis (2019).
- Central Statistical Agency. Ethiopian Demographic and Health Survey. Addis Ababa, Ethiopia (2016).
- Vermeiden T, Stekelenburg J. Maternity Waiting Homes as Part of an Integrated Program for Maternal and Neonatal Health Improvements: Women's Lives Are Worth Saving Journal of Midwifery & Women's Health 62 (2017): 151-4.
- Osborn D, Cutter A, Ullah F. Universal Sustainable Goals. Understanding the Transformational Challenge for Developed Countries (2015).
- Sialubanje C, Massar K, Pijl MSGVD, et al. Improving access to skilled facility-based delivery services: Women’s beliefs on facilitators and barriers to the utilisation of maternity waiting homes in rural Zambia. Reproductive Health 12 (2015).
- Gaym A, Pearson L, Soe KWW. Maternity waiting homes in Ethiopia--three decades’ experience. Ethiop Med J 50 (2012): 209-19.
- Ethiopian Public Health Institute, Averting Maternal Death and Disability. Ethiopian Emergency Obstetric and Newborn Care (EmONC) Assessment (2016).
- Hodin S. Maternity Waiting Homes: A Viable Solution for Rural Women? (2017).
- Gebremeskel TZ. Effect of Maternal Waiting Home Utilization on Maternal and Perinatal Health Outcomes, in Selekleka Primary Hospital, Northern Ethiopia: Retrospective Cohort Study. Addis Ababa: Addis Ababa University (2018).
- Tiruneh GT, Getu YN, Abdukie MA, et al. Distribution of maternity waiting homes and their correlation with perinatal mortality and direct obstetric complication rates in Ethiopia. BMC Pregnancy and Childbirth 19 (2019).
- Erickson AK, Abdalla S, Serenska A, et al. Association between maternity waiting home stay and obstetric outcomes in Yetebon, Ethiopia: a mixed-methods observational cohort study. BMC Pregnancy and Childbirth 21 (2021).
- Getachew B, Liabsuetrakul T, Gebrehiwot Y. Association of maternity waiting home utilization with women's perceived geographic barriers and delivery complications in Ethiopia. Int J Health Plan Mgmt 35 (2020).
- Zuanna TD, Fonzo M, Sperotto M, et al. The effectiveness of maternity waiting homes in reducing perinatal mortality: a case–control study in Ethiopia. BMJ Global Health 6 (2012).
- Bekele BB, Dadi TL, Tesfaye T. The significant association between maternity waiting homes utilization and perinatal mortality in Africa: systematic review and meta-analysis. BMC Res Notes 12 (2019).
- Dadi TL, Bekele BB, Kasaye HK. et al. Role of maternity waiting homes in the reduction of maternal death and stillbirth in developing countries and its contribution for maternal death reduction in Ethiopia: a systematic review and meta-analysis. BMC Health Services Research 18 (2018): 748-18.
- Kebede AS, Muche AA, Alene AG. Factors associated with adverse pregnancy outcome in Debre Tabor town, Northwest Ethiopia: a case control study. BMC Res Notes 11 (2018).
- Getaneh T, Asres A, Hiyaru T. et al. Adverse perinatal outcomes and its associated factors among adult and advanced maternal age pregnancy in Northwest Ethiopia. Scientific Reports 11 (2021).
- Li U, Zhang W, Lin J, et al. Risk factors for adverse maternal and perinatal outcomes in women with preeclampsia: analysis of 1396 cases. Clin Hypertension 20 (2018): 1049-1057.
- Dasa TT, Okunlola MA. Dessie Y. Effect of Grand Multiparity on the Adverse Birth Outcome: A Hospital-Based Prospective Cohort Study in Sidama Region, Ethiopia 14 (2022): 363-372.
- Muniro Z, Tarimo CS, Mahande MJ, et al. Grand multiparity as a predictor of adverse pregnancy outcome among women who delivered at a tertiary hospital in Northern Tanzania. BMC Pregnancy and Childbirth 19 (2019): 222.
- Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med 38 (1994).
- Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization (2019).
- Trends in Maternal Mortality 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2015a).
- Ekunwe AB. The Efficacy of Maternity Waiting Homes in Decreasing Maternal and Perinatal Mortality in Low-Income Countries: A Systematic Review. The University of Arizona (2017).
- Lugobei HM, Muhindo R, Kayondo M, et al. Risks of adverse perinatal and maternal outcomes among women with hypertensive disorders of pregnancy in southwestern Uganda. PLoS ONE 15 (2020).
- Bekele BB, Dadi TL, Tesfaye T. The significant association between maternity waiting homes utilization and perinatal mortality in Africa: systematic review and meta-analysis. BMC Res Notes 12 (2019).
- Braata F, Vermeidena T, Getneta G, et al. Comparison of pregnancy outcomes between maternity waiting home users and non-users at hospitals with and without a maternity waiting home: retrospective cohort study. International Health 10 (2018): 47-53.
- Ethiopian Public Health Institute (EPHI)[Ethiopia] and ICF. Ethiopia mini demographic and health survey 2019: key indicators (2019).
- Harrison MS, Betrán AP, Suresh K, et al. Risk factors associated with adverse maternal outcomes following intrapartum cesarean birth: a secondary analysis of the WHO global survey on maternal and perinatal health, 2004–2008. BMC Pregnancy and Childbirth 20 (2020).
- Lonkhuijzen LV, Stekelenburg J, Roosmalen JV. Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries Cochrane Database of Systematic Reviews (2012).
- Lori JR, Perosky J, Munro-Kramer ML, et al. Maternity waiting homes as part of comprehensive approach to maternal and newborn care: a cross-sectional survey. BMC Pregnancy and Childbirth 19 (2019).
- Loria JR, Munrob ML, Rominskic S, et al. Maternity waiting homes and traditional midwives in rural Liberia. Int J Gynaecol Obstet 123 (2013): 114-118.
- Saaka M, Aryee P, Kuganab-Lem R, et al. The effect of social behavior change communication package on maternal knowledge in obstetric danger signs among mothers in East Mamprusi District of Ghana. Globalization and Health 13 (2017).
- Sadiq AA, Poggensee G, Nguku P, et al. Factors associated with adverse pregnancy outcomes and perceptions of risk factors among reproductive age women in Soba LGA, Kaduna State 2013. Pan African Medical Journal 25 (2016).
- Singh K, Speizer I, Kim ET, et al. Reaching vulnerable women through maternity waiting homes in Malawi. Int J Gynecol Obstet 136 (2017): 91-97.
- Souza JP, Widmer M, Gülmezoglu AM, et al. Maternal and perinatal health research priorities beyond 2015: an international survey and prioritization exercise. Reproductive Health 11 (2014).
- Making pregnancy safer: the critical role of the skilled attendant. a joint statement by WHO, ICM and FIGO (2004).
- WHO. WHO recommendations on health promotion interventions for maternal and newborn health (2015b).


 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 