Acute Complications of Sickle Cell Disease: A Retrospective Study in Pediatric Emergency Departments
Amadou Sow1, Yaay Joor Dieng2, Dieynaba Fafa Cisse2, Aliou Thiongane2, Ndeye Fatou Sow2, Djibril Boiro1, Guilaye Diagne2, Aminata Mbaye2, Awa Kane2, Cheikh Tidiane Diagne1, Moussa Seck3, Amadou Lamine Fall1, Indou Deme Ly2, Ousmane Ndiaye1*
1Abass Ndao Hospital, Fann, Dakar, Senegal
2Albert Royer National Hospital, Fann, Dakar, Senegal
3National Blood Transfusion Center, Fann, Dakar, Senegal
*Corresponding Authors: Amadou Sow, Pediatrician, Abass Ndao Hospital, Fann, Dakar, Senegal.
Received: 09 October 2025; Accepted: 24 October 2025; Published: 31 October 2025
Article Information
Citation: Amadou Sow, Yaay Joor Dieng, Dieynaba Fafa Cisse, Aliou Thiongane, Ndeye Fatou Sow, Djibril Boiro, Guilaye Diagne, Aminata Mbaye, Awa Kane, Cheikh Tidiane Diagne, Moussa Seck, Amadou Lamine Fall, Indou Deme Ly, Ousmane Ndiaye. Acute Complications of Sickle Cell Disease: A Retrospective Study in Pediatric Emergency Departments. Journal of Pediatrics, Perinatology and Child Health. 9 (2025): 190-192.
View / Download Pdf Share at FacebookAbstract
Introduction: Sickle cell anemia is an autosomal recessive genetic disease, linked to the synthesis of an abnormal hemoglobin called hemoglobin S. It manifests itself with acute complications that can be fatal. The objective of this work was to evaluate the management of acute complications of sickle cell anemia in the emergency room.
Methods: This was a retrospective and descriptive study over 12 months (January-December 20) concerning children hospitalized in the SAU for acute complications of sickle cell anemia.
Results: The prevalence of acute complications of sickle cell disease in the emergency room was 5.82%. The average age was 8.14 years (6 months - 18 years) including 53.85% boys. The reasons were dominated by bone pain (55.77%), fever (34.62%). Asthenia was noted in 84.62% of patients, pallor 82.69%. Respiratory distress was noted in 69.23% of cases. The average hemoglobin level was 7.3 g/dl (2.7 - 9.2 g/dL. The main complications were bone CVO (37.23%), acute hemolysis (30.77%), acute infections (13.46%), acute chest syndrome (11.54%). Management included hydration by infusion (98.08%), antibiotic therapy (48%), transfusion (53.84%) and oxygen therapy (28.84%). Level II analgesics were more used (88.5%). There were 2 deaths.
Conclusion: Acute complications of sickle cell disease are common in emergency departments. They require rapid and adequate treatment for a better prognosis. Emphasis should be placed on primary prevention through genetic counseling.
Keywords
<p>Child; Sickle cell anemia; Hemolysis; Vaso-occlusive crises; Senegal</p>
Article Details
1. Introduction
Sickle cell anaemia is the most widespread genetic disease in the world, linked to the synthesis of an abnormal haemoglobin called haemoglobin S, the polymerisation of which leads to fragility of RBCs, resulting in hyperhaemolysis, vaso-occlusive attacks and loss of their plasticity. The most frequent complications are vaso-occlusive crises, acute haemolysis and infections, especially bacterial infections. Serious vaso-occlusive accidents are characterised by strokes, acute thoracic syndrome and priapism [1]. These complications are serious, even fatal, and must be recognised and treated early to prevent sequelae [1]. The aim of this study was to evaluate the management of acute complications of sickle cell disease in children in emergency departments, to determine the prevalence of these complications, the main reasons for consultation and the evolutionary aspects.
2. Methodology
This was a retrospective study over a 12-month period (1 January to 31 December 2020) including patients aged less than 15 years hospitalised for complicated homozygous sickle cell disease in the emergency department of the Centre Hospitalier National d'Enfants Albert Royer (C.H.N.E.A.R) in Dakar. Data were collected from hospital records and registers. Sociodemographic, clinical, therapeutic and evolutionary parameters were collected and analysed. Data entry and analysis were performed using the following software: Excel 2010 and Epi info 7.2. During analysis, qualitative variables were described using frequency tables, bar charts and pie charts. Quantitative variables were described by their positional parameters (mean, median and mode) and dispersion (standard deviation, extremes).
3. Results
3.1 Sociodemographic data
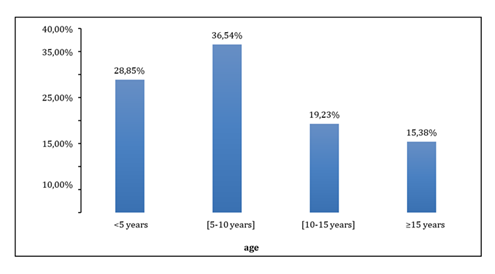
During the study period the number of children hospitalized in the Emergency Department was 894, 52 of whom presented with an acute complication of sickle cell disease, i.e. a prevalence of 5.82%. The mean age of the children was 8.14 ± 4.94 years, with extremes of 0.5 and 18 years. The mode and median were 8 years. The 5-9 age group accounted for the majority (36.54%, n=19). The majority were male (53.85%). The sex ratio was 1.17. The place of origin was provided for 46 patients; almost all 89.13% (n=41) came from the Dakar region and mainly from its suburbs 56.52% (n=26). Figure 1 shows the distribution of patients by age.
3.2 Clinical and paraclinical data
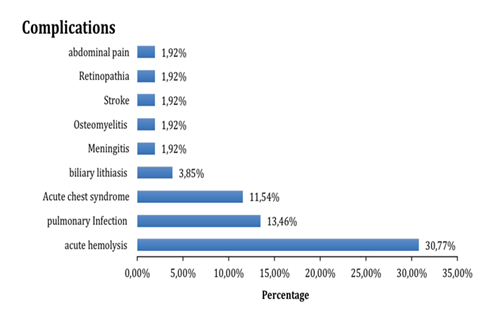
Bone pain 55.77%(n=29), abdominal pain 34.62%(n=18) and fever 34.62%(n=18) were the main reasons for consultation which are illustrated in Figure 2. Asthenia 84.62% (n=44) and pallor 82.69% (n=43) were the main general signs. Among patients with physical signs, bone pain (n=35) was in the majority. Nine (9) patients presented with respiratory distress and 14 with abdominal pain. The minimum haemoglobin concentration was 2.7 g/dl while the maximum was 9.2 g/dl on CBC. Anaemia, hyperleukocytosis and thrombocytopenia were noted in 84.62%, 51.92% and 23.07% of patients respectively. Chest X-rays were taken in 12 patients (23.08%), 41.67% of whom had an acute chest syndrome. Acute haemolysis was the main complication (30.77%).
3.3 Treatment and outcome
Hyperhydration was the predominant treatment at 98.08% (n=51). The most commonly used antibiotics were 3rd generation cephalosporins (C3G) 64.00% (n=16). In terms of analgesic treatment, paracetamol was used in most cases (83%). Morphine was used infrequently (6%). Almost all patients (96.15%, n=50) had a favourable outcome; 2 cases of death (3.85%) were recorded. The distribution of patients according to the complications is shown in Figure 2.
4. Discussion
4.1 Epidemiological data
The frequency of hospital admissions was 52, or 5.82% of children with sickle cell disease admitted for an acute complication, an average of 4.33 cases per month. The peaks were observed in January and February (11.54%), corresponding to the cold season with an upsurge in viral infections. This is a period when children with sickle cell disease are exposed to complications due to temperature variations [1]. The average age of the children was 8.14 years, with extremes of 5 months and 18 years. Older children over 5 years of age predominated (36.54%). Complications of sickle cell disease are more frequent in older children because of the disappearance of foetal haemoglobin. The predominance was male (53.85%) and the ratio of boys to girls was 1.17. The same data are noted in the literature with 2.12 and 1.34 [2]. However, some authors have found an identical sex distribution and indifference to CVO.
4.2 Clinical and biological data
The main reasons for consultation were bone pain (55.77%), abdominal pain (34.62%) and fever (34.62%). This was the same finding as for Bertholdt, with a slightly higher frequency of 40% [2]. Asthenia and pallor were the general signs most frequently noted in patients (84.62% and 82.69% respectively). Half the patients had a fever on admission. Higher rates have been reported in the literature (95.5% [3]). Respiratory signs were dominated by respiratory distress (69.23%), which is most often symptomatic of acute chest syndrome or sickle cell pneumonia. The same is true in the literature, with a lower frequency of 50% [3]. The biological signs were mainly normocytic normochromic anaemia and hyperleukocytosis (51.92%), reflecting acute haemolysis on a chronic background and a generally bacterial infection, respectively. This haemolytic anaemia is accompanied by hyperbilirubinaemia clinically manifested as non-cholestatic jaundice. The same observations have been made in the literature [4].
4.3 Treatment
Hydration by intravenous infusion was almost systematic for all the children (98.08%). This is logical, given that these children arrive with AEG, sometimes with anorexia and an inability to eat. IV infusion is essential to ensure maintenance fluid requirements. In addition to its hydration role, the infusion improves pain by improving blood volume and oxygenation. The same rates are noted in the literature, with 85.7% [5]. Lower rates were also noted at 66.6%. Red blood cells were exclusively transfused. Bertholdt et al. [2] transfused 44% of their patients with packed red blood cells. Ideally, patients should be transfused with phenotyped red blood cells, but phenotyped blood is not available in our context. Level I and II analgesics were the most commonly used in our department because of the lack of level III analgesics, in contrast to Bertholdt, who used level III analgesics (morphine) in 33.33% of cases. Because of the intensity of pain in CVO sickle cell patients, tier III analgesics should be used as first-line treatment. In our context, the limited availability and delicate handling of morphine explain the use of levels I and II. 3rd generation cephalosporins were the most commonly used in the management of bacterial infections (64%). The same was true of Douamba, with a 64.6% usage rate. The combination of amoxicillin and clavulanic acid was used in 16% of cases, which is low in relation to the rarity of staphylococcus as the germ causing infections in sickle cell patients. Dual antibiotic therapy was used in 86.66% of cases. The same observation can be made in the literature [6]. Oxygen therapy concerned 28.85% of patients. The outcome was favourable for almost all children with survival in 96.15% of cases. There were 2 cases of death. This rate was lower than that found in Burkina 7.5% [6].
4.4 Acute complications
Acute haemolysis leading to worsening of the anaemia was present in 30.77% of cases. This haemolysis is often due to infection or the presence of irregular agglutinins. The frequency of infections in children with sickle cell disease explains the preponderance of this complication [7]. The second most frequent complication (13.46%) was infection, mainly of the lungs in the form of pneumonia. They are favoured by a low immune status, but also, and above all, by the absence of vaccination, particularly the pneumococcal vaccine. Osteoarticular infections came second after pneumonia. Acute chest syndrome was less frequent than pneumonia and acute haemolysis. It was observed in 11.54% of children, which is significantly lower than the data in the literature, where it occurs in up to 75% of cases [3]. This difference in frequency may be explained by the fact that ATS is under-diagnosed because it is often confused with acute pneumonia. Other less frequent complications were bacterial meningitis and stroke, accounting for 1.92% of cases of each. As a result of the pneumococcal vaccination available in the EPI, pneumococcal meningitis has become rare in children in general and sickle cell patients in particular. Strokes are major vaso-occlusive accidents which must be detected and prevented at all costs, as they are life-threatening and can have functional consequences with motor sequelae.
5. Conclusion
Acute complications of sickle cell disease are common in emergency departments. They require rapid and appropriate treatment to ensure a better prognosis. Emphasis must be placed on primary prevention through genetic counselling.
References
- Galacteros F. Sickle cell disease: pathophysiology and diagnosis. Rev Prat 54 (2004): 1534-1540.
- Fournier C, Benkerrou M, Vilmer E, et al. Evolution de l'activité liée à la drépanocytose à l’hôpital de Robert-Debré (Paris), entre 1992 et 1996. Arch Pediatr 7 (2000): 465-473.
- Fauroux B, Epaud R, Clement A. Acute chest syndrome in children. In Girot R, Bégué P, Galactéros F. La Drépanocytose. Paris: John Libbey; 2003: 125-133.
- Parot A, Maitre B. Acute thoracic syndrome in adults. In Girot R, Bégué P, Galactéros F. La Drépanocytose. Paris: John Libbey; 2003: 135-143.
- Diagne I, Diagne Gueye Nd R, Fall L, et al. Acute encephalic manifestations in Senegalese children with sickle cell disease. Dakar Med 47 (2001): 116-120.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 91 (1998): 288-294.
- Wajcman H. Diagnosis and screening for sickle cell disease. Rev Prat 54 (2004): 1543-1546.


 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 