Bariatric Surgery Outcomes on Type 2 Diabetes Remission in Non-Obese Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis
Mostafa Jihad1, Babak Nakhjavan Shahraki2, Havila Tiyyagura3, Shah Zaib Bhindar4, Sidra Baig5, Akash Ranganatha6, Bhavna Singla7, Shivam Singla8, Eman Alamin9, Binish Essani10, Marium Abid11, Muhammad Sohail S. Mirza12*
1Lodz Medical University, Poland
2Zahedan University of Medical Sciences, Iran
3Guntur Medical College, Guntur, Andhra Pradesh, India
4Nishtar Medical College, Multan, Pakistan
5Dr. VRK Women’s Medical College, Aziznagar, Telangana, India
6JJM Medical College, Davangere, Karnataka, India
7Erie County Medical Center, Buffalo, NY, USA
8Tidal Health Peninsula Regional, Salisbury, MD. USA
9University of Medical Sciences and Technology (UMST), Khartoum, Sudan
10Jinnah Medical and Dental College, Karachi, Pakistan
11Jinnah Medical & Dental College, Karachi, Pakistan
12Muhammad Sohail S. Mirza, MBBS. Shandong University School of Medicine, Jinan, China
*Corresponding author: Muhammad Sohail S. Mirza, Shandong University School of Medicine, Jinan, China.
Received: 28 August 2025; Accepted: 05 September 2025; Published: 15 September 2025
Article Information
Citation: Mostafa Jihad, Babak Nakhjavan Shahraki, Havila Tiyyagura, Shah Zaib Bhindar, Sidra Baig, Akash Ranganatha, Bhavna Singla, Shivam Singla, Eman Alamin, Binish Essani, Marium Abid, Muhammad Sohail S. Mirza. Bariatric Surgery Outcomes on Type 2 Diabetes Remission in Non-Obese Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis. Archives of Internal Medicine Research. 8 (2025): 272-284.
View / Download Pdf Share at FacebookAbstract
Chronic symptoms such as epigastric pain, bloating and early satiety are the main features of functional dyspepsia (FD). Even though the Low-FODMAP diet is beneficial for IBS, more research is needed to determine its effects on FD. The purpose of this review was to find out how helpful the Low-FODMAP diet is for people with FD. A search was made in well-known databases (PubMed, web of science, Cochrane Library, Google Scholar) to find randomized controlled trials (RCTs) and observational studies published between 2020 and 2025. Studies that looked at the difference between Low-FODMAP diet and either control dietary advice or placebo in people with FD were included. Analysis of pooled data was performed and effect size was calculated using a random-effects model. The degree of heterogeneity was tabulated using the I² statistic and funnel plotting and Egger’s test were carried out to check for publication bias. From the total number of studies investigated, ten were used for the review since they mirrored the criteria. The combined analysis showed that following the Low- FODMAP diet led to fewer symptoms in the gut and a better quality of life for people with FD (r = 0.29, 95% CI: -0.03 to 0.57). The diet may noticeably enhance psychological outcomes, and reductions in anxiety and depression were found in several studies. Ongoing research is, however, complicated by the presence of significant heterogeneity (I² = 94.5%) among studies. The intervention would hence indicate variability in treatment outcomes. This gives credence to the Low- FODMAP diet as a good intervention for gastrointestinal symptoms in FD and is likely to promote psychological well-being. Although the heterogeneity was observed, overall results encourage such a diet for this specific: management of FD. More studies should be conducted to standardize protocols, determine their long-term effects, and better understand the psychological implications of the diet.
Keywords
<p>Bariatric Surgery; Diabetes Remission; Roux-en-Y Gastric Bypass; Sleeve Gastrectomy; Non-Obese Patients</p>
Article Details
Introduction and Background
Bariatric surgery (BS) has long been considered the gold standard for treating severe obesity, primarily focusing on inducing significant weight loss [1,2]. However, recent advances in metabolic surgery suggest that its benefits extend beyond weight reduction to the management of type 2 diabetes (T2D), especially in patients with metabolic syndrome (MS) [3]. MS is a complex of diseases that encompasses such disorders as hypertension, dyslipidemia, and insulin resistance, and causes a substantial risk of developing cardiovascular diseases and T2D [4]. Traditionally, BS was indicated for patients with morbid obesity (BMI > 35), but emerging evidence supports its potential benefits for less obese individuals, including those with BMI < 30, particularly in the context of MS [5].
In patients with T2D and MS, insulin resistance and impaired glucose metabolism are key challenges. These patients often experience difficulties in managing their condition with conventional pharmacologic interventions [6]. There are encouraging outcomes developed by BS that have improved glycemic control and even caused remission of diabetes since they have shown that surgery is effective in inducing both improvement in metabolic outcomes (MO) and resolving associated comorbidities [7]. The BS and T2D remission correlation is not simple and depends on such factors as the years of diabetes, the procedure of the surgery that was used, and the initial insulin sensitivity [8]. It should be mentioned that the patients with a shorter history of T2D and with well-maintained pancreatic beta-cells have more positive outcomes after the surgery [9].
Among those patients who have MS but are not obese, the question of whether to have BS or not is often informed by a risk-benefit analysis of the patient [10]. As much as the clinical advantages of BS in obese patients with T2D are under-documented, its influence on non-obese groups has been the field of future research[11]. Evidence has proven that the results of BS in non-obese patients are similar to those recorded in morbidly obese patients, recording the same percentage of diabetes remission (DR) and modified metabolic indices [12]. The surgery, which has been tested on whether it would be effective in treating diabetes in MS patients, is a surgical technique like Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and mini-gastric bypass (MGB) and some of literature evidence has indicated that MGB has the potential for superior early results in DR relative to sleeve gastrectomy [13,14].
Long-term sustainability of DR is a central question of BS in non- obese subjects. Although most patients undergo remarkable improvements in glycemic control in the perioperative period, relapses relating to diabetes have been witnessed even after several years in some of the patients [15]. The type of bariatric procedure, initial insulin sensitivity of the patients, and sustainability of weight loss are among the factors that are very important in predicting the lasting success of the intervention [16]. The findings of cohort studies and systematic reviews of large-scale evidence indicate that remission rates amongst patients who lose more weight and reduce insulin resistance after surgery are often greater [17].
The current systematic review and meta-analysis study will evaluate the efficacy of BS in inducing the remission of T2D among non-obese patients (NOP) with MS, determine the influence of various surgical procedures, and identify factors that predict successful results. The review will also examine the long-term nature of such benefits through a critical evaluation of the circumstances surrounding factors of remission and relapse. Finally, this paper would be useful in the field of promoting of the discussion regarding the effectiveness of BS to treat T2D without obesity and may effectively be used in clinical practice and decision-making by patients.
Methods
Data Sources and search strategy
The study was done by conducting a systematic literature search to examine the impact of BS on remission of T2D among the NOP with MS. The search of literature was conducted in many electronic collections, such as PubMed, Cochrane Library, and Google Scholar. To entail the most recent evidence, the search was limited to the articles that were published between 2000 and 2025. The search strategy has been conducted according to the PRISMA standards in order to provide a clear and repeatable method for further investigators. To best maximize retrieval of relevant studies, a combination of both keywords and vocabulary terms (e.g., MeSH terms) was employed. The following search terms were included: “bariatric surgery,” “metabolic syndrome,” “type 2 diabetes,” “non-obese,” “remission,” “glycemic control,” and “metabolic outcomes.” Boolean operators such as AND and OR were used to combine the search terms. Studies published in English were included in the search process. To further capture all relevant literature, the references of identified studies were automatically searched to find additional publications that may not have been captured in the initial database search.
Table 1: Search strategy across databases
|
Database |
Search Terms Used |
Filters Applied |
Truncations/Syntax |
|
PubMed |
"bariatric surgery" AND "metabolic syndrome" AND "type 2 diabetes" AND "non-obese" AND "remission" AND "glycemic control" |
Human studies, English language, 2000-2025 |
("bariatric surgery"[MeSH] OR "metabolic syndrome"[MeSH]) |
|
Cochrane Library |
"Bariatric surgery" AND "metabolic syndrome" AND "type 2 diabetes" AND "non-obese" AND "remission" AND "long-term outcomes" |
RCTs, Human studies, English, 2000-2025 |
Use of Boolean operators (AND, OR) |
|
Google Scholar |
("bariatric surgery" OR "metabolic surgery") AND ("type 2 diabetes" AND "non-obese" AND "remission" AND "metabolic syndrome") |
English language, 2000-2025 |
Exact phrase search using quotes for clarity |
Inclusion and exclusion criteria
The PICOS framework facilitated the critical evaluation process, ensuring a structured and precise selection of studies that specifically examined the effects of BS on T2D remission in NOP with MS, based on the defined population, intervention, comparison, outcomes, and study design (Table 2).
Table 2: PICOS Framework for Recent Study.
|
PICOS Element |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Non-obese adults (BMI < 30 kg/m2) identified with MS (presence of at least three mechanisms: abdominal obesity, dyslipidemia, hypertension, insulin resistance). |
Obese patients (BMI ≥ 30 kg/m2) or those with T1D. |
|
Intervention |
BS (e.g., RYGB, MGB) for diabetes management. |
Non-surgical interventions (e.g., pharmacological treatments, lifestyle modifications) or surgeries unrelated to MS and diabetes management. |
|
Comparison |
Studies comparing BS with other interventions or baseline pre-surgery conditions. |
Studies with no comparison group or studies with comparisons unrelated to BS (e.g., comparing different medications without surgery). |
|
Outcome |
Primary outcome: DR (HbA1c < 6.5% without the need for antidiabetic medications). |
Studies with no data on DR, MO (e.g., insulin sensitivity), or weight loss. Studies without a clear definition of DR. |
|
Secondary outcomes: Enhancements in glycemic control (HbA1c, fasting glucose), insulin sensitivity, and weight loss. |
||
|
Study Design |
RCTs, cohort studies, and case-control studies |
Case reports, reviews, meta-analyses, and studies with unclear methodology or incomplete data. |
Data Extraction
Data extraction for this systematic review was accomplished using a standardized data extraction form by two independent reviewers to ensure consistency and accuracy. The information that was summarized based on the studies selected included the authors of the studies, the year of publication, the location of the study, and the design. Sample size, age, sex, BMI, and any comorbidities in terms of hypertension and dyslipidemia were captured. Related details about the bariatric surgical procedures were also obtained, such as the nature of the surgery compensated, follow-up period, and the overall success rate of the T2D remission. As well, glycemic control outcomes, such as changes in the level of HbA1c, fasting glucose, insulin sensitivity, and weight loss, were retrieved. Secondary outcomes data (on improvements in other elements of MS, including blood pressure, lipid profiles) were also considered. Where a difference of opinion arose between the two reviewers in the extraction process, the matter was discussed with the help of discussion. In the case that no agreement was achieved, a third reviewer was consulted to ensure that the clarity and uniformity of the data extraction process would take place.
Quality Assessment
Each study's risk of bias and overall quality were evaluated with the help of proper tools, depending on the study design. A risk of bias 2 (RoB 2) tool (Cochrane) was applied to assess the methodology of the RCTs. The aspects that this assessment assessed include the generation of random sequence, allocation concealment, blinding, completeness of outcome data, and selective reporting [18]. To assess the quality of observational studies, the Newcastle-Ottawa Scale (NOS) has been employed to evaluate the superiority of the various studies, with enrolment of subjects, comparability of subjects in the study, and the evaluation of the outcomes taken into consideration [19].
Also, funnel plots were created and checked whether they exhibit asymmetry in order to investigate the possibility of publication bias. The regression test used by Egger was utilized to investigate the existence of small-study effects. The trim-and-fill method was used to correct the outcome in situations where publication bias was observed, so that the results reflected the available evidence better [20].
Statistical Analysis
A random-effects model was also utilized to produce the data as a result of heterogeneity of participants, type of BS undergone by the participants, and the outcome of the studies included in them. Odds ratios (ORs) were used to pool effect sizes of binary outcomes (e.g., DR); mean differences (MDs) were used to pool effect sizes of continuous outcomes (e.g., changes in the HbA1c level, weight loss, and insulin sensitivity). CI was also calculated to factor in the accuracy of these estimates. A random-effects model was preferentially used because it considers study-to-study variability, giving stronger and more trustworthy results in those circumstances in which the studies are not homogeneous. The level of heterogeneity amongst studies was measured through the I statistic, with values of 0%, 25%, 50%, and 75% depicting low, moderate, and high degrees of heterogeneity. Subgroup analysis was done to find the results of the BS on the remission of diabetes; the effects of BS on the DR differed by type of surgery, the duration of the follow-up, baseline BMIs, and other aspects of patients, like their age, sex, and comorbidities. These statistical methods allowed for an inclusive understanding of the effectiveness of BS on DR in NOP with MS.
Results
Study selection
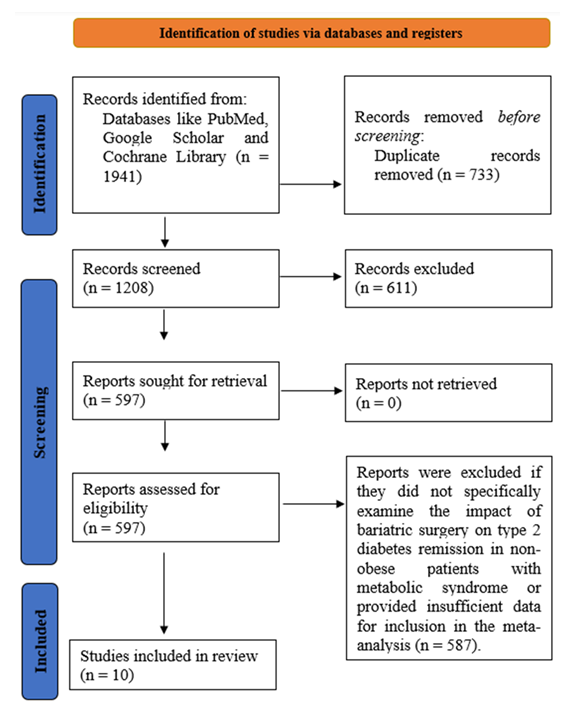
At the outset of this systematic review (meta-analysis), a total of 1941 studies were acknowledged through searches in various databases and other sources (Figure 1). After removing duplicates and articles that did not meet the suitability criteria, 1208 studies were screened for relevance. Of these, 611 studies were excluded as they did not focus on BS, T2D remission, or NOP with MS. Following a thorough full-text review, 597 studies were assessed in detail. A total of 587 studies were excluded due to not meeting the inclusion criteria, either because they did not examine BS as an intervention for T2D, lacked relevant outcomes, or did not provide the necessary data for the meta-analysis. Ultimately, 10 clinical trials that evaluated the effects of BS on DR in NOP with MS were included.
Characteristics of the included studies
The systematic review and meta-analysis included a diverse set of studies evaluating the effects of BS on T2D remission in NOP (Table 3). These studies include cohort studies, population-based studies, and RCTs. The patient populations varied, with some studies focusing on obese patients (BMI ≥ 30 kg/m²) and others on NOP (BMI < 30 kg/m²) with T2D. The most common interventions were RYGB and SG, with some studies exploring alternative procedures like duodenal switch (BPD-DS) and duodenal-jejunal bypass (DJB). Several studies also compared different surgical techniques, such as RYGB vs SG, while others explored the role of pharmacological interventions (e.g., canagliflozin) post-surgery. Primary outcomes included DR, glycemic control (HbA1c, FPG, 2hPG), weight loss, and insulin sensitivity, with some studies also incorporating metabolic markers such as incretins and adipocytokines. The follow-up durations ranged from 1 to 2 years, and most studies indicated significant improvements in DR and metabolic outcomes, especially in patients with BMI > 30 kg/m². However, some studies also identified the Visceral Adiposity Index (VAI) and predictive models like DiaBetter and DiaRem as useful tools for forecasting DR in NOP post-surgery.
Table 3: Summary of studies involved in the study
Quality assessment
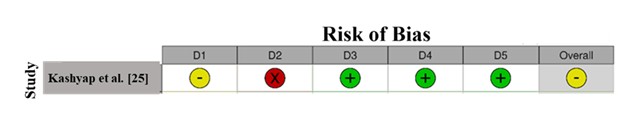
The Risk of Bias (RoB) assessment for Kashyap et al. [25] indicates a moderate risk of bias. Domain 1 (Randomization) is unclear, suggesting potential selection bias (Figure 2). Domain 2 (Deviations from Intended Interventions) shows a high risk, indicating possible performance bias due to deviations from planned interventions. However, Domains 3, 4, and 5 show low risk, reflecting proper handling of data, reliable outcome measurements, and appropriate reporting. Overall, the study’s RoB is moderate due to concerns in randomization and intervention fidelity. [31].
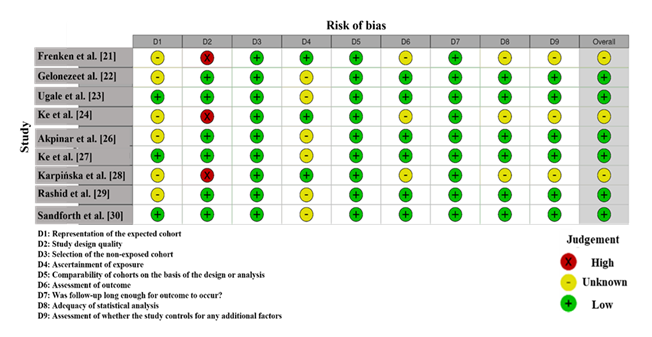
RoB assessment for the studies comprised in this meta-analysis, shown in Figure 3, reveals variability in methodological quality across the studies. Several studies, such as Frenken et al. [21], Ke et al. [24], and Karpinska et al. [28], exhibit a high risk in Domain 2 (Deviations from Intended Interventions), marked by a red "X", indicating potential performance bias due to deviations in intervention administration. Ke et al. [27] show a high risk in Domain 1 (Randomization), which could introduce selection bias due to unclear randomization processes. Studies such as Geloneze et al. [22] and Rashid et al. [29] show low risk across most domains, especially in Domain 3 (Measurement of Outcomes), Domain 4 (Incomplete Outcome Data), and Domain 5 (Selection of Reported Results), suggesting reliable data handling and outcome measurements. However, there are also studies like Akpinar et al. [26] and Sanforth et al. [30] that show an unclear risk in various domains, such as Domain 6 (Missing Outcome Data) and Domain 7 (Selective Reporting), indicating some uncertainty regarding data handling and reporting biases. Overall, studies with high or unclear risks, especially those with deviations in interventions or unclear randomization, should be interpreted with caution in the meta-analysis [32].
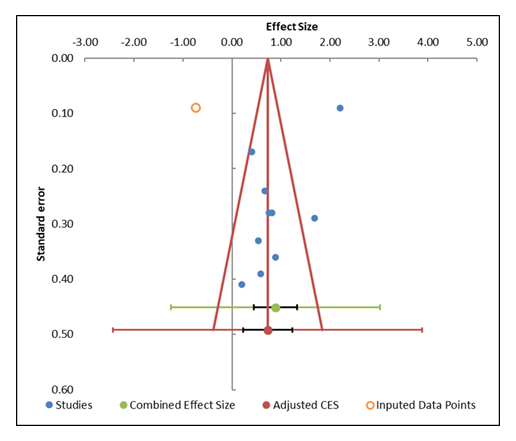
Publication Bias
The funnel plot (Figure 4) depicts a fairly symmetric distribution of the studies around the overall effect size, which indicates that there is no noteworthy publication bias that should be of concern in the presented meta-analysis. The studies on both sides of the combined effect size are distributed equally, and the small studies form the bottom of the plot, while the larger studies are at the top of the plot. This tends to be characteristic of well-dispersed data and represents the fact that smaller studies, which the more likely to be biased by publication, are not over-represented. Visual symmetry of funnel plot helps to justify that publication bias is not significant. The regression results as calculated in the Egger regression itself further enforce this reading with a p-value of 0.109 of the slope implying that there is no sign of non-significant asymmetry in study distribution. A p-value larger than 0.05 shows there is no significant difference between the slope and the zero slope, and this reinforces no publication bias of the included studies in the meta-analysis. Moreover, through the results of the trim-and-fill analysis, all studies appear to be imputable, indicating that funnel plot is balanced and contains no significant asymmetry. This also gives evidence to the fact that publication bias is unlikely a significant factor in corrupting the consequences of the present meta-analysis [33].
Table 4: Information related to funnel plot
|
Study name |
Effect Size (z) |
Standard error (z) |
|
Frenken et al. [21] |
2.2 |
0.09 |
|
Geloneze et al. [22] |
0.4 |
0.17 |
|
Ugale et al. [23] |
0.82 |
0.28 |
|
Ke et al. [24] |
1.68 |
0.29 |
|
Kashyap et al. [25] |
0.89 |
0.36 |
|
Akpinar et al [26] |
0.2 |
0.41 |
|
Ke et al. [27] |
0.54 |
0.33 |
|
Karpińska et al. [28] |
0.75 |
0.28 |
|
Rashid et al. [29] |
0.67 |
0.24 |
|
Sandforth et al. [30] |
0.59 |
0.39 |
|
Combined effect size |
Observed |
|
|
Effect size |
0.89 |
Not analyzed |
|
SE |
0.2 |
Not applicable |
|
CI Lower limit |
0.45 |
Not applicable |
|
CI Upper limit |
1.33 |
Not applicable |
|
PI Lower limit |
-1.25 |
Not applicable |
|
PI Upper limit |
3.03 |
Not applicable |
|
Heterogeneity |
Not analyzed |
|
|
Q |
550.14 |
Not analyzed |
|
pQ |
0 |
Not analyzed |
|
I2 |
98.18% |
Not applicable |
|
T2 |
1.95 |
Not applicable |
|
T |
1.4 |
Not applicable |
Table 5: Egger Regression
|
Parameter |
Estimate |
SE |
CI LL |
CI UL |
|
Intercept |
-12.62 |
7 |
-28.46 |
3.22 |
|
Slope |
13.12 |
6.79 |
-2.23 |
28.48 |
|
t test |
-1.8 |
Not applicable |
Not applicable |
Not applicable |
|
p-value |
0.109 |
Not applicable |
Not applicable |
Not applicable |
Forest plot
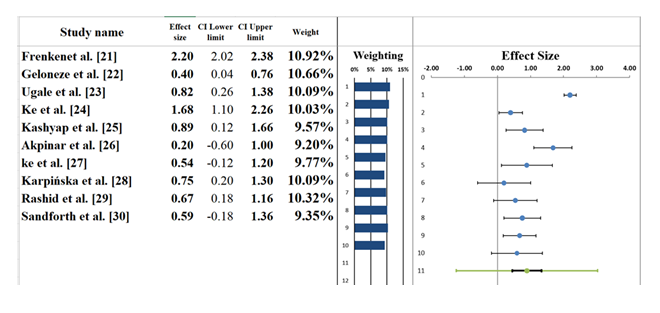
A meta-analysis of the combined effects of BS in remission of diabetes in obese and non-obese individuals can be seen in the forest plot (Figure 5). Pooled effect size across these studies was 0.89 (95% CI: 0.45 to 1.33), which showed that the positive effects of BS on diabetes-related outcomes were moderate, considering that it tends to decrease the HbA1c level and cause DR. This suggests that BS generally contributes to improved glycemic control across studies. However, the confidence interval spans from a small benefit to a more substantial one, implying some uncertainty regarding the overall impact of surgery on DR. Bariatric surgery, specifically RYGB and SG, shows varied benefits across different patient populations. Several studies, including Frenken et al. [21] and Geloneze et al. [22], report significant improvements in DR with RYGB, while others, such as Kashyap et al. [25], show more modest effects. These differences highlight that the effectiveness of BS may be influenced by factors such as patient BMI, surgical technique, and comorbid conditions. The individual studies contribute differently to the pooled effect size. For example, Frenken et al. [21] reported an effect size of 2.20 (95% CI: 2.02–2.38), indicating a strong benefit in obese patients with diabetes, while Akpinar et al. [26] showed a weaker effect size of 0.20 (95% CI: -0.60 to 1.00), suggesting minimal benefit in their population. This variation could be attributed to differences in patient demographics, the type of bariatric procedure used, and the measurement of DR. Overall, the findings suggest that BS has a significant role in achieving DR, especially in patients with higher BMI, but variability across studies highlights the need for larger, more consistent trials to refine the patient selection criteria and optimize surgical techniques for improved outcomes [34].
Table 6: Information correlated with Forest plot
|
Meta-analysis model |
|
|
Effect Size |
0.89 |
|
Standard Error |
0.2 |
|
Confidence interval LL |
0.45 |
|
Confidence interval UL |
1.33 |
|
Prediction interval LL |
-1.25 |
|
Prediction interval UL |
3.03 |
|
Z-value |
4.53 |
|
One-tailed p-value |
0 |
|
Two-tailed p-value |
0 |
|
Number of incl. subjects |
8928 |
|
Number of incl. studies |
10 |
|
Heterogeneity |
|
|
Q |
154.25 |
|
pQ |
0 |
|
I2 |
94.17% |
|
T2 (z) |
0.85 |
|
T (z) |
0.92 |
Heterogeneity Assessment
The heterogeneity assessment based on the forest plot (Table 6) reveals considerable variability across the studies included in this meta-analysis. The I² statistic is 94.77%, suggesting that a significant proportion of the variation in effect sizes is due to true differences between the studies rather than random chance. This high level of heterogeneity indicates substantial diversity in the studies, likely driven by variations in patient characteristics, surgical techniques, study designs, and follow-up durations. The p-value recorded is 0.000, proving that Q- Q-statistic = 154.25 is indeed significant. This finding strengthens the idea that the variation in the study results is not an outcome related to random chance, but rather an outcome related to actual deviation in the studies. The T2 of 1.25 also confirms the existence of considerable variation in the treatment results, with the factors contributing to such variation being the sample size, demographic factors, type of BS that is conducted, and variation in the patient's health status. Although the pooled effect size indicates that BS has positive implications on remission in diabetes cases, the heterogeneity is high; therefore, the results of the studies should be interpreted with consideration of confounding factors like the types of surgical procedures, patients' BMI and comorbid conditions (e.g. obesity, MS). These are the sources of the variation and they should be considered to come to a clearer idea about the real effectiveness of BS as one of the ways of DR. [35].
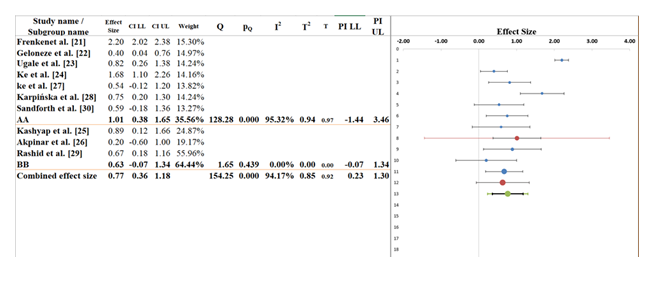
Subgroup analysis
Figure 6 displays the subgroup analysis that focuses on how effect sizes vary across two different groups (AA and BB) to know how BS differs in the remission of diabetes. The pooled effect indicating moderate positive effect of BS on remission of diabetes stands at 0.77 (95 percentage CI: 0.36 to 1.18). The confidence interval makes some uncertainty, but it shows that the BS procedure is more likely to bring positive results. The I2 value (94.17) demonstrates substantial heterogeneity implying a wide range of differences among studies with the reason being aspects such as the study design/ patient demographics/ surgical procedures. In the subgroup AA, effect size is 1.01 (95 percent CI: 0.38 to 1.65) and there is a moderate positive impact of surgery. But the large amount of confidence interval indicates that there is no certainty about the degree of the effect. With I that is equal to 95.32 percent, the value shows high variability, which could be caused by the disparities in patient demographics, surgical methods, and other criteria. This points out to the fact that more studies are required to gain a proper insight of the efficacy of BS in this subgroup [36].
The effect size is smaller, 0.63 (95% CI: -0.07 to 1.34) in the case of subgroup BB (Table 7). The confidence interval is broad and attributable to the probability of no effect, and the I2 is 0.00%, so there is no variability in the effect sizes within this group. Although this implies that more consistency in the findings was achieved in the case of BB, it is also evident that there was a broad confidence interval, indicating the necessity of additional data to determine the actual effect. The results demonstrate that the effect sizes between subgroups AA and BB are statistically significant (Q-statistic between groups = 128.28, p = 0.000), which means that the subgroups differ based on the modification of CWCs. This implies that the treatment effect of BS varies significantly between these two subgroups, which may be because of the varied characteristics of patients, methods of surgery, and methodology of the studies. Even though the result of the subgroup analysis suggests that there is a positive effect of BS on DR, variation among studies is quite high. Heterogeneity of the first subgroup AA is strong, and the explanation of such outcome may feature surgical procedure and patient selection since the former might lead to different results, and the latter contributes to the outcome variability. Thus, subgroup BB demonstrates consistent results, yet they can be more detailed with further study of that effect to improve it. [37]. The discrepancy in heterogeneity, with an overall I² of 94.17% and I² of 0% in subgroup BB, can be explained by the fact that while the studies in subgroup BB showed consistent effect sizes, the wide confidence intervals indicate uncertainty, and the overall heterogeneity is driven by variability in other subgroups.
Table 7: Information related to Sub-group analysis
|
Meta-analysis model |
||
|
Effect size |
0.77 |
|
|
Standard Error |
0.18 |
|
|
Confidence interval LL |
0.36 |
|
|
Confidence interval UL |
1.18 |
|
|
Prediction interval LL |
0.23 |
|
|
Prediction interval UL |
1.3 |
|
|
Number of incl. subjects |
4774 |
|
|
Number of subgroups |
2 |
|
|
Analysis of variance |
|
|
|
Between / Model (Q*) |
0.8 |
|
|
Between / Model (Df) |
1 |
|
|
Between / Model (P) |
0.371 |
|
|
Within / Residual (Q*) |
4.45 |
|
|
Within / Residual (Df) |
8 |
|
|
Within / Residual (P) |
0.815 |
|
|
Total (Q*) |
5.25 |
|
|
Total (Df) |
9 |
|
|
Total (P) |
0.812 |
|
|
Pseudo R2 |
15.26% |
|
Narrative analysis
Bariatric Surgery and Diabetes Remission Outcomes: All the studies used in this systematic review report a high level of effectiveness of the use of BS in ensuring the remission of diabetes among obese individuals and non-obese with T2D. As seen in research led by Frenken et al. [21] and Geloneze et al. [22], the effective outcomes of both RYGB and SG are the reduction in the HbA1c level and the irrelevance of diabetes medication. Yet, the effect is also different with patients with BMI > 30 kg/m 2 showing greater improvement, as it is evident in Ke et al. [24], although those of NOP have more modest results as reported by Ke et al. [27] as well.
Impact of Patient Characteristics on Outcomes: BS seems to be affected by different patient attributes, including BMI, age, and comorbidities. Researchers such as Kashyap et al. [25] discovered that BS contributes to substantial weight loss and glycemic control in patients affected with obesity. Ke et al. [27] and Karpinska et al. [28], in contrast, emphasise that NOP have more unstable results, which is why selecting patients should be improved. VAI, as indicated by Ke et al. [27], is also an effective predictor to determine the presence of NOP who will potentially benefit from the surgery.
Safety and Long-Term Feasibility: BS is generally safe in both obese and non-obese patients with T2D, with low adverse event rates reported among the studies. According to Akpinar et al. [26] and Sanforth et al. [30], proper selection of patients should particularly take comorbidities like hypertension and dyslipidemia into consideration in order to derive the benefits of the surgery. Nevertheless, the necessity of the long-term follow-up may be emphasized as the data regarding the sustainability of surgery performance, in particular, among non-obese people, remains limited, and long-term observation is critical.
Variability in Outcomes and Study Findings: The results of the studies included in this review pose a certain degree of fluctuation regarding the success of BS in existing diabetes, and this issue is mainly connected to differences in the design of the research, procedure, and specific demographics. Indicatively, the findings in studies such as Kashyap et al. [25], Geloneze et al. [22] involving huge gains in insulin sensitivity and weight loss, as compared to others such as Akpinar et al. [26], who indicate modest improvements. Such a discrepancy highlights the necessity of more standardized approaches to increase the repeatability of the outcomes and suggestions when it comes to BS as an intervention in treating T2D.
Discussion
The systematic review and meta-analysis presented in this study are crucial to determining the remission of diabetes with BS in non-obese and obese patients with T2D. The findings of the different studies illustrate that BS and specifically RYGB and SG have an immense effect of enhancing the levels of HbA1c. This is coherent with the report of Frenken et al. [21] and Geloneze et al. [22], who also considered that glycemic control showed significant improvements in obese individuals after receiving bariatric surgery. In non-obese patients, however, the effects are less dramatic, with, e.g., HbA1c reductions and increases to insulin sensitivity being moderate but still statistically significant, such as in Ke et al. [27].
The character of patients, primarily in terms of BMI and comorbidity, is one of the most important reasons that determine the success of bariatric surgery. Literature findings like those by Kashyap et al. [25] and Ke et al. [24] indicate that obese patients experience a lot of weight loss and enhancement of glycemic control, which correlates with ours. Conversely, Ke et al. [27] and Karpinska et al. [28] reveal that outcomes are more variable in NOP, indicating that their treatment outcomes could not be as profound as those of obese patients. This inconsistent result further supports the idea that better patient selection should be done and that parameters such as VAI may be useful in determining which NOP will most likely respond to surgery [38,39].
The heterogeneity of results found in the studies means that the results mostly vary, and therefore, it can be concluded that the success of BS in bringing remission to diabetes could be offset by factors like the surgical technique, demographical characteristics of the patient, and comorbid factors. The current findings support the works of Kashyap et al. [25] explaining why there should be standardized criteria in BS to reduce variability. It can also be explained by the large heterogeneity, and possibly that, depending on the type of patients, the effects of BS may greatly differ, and that more homogenized methods and extended follow-ups are needed to properly devise treatment protocols and secure necessary outcomes [40].
Altogether, this review validates the moderate positive outcome of BS on DR, especially in obese people, but reinforces the need for additional research dedicated to discussing the factors impacting the variability, especially among non-obese subjects. Patient selection criteria, surgical methodologies, and follow-up times to be used will need to be standardized, which is important to maximize the outcome and enhance the reliability of the research results between future studies.
Limitations
Despite the promising findings, this systematic review and meta-analysis have several limitations. First, there is significant heterogeneity (I² = 94.77%) across the included studies, indicating that factors such as patient demographics, surgical techniques, and follow-up durations likely contribute to variability in the results. This high variability makes it challenging to generalize the findings to all patient populations and surgical procedures. Furthermore, many of the studies included were retrospective cohort studies or observational studies, which are more susceptible to bias compared to RCTs. The lack of RCTs limits the ability to draw causal inferences and may introduce confounding factors. Another limitation is the inconsistent reporting of outcomes across studies. Some studies focused on HbA1c levels, while others reported DR differently, making it difficult to compare results directly. Additionally, NOP exhibited more variable outcomes, and while factors like VAI have been proposed as predictors, further research is needed to validate these markers in non-obese populations. Lastly, the long-term follow-up data for NOP remain limited, which hinders the assessment of the sustainability of DR post-surgery, making it challenging to evaluate the lasting effects of BS in these individuals.
Future Research
Future studies need to concern themselves with the sizeable heterogeneity found in the current meta-analysis and especially by harmonising the criteria being used to select patients, methods of surgical intervention, and follow-ups. This would make it easier to minimize the variability between studies and give better, more consistent results. In particular, the current state of research requires RCTs that could offer higher-quality evidence since most of the existing studies are retrospective and observational and more vulnerable to bias. More robust causal inferences could be made about the causal effects of BS on remission of diabetes with RCTs. Also, there is a need to study more predictive markers like VAI, especially in identifying which non-obesity patients are likely to respond better to bariatric surgery. The long-term results of the follow-up are also important in the evaluation of long-term diabetes sustainability after the surgery, especially in non-obese patients, whose recovery was more inconsistent in the reviewed literature. Finally, prospective studies that aim at deepening the previously noted causes of DR, like insulin sensitivity and gut hormones, would be of great value. Studying these mechanisms may also contribute to more specific interventions and the concept of BS as a means of controlling T2D.
Conclusions
To sum it up, it is confirmed in this systematic review and meta-analysis that BS influences the remission of diabetes in patients with T2D positively and significantly in those with obesity. The overall effect size shows a medium-sized advantage in the increased HbA1c levels enhancement and diminished application of diabetes medications after surgery. The findings are also in line with the results of the past studies. But it should be noted in the review that the results of BS in NOP are less consistent, and poor improvements in HbA1c and insulin sensitivities are observed. The present level of variability highlights the significance of taking into account the characteristics of patients, namely BMI, VAI, co-morbidities, and their presence in predicting the appropriateness of bariatric surgery. The procedure yields no significant results for the patients who are not obese, as it does for obese patients, though they benefit. The positive results in spite of this were accompanied by high heterogeneity among the studies, which indicates that factors like surgical technique, follow-up period, and patient selection, among others, help to explain the variability in the results. It is also not able to come up with strong causal conclusions due to the absence of RCTs in the body of literature. Summarily, BS presents an excellent method of achieving DR, although standardisation is essential by conducting more studies to improve how the process is done, patient selection, and long-term consequences, particularly in the non-obese group.
References
- Wolfe BM, Kvach E, Eckel RHJCr: Treatment of obesity: weight loss and bariatric surgery 118 (2016): 1844-1855.
- Nguyen NT, Varela JEJNrG, hepatology: Bariatric surgery for obesity and metabolic disorders: state of the art 14 (2017): 160-169.
- Pareek M, Schauer PR, Kaplan LM, et al DLJJotACoC: Metabolic surgery: weight loss, diabetes, and beyond 71 (2018): 670-687.
- Dhondge RH, Agrawal S, Patil R, et al: A comprehensive review of metabolic syndrome and its role in cardiovascular disease and type 2 diabetes mellitus: mechanisms, risk factors, and management 16 (2024).
- Wu Y, Li D, Vermund SHJIjoer, Health P: Advantages and limitations of the body mass index (BMI) to assess adult obesity 21 (2024): 757.
- Soliman RH, Farhan HM, Hegazy M, et al.: Impact of insulin resistance and metabolic syndrome on disability in patients with multiple sclerosis 56 (2020): 18.
- Koliaki C, Liatis S, Le Roux CW, et al: The role of bariatric surgery to treat diabetes: current challenges and perspectives 17 (2017): 50.
- Wang G-F, Yan Y-X, Xu N, et al.: Predictive factors of type 2 diabetes mellitus remission following bariatric surgery: a meta-analysis 25 (2015): 199-208.
- Kim WS, Choi Y, Kim N, et al.: Long-term effect of the eradication of Helicobacter pylori on the hemoglobin A1c in type 2 diabetes or prediabetes patients 37 (2022): 579.
- Arterburn DE, Telem DA, Kushner RF, et al: Benefits and risks of bariatric surgery in adults: a review 324 (2020): 879-887.
- Alqunai MS, Alrashid FFJAJoTR: Bariatric surgery for the management of type 2 diabetes mellitus-current trends and challenges: a review article 14 (2022): 1160.
- Alghamdi MMA: Oral inflammatory load and salivary flow rate in morbidly obese patients: relationship with diabetes and effect of bariatric care protocol. University of Toronto (Canada), (2018).
- Kermansaravi M, Chiappetta S, Kassir R, et al.: Efficacy of one anastomosis gastric bypass versus sleeve gastrectomy and Roux-en-Y gastric bypass for the treatment of type 2 diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials 34 (2024): 4555-4562.
- Musella M, Apers J, Rheinwalt K, et al.: Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey 26 (2016): 933-940.
- Catalano PM, Shankar KJB: Obesity and pregnancy: mechanisms of short-term and long-term adverse consequences for mother and child 356 (2017).
- Frühbeck GJNRE: Bariatric and metabolic surgery: a shift in eligibility and success criteria 11 (2015): 465-477.
- Vasdeki D, Koufakis T, Tsamos G, et al: Remission as an emerging therapeutic target in type 2 diabetes in the era of new glucose-lowering agents: benefits, challenges, and treatment approaches 14 (2022): 4801.
- Nejadghaderi SA, Balibegloo M, Rezaei NJHSR: The Cochrane risk of bias assessment tool 2 (RoB 2) versus the original RoB: A perspective on the pros and cons 7 (2024): e2165.
- Luchini C, Stubbs B, Solmi M, et al: Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale 5 (2017): 80-84.
- Doleman B, Freeman SC, Lund JN, et al: Funnel plots may show asymmetry in the absence of publication bias with continuous outcomes dependent on baseline risk: presentation of a new publication bias test 11 (2020): 522-534.
- Frenken M, Cho E-Y, Karcz WK, et al: Improvement of Type 2 Diabetes Mellitus in Obese and Non-Obese Patients after the Duodenal Switch Operation (2011): 860169.
- Geloneze B, Geloneze SR, Chaim E, et al.: Metabolic surgery for non-obese type 2 diabetes: incretins, adipocytokines, and insulin secretion/resistance changes in a 1-year interventional clinical controlled study 256 (2012): 72-78.
- Ugale S, Gupta N, Modi KD, et al.: Prediction of remission after metabolic surgery using a novel scoring system in type 2 diabetes–a retrospective cohort study 13 (2014): 89.
- Ke Z, Li F, Chen J, et al.: Effects of laparoscopic Roux-en-Y gastric bypass for type 2 diabetes mellitus: comparison of BMI> 30 and< 30 kg/m2 27 (2017): 3040-3047.
- Kashyap SR, Kheniser K, Aminian A, et al.: Double-blinded, randomized, and controlled study on the effects of canagliflozin after bariatric surgery: A pilot study 6 (2020): 255-263.
- Akpinar EO, Liem RS, Nienhuijs SW, et al.: Metabolic effects of bariatric surgery on patients with type 2 diabetes: a population-based study 17 (2021): 1349-1358.
- Ke Z, Li F, Gao Y, et al.: The use of visceral adiposity index to predict diabetes remission in low BMI Chinese patients after bariatric surgery 31 (2021): 805-812.
- Karpińska IA, Choma J, Wysocki M, et al.: External validation of predictive scores for diabetes remission after metabolic surgery 407 (2022): 131-141.
- Rashid M, Al Qarni A, Al Mahri S, et al.: Transcriptome changes and metabolic outcomes after bariatric surgery in adults with obesity and type 2 diabetes 8(2024): 8:bvad159.
- Sandforth L, Raverdy V, Sandforth A, et al.: Subphenotype-Dependent Benefits of Bariatric Surgery for Individuals at Risk for Type 2 Diabetes 48 (2025): 996-1006.
- Flemyng E, Moore TH, Boutron I, et al.: Using Risk of Bias 2 to assess results from randomised controlled trials: guidance from Cochrane 28 (2023): 260-266.
- Moskalewicz A, Oremus MJJoce: No clear choice between Newcastle–Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer 120 (2020): 94-103.
- Lin LJRsm: Graphical augmentations to sample-size-based funnel plot in meta-analysis 10 (2019): 376-388.
- Andrade CJTJocp: Understanding the basics of meta-analysis and how to read a forest plot: as simple as it gets 81 (2020): 21858.
- Sedgwick PJB: Meta-analyses: what is heterogeneity? 350 (2015).
- Wang X, Piantadosi S, Le-Rademacher J, et al: Statistical considerations for subgroup analyses 16 (2021): 375-380.
- Lipkovich I, Dmitrienko A, B D'Agostino Sr RJSim: Tutorial in biostatistics: data-driven subgroup identification and analysis in clinical trials 36 (2017): 136-196.
- Panunzi S, Carlsson L, De Gaetano A, et al.: Determinants of diabetes remission and glycemic control after bariatric surgery 39 (2016): 166-174.
- Napoleão A, Fernandes L, Miranda C, Marum APJN: Effects of calorie restriction on health span and insulin resistance: Classic calorie restriction diet vs. ketosis-inducing diet 13 (2021): 1302.
- Aderinto N, Olatunji G, Kokori E, et al.: Recent advances in bariatric surgery: a narrative review of weight loss procedures 85 (2023): 6091-6104.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 