How Residents MET their Training: Resident’s Perception of Medical Emergency Team and its Contribution to their Training
Kangqi Ng1*, Jia Wen Kam2, Daryl Jones3, Augustine Tee4
1Consultant, General Medicine, Changi General Hospital, Singapore
2Biostatistician, Singapore
3Consultant Intensive Care specialist, Austin Health, Adjunct Professor, SPHPM, Monash University, Victoria, Australia
4Senior Consultant, Respiratory and critical care medicine, Changi General Hospital, Singapore
*Corresponding author: Kangqi Ng, Consultant, General Medicine, Changi General Hospital, 2 Simei Street 3, Changi City, 529889, Singapore
Received: 11 February 2022; Accepted: 21 February 2022; Published: 04 March 2022
Article Information
Citation:
Kangqi Ng, Jia Wen Kam, Daryl Jones, Augustine Tee. How Residents MET their Training: Resident’s Perception of Medical Emergency Team and its Contribution to their Training. Archives of Internal Medicine Research 5 (2022): 077-090.
View / Download Pdf Share at FacebookAbstract
Background: Medical Emergency Teams (MET) have been implemented in many hospitals to improve patient safety. Few studies examined how residents perceive the MET as part of training.
Objective: We aimed to evaluate residents’ perceptions of how MET rotation affected training in the core competencies specified by Accreditation Council for Graduate Medical Education (ACGME).
Methods: We conducted an online survey of 106 res- idents. They are either junior residents who are in training in internal medicine, non-trainee registrars or senior residents who are training in respiratory or advanced internal medicine.
Results: We achieved a response rate of 62.3%. More than 90% of residents agreed or strongly agreed that MET contributed positively to their training, made resuscitation of patients safer and more efficient, and disagreed or strongly disagreed that MET made resuscitation of patients more time-consuming or cumbersome. More than 80% agreed or strongly agreed that the MET improved their clinical judgement in medical emergencies, helped achieve their learning goals and exposed them to a wide variety of cases. At least two-thirds thought that the MET posting improved their procedural skills and communication in end of life care discussions. In contrast, 26.6% of respondents agreed or strongly agreed that the MET decreased autonomy of the primary team. One-third felt they needed formal training for the MET posting.
Conclusion: Our findings suggest that residents perceive participation in MET was beneficial in training and improved patient care. We also found that formal training and consultant oversight may be needed for junior team leaders of MET
Keywords
<p>Medical Emergency Teams (MET), Rapid Response Systems (RRS)</p>
Article Details
1. Introduction
Medical Emergency Teams (MET) exists in many hospitals in developed countries as part of Rapid Response Systems (RRS). It has been shown in meta-analysis and cohort studies that RRS are associated with reduced rates of unplanned cardiorespiratory arrests outside of intensive care units, as well as reduced in-hospital mortality [1-3]. The term MET implies that the responding team is physician led. Few studies have examined how residents perceive the MET as part of their training. Jacques and co-workers studied intensive care registrars and their attitude and evaluation of the MET and found that the majority felt it enhanced the quality of their training [4]. Benin also qualitatively described the experiences and attitudes held by nurses, physicians and admin-istrators regarding MET and concluded that MET is a good educational tool for junior doctors and nurses. However, MET may also be detrimental to their edu-cation as the independent decision-making process of primary team doctors can be compromised in an eff-ort to expedite care for deteriorating patients. In this aspect, the traditional teaching approach to medical management in acutely ill patients was super-ceded by placing patient outcome as a priority [5]. In cont-rast, other studies showed that ward residents agreed that their work with MET was a valuable educational experience and improved patient safety [6-7].
The MET in Changi General Hospital (CGH) is led by a non-trainee registrar or senior resident who is undergoing training in either internal medicine (IM), respiratory medicine or intensive care medicine. They are directly involved in leading or carrying out evalu-ation and resuscitative procedures. The training prog-ram for all hospital residents involves attaining core competencies in several domains. The aim of this study was to evaluate MET residents’ perceptions of the utility of MET in contribution to their training. To achieve this, we conducted a survey of physicians who had completed a MET rotation to evaluate their perceptions of this role in contributing to the core competencies of the resident’s training program.
2. Methodology
2.1 Ethics approval
Approval was obtained for the conduct of the survey (Approval number 2017/2858). Participation in the survey was anonymous and voluntary and willingne-ss to complete the survey was taken as an indication of consent.
2.2 Study setting
The study was conducted in Changi General Hospital
(CGH), situated in eastern Singapore, serving a population of about 1 million. It has approximately 1000 beds and is a major accredited teaching hospital with the SingHealth Residency Programme. As a tertiary hospital, it has a complement of specialities, except for pediatrics, obstetrics and gynaecology, cardiothoracic surgery and transplant.
2.3 The MET in CGH
We implemented a MET system in our hospital in 2009, where it was physician-led and complemented with critical care trained nurses and respiratory therapists. The CGH MET was a maturing rapid response system with about 17 activations per 1000 admissions in 2016. Our MET activation criteria is summarized in Table 1 and is similar to MET activation criteria elsewhere [8].
2.4 Role of residents in the hospital MET
The residents whom we surveyed in this study were either in the Internal Medicine junior or senior residency, Respiratory Medicine senior residency or non-trainee registrars (fellow equivalent with post-graduate degree in internal medicine). We do not have a dedicated critical care residency programme. Therefore, our study examined a heterogeneous group of trainees who were at different stages in their training. The senior residents and non-trainee regis-trars led MET activations, with a locally accredited intensivist providing supervision and a MET comm-ittee responsible for oversight. This was similar to the MET model in Australia and New Zealand though the role of a physician was also variable [9, 10]. Other members of the MET include junior resid-ent(s), a respiratory therapist and a trained intensive care unit (ICU) nurse. Junior residents doing their ICU rotation as part of Internal Medicine residency assisted the MET registrar as part of the MET. Other junior residents that were present belonged to the primary or parent team, and took orders from the MET. The latter were not surveyed.
2.5 Development and implementation of the survey
The survey was conducted amongst residents who were posted to CGH medical intensive care unit over a period of 3 years from year 2013 to 2016 after these residents have completed their rotation to the MET. The survey contained questions based on the 6 core competencies of the residency programme. These core competencies were according to those identified by ACGME (Accreditation Council for Graduate Medical Education) [11] and include 1) patient care and procedural skills, 2) medical knowledge, 3) practice-based learning and improvement, 4) inter-personal and communication skills, 5) profession-alism and 6) systems-based practice (Appendix; Table A). The questions aimed to evaluate the resid-ents’ perceptions of how a rotation in the MET affected training in the core competencies and whether it helped to fulfil each of them. There were also general questions to determine a resident’s overall perception of MET. The survey was condu-cted using principles published elsewhere [12].
2.6 Data collection and survey format
We conducted the survey using an online survey tool that was sent to every resident via email (Appendix). The residents were not interviewed face to face. No personally identifiable data were collected. However, to enable better analysis of MET in relation to trai-ning stages, residents answered questions regarding which residency program and which postgraduate year they were in. Responses were obtained using a five-level Likert scale with 1 being "strongly disa-gree" and 5 "strongly agree". All completed and partially completed surveys were analysed by a research assistant. The survey was facilitated by members of the MET team with interest in evaluating resident’s perception regarding MET as a training tool. Categorical data was presented as frequency (percentage). Likert scale data was presented as median (interquartile range). Mann-Whitney test was used for between 2-group comparisons and Kruskal-Wallis test was used for more than 2-group com-parison. In case of statistically significant difference in Kruskal-Wallis test, Bonferroni post hoc adjust-ment was used for multiple pairwise comparesons. We performed statistical analysis with SPSS stati-stical software, version 19.0 (IBM Corp. Armonk, NY). A two-sided, p-value of < 0.05 was taken to indicate statistical significance. We compared the perceptions of the different residency programs, postgraduate years 1-3, 4-6 or 7 and gender.
|
System |
Detailed Description |
|
Airway |
If threatened i.e. noisy breathing, stridor or wheeze |
|
Breathing |
Acute change in respiratory rate <8 or >30 breath per minute |
|
Acute change in pulse oximetry to <90% despite oxygen administration |
|
|
Oxygen requirements of FiO2 50% or greater |
|
|
Circulation |
Acute change in heart rate to <40 or >130 beats per minute |
|
Acute change in systolic blood pressure <90 mmHg |
|
|
Neurology |
Acute change in mental status (fall of Glasgow coma scale >2 points) |
|
Others |
Any patient that a staff member (doctor, nurse, allied health) is seriously worried about that does not fit the above criteria |
Table 1: MET calling criteria.
3. Results
3.1 Sample frame and survey response rate
A total of 106 residents were posted to MET over a period of 3 years. The study survey was distributed to all 106 respondents, of which 66 submitted their responses (response rate 62.3%).
3.2 Demographics of residents
Out of the 66 respondents, 24 (36.4%) were junior residents and 42 (63.6%) were registrars or senior residents; 15.2% of the respondents were in postgraduate years 1 to 3, 39.4% postgraduate years 4 to 6, and 45.5% were in postgraduate years 7 or more. Of the 66 respondents, 60.6% were female.
3.3 General questions related to the MET posting overall
More than 90% of residents agreed or strongly agreed that MET contributed positively to patient care and their training; made resuscitation of patients safer and more efficient; and disagreed or strongly disagreed that MET made resuscitation of patients more time-consuming or cumbersome (Table 2).
3.4 Questions related to patient care and procedural skills
Eighty two percent of respondents agreed or strongly agreed that the posting in the MET improved their clinical judgement in medical emergencies, and 70% thought that it improved their procedural skills (Table 3). Questions relating to clinical autonomy of the primary team and involvement of clinical supervisors were more varied and 37% strongly disagreed or disagreed that MET has decreased clinical autonomy of primary team. About one fifth of residents felt MET activations involved complex medical emergencies that frequently required their super-visor’s intervention (Table 3).
3.5 Questions related to medical knowledge
Almost 85% of respondents agreed or strongly agreed that the MET posting exposed them to a wide variety of clinical cases. 18% agreed or strongly agreed that they felt they were equipped to resolve disputes amongst clinicians that arose during MET active-tions, compared to 40% who disagreed or strongly disagreed, with a similar proportion being neutral in their response to this question (Table 3). There was varied level of agreement in relation to the perceived need for formal training and assessment in relation to the MET posting, with approximately one third agreeing, one third neutral and one third disagreeing with this question (Table 3).
3.6 Questions related to practice-based learning and improvement
Almost three-quarters of respondents disagreed or strongly disagreed that MET activations exposed their weaknesses, and 86% agreed or strongly agreed that the MET posting helped them achieve their learning goals. Responses were varied when partici-pants were asked whether they were able to assume a teaching role during the MET posting with 40.6% being neutral in this response (Table 4).
3.7 Questions related to interpersonal and communication skills
Residents infrequently (1.7%) agreed that they have differing opinions from the respiratory therapists, especially regarding non-invasive ventilation. In addition, more than two-thirds agreed or strongly agreed that through the MET posting they learnt to communicate with family particularly regarding end of life care issues (Table 4).
3.8 Questions relating to professionalism
The MET posting appeared to contribute positively to professionalism. Approximately three-quarters of participants agreed or strongly agreed that the MET exposed them to various patient populations and the importance of patient autonomy and shared decision making. In addition, approximately two-thirds thoug-ht that the MET taught them regarding the influence of family in patients’ decision making (Table 4).
3.9 Questions about systems-based practice
The MET posting appeared to contribute very positively toward elements of systems based practice. Thus, four out of five respondents agreed or strongly agreed that the MET posting taught the importance of coordination of health care to ensure the best possible patient outcomes, and 95% learnt how having a rapid response team can help improve patient outcome (Table 5).
|
Overall |
SD |
D |
N |
A |
SA |
Median (IQR) |
|
Overall, I feel MET contributed positively to patient care N =57 n(%) |
0 (0.0) |
0 (0.0) |
1 (1.8) |
31 (54.4) |
25 (43.4) |
4 (4-5) |
|
Overall, I feel MET posting contributed positively to my training N =57 n(%) |
0 (0.0) |
0 (0.0) |
6 (10.5) |
28 (49.1) |
23 (40.4) |
4 (4-5) |
|
Overall, regarding resuscitation of patients, MET activations made it more cumbersome N =57 n(%) |
19 (33.3) |
32 (56.1) |
5 (8.8) |
1 (1.8) |
0 (0.0) |
2 (1-2) |
|
Overall, regarding resuscitation of patients, MET activations made it more time-consuming. N =57 n(%) |
19 (33.3) |
33 (57.9) |
4 (7.0) |
1 (1.8) |
0 (0.0) |
2 (1-2) |
|
Overall, regarding resuscitation of patients, MET activations made it more efficient N =57 n(%) |
0 (0.0) |
0 (0.0) |
3 (5.3) |
29 (50.9) |
25 (43.9) |
4 (4-5) |
|
Overall, regarding resuscitation of patients, MET activations made it safer. N =57 n(%) |
0 (0.0) |
0 (0.0) |
2 (3.5) |
28 (49.1) |
27 (47.4) |
4 (4-5) |
SD = strongly disagree, D = disagree, N = neutral, A = agree, SA = strongly agree
Table 2: Overall questions related to perceptions of the MET.
|
Survey Questions |
SD |
D |
N |
A |
SA |
Median (IQR) |
|
Patient Care & Procedural Skills |
||||||
|
The posting in MET improved my clinical judgement in medical emergencies N = 61 n(%) |
1 (1.6) |
1 (1.6) |
9 (14.8) |
26 (42.6) |
24 (39.3) |
4 (4-5) |
|
The posting improved my procedural skills eg intubation, Central Venous Pressure line setting, Intra-Arterial line setting N = 61 n(%) |
1 (1.6) |
3 (4.9) |
14 (23.0) |
21 (34.4) |
22 (36.0) |
4 (3-5) |
|
I feel that MET posting has decreased clinical autonomy of the primary team N =61 n(%) |
7 (11.5) |
16 (26.2) |
22 (36.0) |
14 (23.0) |
2 (3.3) |
3 (2-4) |
|
Met activations involved complex medical emergencies that frequently required my supervisor's intervention N =61 n(%) |
2 (3.3) |
17 (27.9) |
30 (49.2) |
10 (16.4) |
3 (4.9) |
3 (2-3) |
|
Medical Knowledge |
||||||
|
I do not feel that I am equipped to resolve disputes among clinicians that arose during met activations N = 59 n(%) |
1 (1.7) |
23 (39.0) |
24 (40.7) |
9 (15.3) |
2 (3.4) |
3 (2-3) |
|
I feel that we need a have formal training before MET posting and a formative assessment during/after MET posting N =59 n(%) |
4 (6.8) |
19 (32.2) |
16 (27.1) |
19 (32.2) |
1 (1.7) |
3 (2-4) |
|
MET posting has exposed me to a wide variety of clinical cases. N=59 n(%) |
0 (0.0) |
1 (1.7) |
8 (13.6) |
33 (55.9) |
17 (28.8) |
4 (4-5) |
SD = strongly disagree, D = disagree, N = neutral, A = agree, SA = strongly agree
Table 3: Survey questions and responses in the domains of patient care and procedural skills, as well as medical knowledge.
|
Survey Questions |
SD |
D |
N |
A |
SA |
Median (IQR) |
|
Practice-based Learning & Improvement |
||||||
|
I was uncomfortable with MET activations as it exposed my weaknesses. N = 59 n(%) |
11 (18.6) |
32 (54.2) |
12 (20.3) |
4 (6.8) |
0 (0.0) |
2 (2-3) |
|
The MET posting helped me achieve my learning goals. N = 59 n(%) |
0 (0.0) |
1 (1.7) |
7 (11.9) |
35 (59.3) |
16 (27.1) |
4 (4-5) |
|
I was able to assume a teaching role during the MET posting. N = 59 n(%) |
2 (3.4) |
15 (25.4) |
24 (40.7) |
16 (27.1) |
2 (3.4) |
3 (2-4) |
|
Interpersonal & Communication Skills |
||||||
|
I tend to have differing opinions from the respiratory therapists in the team especially regarding non-invasive ventilation. N = 59 n(%) |
13 (22.0) |
37 (62.7) |
8 (13.6) |
1 (1.7) |
0 (0.0) |
2 (2-2) |
|
Through the MET posting, I learnt to communicate with family particularly regarding end of life issues N = 59 n(%) |
0 (0.0) |
4 (6.8) |
14 (23.7) |
31 (52.5) |
10 (16.9) |
4 (3-4) |
|
Professionalism |
||||||
|
MET exposed me to various patient populations such as medical patients with acute surgical conditions or surgical patients with acute medical conditions. N =57 n(%) |
0 (0.0) |
3 (5.3) |
11 (19.3) |
33 (57.9) |
10 (17.5) |
4 (3.5-4) |
|
MET taught me the importance of patient autonomy and shared decision making with primary team doctors and nurses. N =57 n(%) |
0 (0.0) |
2 (3.5) |
13 (22.8) |
30 (52.6) |
12 (21.0) |
4 (3-4) |
|
MET taught me the influence family has in a patient’s decision making. N =57 n(%) |
0 (0.0) |
1 (1.8) |
17 (29.8) |
29 (50.9) |
10 (17.5) |
4 (3-4) |
SD = strongly disagree, D = disagree, N = neutral, A = agree, SA = strongly agree
Table 4: Survey questions and responses in the domains of Practice-based learning and improvement, interpersonal and communication skills, as well as professionalism.
|
Survey Questions |
SD |
D |
N |
A |
SA |
Median (IQR) |
|
Systems Based Practice |
||||||
|
Through MET posting, I learnt the importance of working with various departments and need for coordinating healthcare to ensure best outcome for patient eg dialysis planning N = 57 n(%) |
0 (0.0) |
2 (3.5) |
10 (17.5) |
31 (54.4) |
14 (24.6) |
4 (4-4.75) |
|
Through the MET posting, I learnt how having a rapid response team can help to improve patient care N =57 n(%) |
0 (0.0) |
0 (0.0) |
3 (5.3) |
24 (42.1) |
30 (52.6) |
5 (4-5) |
SD = strongly disagree, D = disagree, N = neutral, A = agree, SA = strongly agree
Table 5: Survey questions and responses in the domain of Systems Based Practice.
3.10 Comparison of respondent’s perceptions according to level of seniority
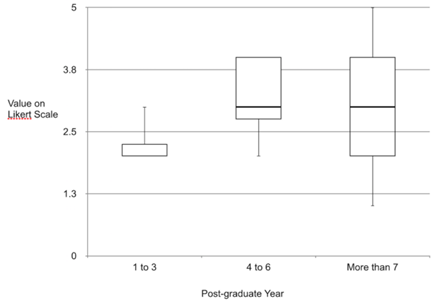
We compared the above statements between gender, junior or senior residency programme and post-graduate year and did not find a significant difference except regarding whether they feel that they “needed to have formal training before MET and a formative assessment during/after MET posting”. We compared 3 groups of residents (Postgraduate years 1-3, post-graduate years 4-6 and postgraduate years 7 or more) in their preference towards formal teaching. Overall, there was a significant difference among the 3 groups (p = 0.040) (Figure 1). A bonferroni post-hoc test showed that the significant difference lied between postgraduate year 1-3 and postgraduate year 4-6 only (p = 0.021). Other pairwise comparisons were not significant. There was no significant difference bet-ween postgraduate years 1-3 and more than 7 years (p = 0.723) and postgraduate years 4-6 and more than 7 years (p = 0.504).
4. Discussion
4.1 Summary of major findings
Our survey was done to evaluate residents’ percep-tion of MET in contribution to their training. Overall, it showed that most of the senior and junior residents perceive that MET contributed positively to their training and management of patients with urgent medical needs. It also showed agreement amongst residents that it improved their patient care and procedural skills, professionalism and systems based practice in line with training curriculum. In contrast, residents disagreed that MET was more cumbersome or time-consuming, that they were uncomfortable to resolve disagreements or that it exposes their weak-nesses. It was unclear if residents preferred formal training before MET, or whether they felt that it decreased clinical autonomy of primary team. The residents are also divided in opinion regarding whether MET frequently required their supervisor’s intervention. We found that residents in post graduate years 4 and above tended towards formal teaching or assessment while residents who were in postgraduate years 1-3 felt less strongly regarding this.
4.2 Comparison with other studies
There is limited literature assessing a trainee’s perception of their role in a MET with respect to contribution to their training. Jacques et al surveyed intensive care medicine trainees who regarded parti-cipation in MET as positive on training and on patient care in wards. In contrast to our findings where trainees were divided in opinion regarding need for formal training before MET; majority of trainees surveyed by Jacques felt that they were well trained for MET duties and that their ICU experience was sufficient training for MET. They also felt that MET accelerated end of life discussions [4]. Butcher et al surveyed resident physicians on whether they perceive educational benefit from collaboration with an RRS and whether they believe that the RRS adversely affects their clinical autonomy. Residents agreed that working with RRS was a valuable educational experience. They disagreed that RRS decreased their clinical autonomy while our residents were divided in their opinion [6]. The residents surveyed by Butcher were part of the primary team while their RRS/MET were nurse-led which may explain the difference in opinion as our residents surveyed are part of the MET. In addition, our junior residents spent only 3 months out of a 3-year training programme in an ICU posting with a MET rotation. They could feel that MET decreased a primary team’s clinical autonomy who would have more experience and perspective.
Sarani et al surveyed residents and registered nurses. Residents and RNs agreed that the medical emerg-ency team improved patient safety. Similar to our study, residents neither agreed nor disagreed with the notion that the creation of the medical emergency team decreased their opportunities to obtain critical care skills or education [7]. Maurice et al surveyed ICU team members (Intensive care registrars and nurses) and medical registrars and found that the majority agreed or strongly agreed that MET training was valuable and improves patient care. They also evaluated skills they wanted to further develop as part of this training programme and commonly selected “Team communication”, “Approach to Com-mon MET calls”, “Knowledge of Rapid Response Systems”, “Task management” and “Situational Awareness” [8]. Our findings are similar as majority agreed and strongly agreed that MET contributed positively to patient care.
4.3 Strengths and limitations
To our knowledge this is only the third survey to evaluate the perceptions of junior doctors in relation to the impact of their role MET responders in relation to their training. Strengths of our study include the fact that the survey was directed at the resident's training curriculum and hence directly reflect how MET contributes to such training. These ACGME domains were familiar to our residents as they were used in their individual trainee evaluation. The survey was conducted on all residents who rotated through the MET posting and responses were obtained in almost two-thirds of those surveyed. Our survey was self-administered via an online tool, this helped to eliminate the bias of the interviewer.
Despite these strengths, our study has some limit-ations. Our response rate was not 100%, therefore, the residents who did not respond might view MET differently from those who responded, resulting in non-response bias. Being an unvalidated survey, there was a risk of responders not understanding the question as it was intended to. Though the questions were structured according to the 6 ACGME domains to which the residents were accustomed to, therefore, reducing the need to pilot the survey to ensure cons-istent understanding of the questions. It was also done in a closed response format making it inflexible. Our study had better response rate than that done by Jacques which had a response rate of 38% [4]. However, Jacques surveyed trainees across different hospitals in Australia and New Zealand while our study was based in one hospital in Singapore. Nevertheless, our trainees had perspectives from two hospitals as they rotated between one hospital with MET and another without MET.
4.4 Implications
Our study showed that residents in post graduate years 4 and above tended towards formal teaching or formal assessment while residents who were in postgraduate years 1-3 felt less strongly regarding formal teaching or assessment. This reflected the level of training as most residents in post graduate years 4 and above were mainly senior residents who were team leaders in a MET activation. Therefore, they had to make decisions and lead a team of junior doctors, nurses and respiratory therapists in different emergency situations. This required clinical expertise in acute medicine, crisis team management and lead-ership qualities and good inter-professional comm-unication skills. On the other hand, residents in the early postgraduate years 1-3 were junior doctors and they did not need to lead the team; their role, rather, was to learn from the senior residents and carry out bedside procedures. This could have made them feel less of a need for formal education on MET. Never-theless, all residents would have had an introduction to the MET service during their orientation program-mme when rotated into CGH. MET was introduced with patient safety and outcome in mind. With resid-ents participation in MET, it resulted in achieving educational objectives according to the ACGME requirements. Therefore, developing a structured trai-ning programme and increasing specialist’s super-vision might aid in both training and patient outcome.
5. Conclusion
Our residents view MET positively in achieving training objectives, particularly in patient care and procedural skills, professionalism and systems based practice. Our findings suggest that there is a need to provide formal training for residents who lead MET and to increase specialist’s supervision to meet their training requirements.
References
- Winters BD, Weaver SJ, Pfoh ER, et al. Rapid-Response Systems as a Patient Safety Strategy: A Systematic Review. Annals of internal medicine 158 (2013): 417-425.
- Beitler JR, Link N, Bails DB, et al: Reduction in hospital-wide mortality after implement-tation of a rapid response team: A long-term cohort study. Crit Care 15 (2011): R269
- Chan PS, Jain R, Nallmothu BK, et al. Rapid response teams: A systematic review and meta-analysis. Arch Intern Med 170 (2010): 18-26.
- Jacques T, Harrison GA, McLaws ML. Attitudes towards and evaluation of medical emergency teams: a survey of trainees in intensive care medicine. Anaesth Intensive Care 36 (2008): 90-95.
- Benin AL, Borgstrom CP, Jenq GY, et al Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators BMJ Qual Saf 21 (2012): 391-398.
- Butcher BW, Quist CE, Harrison JD, et al. Effect of an RRT on Resident Perceptions. J. Hosp. Med 1 (2015): 8-12.
- Sarani B, Sonnad S, Bergey MR, et al. Resident and RN perceptions of the impact of a medical emergency team on educa-tion and patient safety in an academic medical center. Crit Care Med 37 (2009): 3091-3096.
- Le Guen M, Costa-Pinto R. Medical emerg-ency team training: needs assessment, feed-back and learning objectives. Intern Med J 51 (2021): 1298-1303.
- Michelle Cretikos, Jack Chen, Ken Hillman, et al. The objective medical emergency team activation criteria: A case–control study, Resuscitation 73 (2007): 62-72.
- Joint College of Intensive Care Medicine and Australian and New Zealand Intensive Care Society Special Interest Group on Rapid Response Systems; ANZICS Centre for Outcome and Resource Evaluation. Resource use, governance and case load of rapid response teams in Australia and New Zealand in 2014. Crit Care Resusc 18 (2016): 275-282.
- ANZICS-CORE MET dose Investigators, Jones D, Drennan K, et al. Rapid Response Team composition, resourcing and calling criteria in Australia. Resuscitation 83 (2012): 563-567.
- Accreditation Council for Graduate Medical Education. Common Program Requirements (2018).
- Jones D, Story D, Clavisi O, et al. An introductory guide to survey research in anaesthesia. Anaesth Intensive Care 34 (2006): 245-253.
Appendix:
|
Core competencies |
Description |
|
Patient Care & Procedural Skills |
Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health |
|
Medical Knowledge |
Residents must be able to demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. |
|
Practice-based Learning & Improvement |
Residents must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices |
|
Interpersonal & Communication Skills |
Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, patients’ families, and professional associates. |
|
Professionalism |
Residents must be able to demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. |
|
Systems Based Practice |
Residents must be able to demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value |
Table A: Summary of core competencies and description.
|
Survey Questions |
Post-graduate years 1-3, median (IQR) |
Post-graduate years 4-6, median (IQR) |
Post-graduate years 7 or more, median (IQR) |
P Value |
|
Patient Care & Procedural Skills |
||||
|
The posting in MET improved my clinical judgement in medical emergencies N = 61 n(%) |
4 (3.25-4.75) |
4 (4-5) |
4 (4-5) |
0.684 |
|
The posting improved my procedural skills eg intubation, Central Venous Pressure line setting, Intra-Arterial line setting N = 61 n(%) |
4 (4-5) |
4 (3-5) |
4 (3-5) |
0.524 |
|
I feel that MET posting has decreased clinical autonomy of the primary team N =61 n(%) |
3 (2-3) |
3 (2-4) |
3 (2-4) |
0.644 |
|
Met activations involved complex medical emergencies that frequently required my supervisor's intervention N =61 n(%) |
3 (3-4) |
3 (2-3) |
3 (2-3) |
0.263 |
|
Medical Knowledge |
||||
|
I do not feel that I am equipped to resolve disputes among clinicians that arose during met activations N = 59 n(%) |
2 (2-3.5) |
3 (2-3) |
3 (2-3) |
0.294 |
|
I feel that we need a have formal training before MET posting and a formative assessment during/ after MET posting N =59 n(%) |
2 (2-2.25) |
3 (2.75-4) |
3 (2-4) |
0.04 |
|
MET posting has exposed me to a wide variety of clinical cases. N=59 n(%) |
4 (4-5) |
4 (4-4) |
4 (4-5) |
0.677 |
Table B: Comparison of perceptions of questions related to patient care and procedural skills, and medical knowledge according to doctor seniority.
|
Survey Questions |
Post-graduate years 1-3 |
Post-graduate years 6-Apr |
Post-graduate years 7 or more |
P Value |
|
Practice-based Learning & Improvement |
||||
|
I was uncomfortable with MET activations as it exposed my weaknesses. N = 59 n(%) |
1.5 (1-2.25) |
2 (2-3) |
2 (2-3) |
0.151 |
|
The MET posting helped me achieve my learning goals. N = 59 n(%) |
4.5 (4-5) |
4 (4-5) |
4 (4-4) |
0.256 |
|
I was able to assume a teaching role during the MET posting. N = 59 n(%) |
3 (2-3.25) |
3 (2-4) |
3 (2-4) |
0.533 |
|
Interpersonal & Communication Skills |
||||
|
I tend to have differing opinions from the respiratory therapists in the team especially regarding non-invasive ventilation. N = 59 n(%) |
2 (1.75-2.25) |
2 (2-2) |
2 (1-2) |
0.179 |
|
Through the MET posting, I learnt to communicate with family particularly regarding end of life issues N = 59 n(%) |
4 (3.75-5) |
4 (3.75-4) |
4 (3-4) |
0.325 |
|
Professionalism |
||||
|
MET exposed me to various patient populations such as medical patients with acute surgical conditions or surgical patients with acute medical conditions. N =57 n(%) |
4 (4-5) |
4(4-4) |
4 (3-4) |
0.238 |
|
MET taught me the importance of patient autonomy and shared decision making with primary team doctors and nurses. N =57 n(%) |
4 (4-5) |
4 (3.25-4) |
4 (3-4) |
0.335 |
|
MET taught me the influence family has in a patient’s decision making. N =57 n(%) |
4 (4-5) |
4 (3-4) |
4 (3-4) |
0.216 |
Table C: Comparison of perceptions of questions related to practice-based learning and improvement, interpersonal and communication skills, and professionalism according to doctor seniority.
|
Survey Questions |
Post-graduate years 1-3 |
Post-graduate years 6-Apr |
Post-graduate years 7 or more |
P Value |
|
Systems Based Practice |
||||
|
Through MET posting, I learnt the importance of working with various departments and need for coordinating healthcare to ensure best outcome for patient eg dialysis planning N = 57 n(%) |
4.5 (4-5) |
4 (4-4) |
4 (3-5) |
0.209 |
|
Through the MET posting, I learnt how having a rapid response team can help to improve patient care N =57 n(%) |
4.5 (4-5) |
4 (4-5) |
5 (4-5) |
0.922 |
|
Overall |
||||
|
Overall, I feel MET contributed positively to patient care N =57 n(%) |
4.5 (4-5) |
4 (4-5) |
4(4-5) |
0.684 |
|
Overall, I feel MET posting contributed positively to my training N =57 n(%) |
4.5 (4-5) |
4 (4-5) |
4 (4-5) |
0.773 |
|
Overall, regarding resuscitation of patients, MET activations made it more cumbersome N =57 n(%) |
1.5 (1-2) |
2 (1-2) |
2 (1-2) |
0.495 |
|
Overall, regarding resuscitation of patients, MET activations made it more time-consuming. N =57 n(%) |
1.5(1-2) |
2 (1-2) |
2 (1-2) |
0.397 |
|
Overall, regarding resuscitation of patients, MET activations made it more efficient N =57 n(%) |
4.5 (3.75-5) |
4 (4-5) |
4 (4-5) |
0.673 |
|
Overall, regarding resuscitation of patients, MET activations made it safer. N =57 n(%) |
5 (4-5) |
4 (4-5) |
5 (4-5) |
0.286 |
Table D: Comparison of perceptions of questions related to systems based practice, and overall impressions of the MET according to doctor seniority.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 