Lifestyle Behavior Intervention Effect on Physical Activity in Low-Income Overweight or Obese Mothers of Young Children
Mei-Wei Chang1*, Jolynn Pek2, Duane T Wegener2, Jessica Page Sherman1
1The Ohio State University, College of Nursing, Ohio, United States
2Department of Psychology, The Ohio State University, Ohio, United States
*Corresponding Author: Mei-Wei Chang, The Ohio State University, College of Nursing, Ohio, United States
Received: 05 July 2022; Accepted: 18 July 2022; Published: 17 August 2022
Article Information
Citation: Mei-Wei Chang, Jolynn Pek, Duane T Wegener, Jessica Page Sherman. Lifestyle Behavior Intervention Effect on Physical Activity in Low-Income Overweight or Obese Mothers of Young Children. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 361-369.
View / Download Pdf Share at FacebookAbstract
Background: Physical activity promotes health benefits. Yet, low-income overweight or obese mothers with young children have been significantly underrepresented in prior lifestyle intervention studies that include healthy eating and physical activity. The study aimed to evaluate an intervention effect on physical activity among these women participated in a community-based randomized controlled lifestyle behavior intervention study.
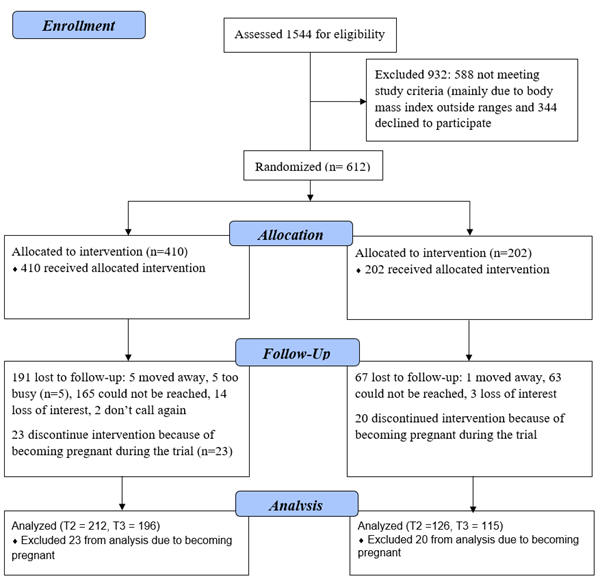
Methods: Participants (N = 612) were randomly assigned to a 16-week lifestyle behavior intervention or comparison group. All participants self-reported self-efficacy, emotional coping, social support, autonomous motivation, and leisure time physical activity. We applied a general linear mixed model to test the intervention effect on physical activity at the end of the intervention (T2, 338 participants) and at 3-month follow-up (T3, 311 participants).
Results: At T2, the intervention group reported a statistically significant higher score in self-efficacy (d = 0.38), emotional coping (d = 0.21), autonomous motivation (d = 0.26), and vigorous physical activity (d = 0.28) than the comparison group. However, there was no group difference in social support. At T3, the intervention group reported a statistically significant higher score in self-efficacy (d = 0.24) than the comparison group, but there were no group differences in other measures.
Conclusion: The 16-week lifestyle behavior intervention yielded short and long-term effects on self-efficacy but only short-term effects on emotional coping, autonomous motivation, and vigorous physical activity.
Keywords
<p>Low-Income, Obesity, Self-Efficacy, Physical Activity, Autonomous Motivation, Emotional Coping</p>
Article Details
1. Introduction
Approximately 50% of child-bearing aged women are overweight or obese [1], which increases their risk for many chronic conditions including breast cancer [2], type 2 diabetes, hypertension, and cardiovascular disease [3]. When these women become pregnant, they are at risk for adverse maternal and birth outcomes. For example, growing evidence has shown that pre-pregnancy overweight or obesity is a strong predictor of excessive gestational weight gain and pregnancy complications [4]. Excessive gestational weight gain is associated with many adverse maternal and birth outcomes (e.g., gestational diabetes [5], gestational hypertension [6], large for gestational age newborn [7, 8]) and a strong predictor of obesity later in women’s lives [9, 10]. Obesity and its related chronic conditions described above are preventable and can be improved by engaging in recommended physical activity (150 minutes/week [moderate physical activity] or 75 minutes/week [vigorous physical activity]) [2, 11]. Yet, approximately 50% of child-bearing aged women, especially those with obesity, do not engage in recommended physical activity [12]. Also, among overweight or obese postpartum women, only 24-34% meet the guideline [13]. Mothers of young children are less likely to engage in physical activity than age-matched women without children [14]. Low-income adults, especially women, are 1.6 to 1.9 times less likely to meet the physical activity guideline than higher income adults [15]. Taken together, the public health importance of increasing physical activity in low-income overweight or obese mothers of young children, the priority population, is crucial to promote positive health outcomes.
Two recent meta-analyses [16, 17] and an individual effectiveness intervention study [18] have shown that healthy lifestyle behaviors (healthy eating, physical activity) promote postpartum weight loss, including for low-income, overweight or obese women [18]. Despite the promise in existing research, most prior studies have had relatively small sample sizes, mainly due to limitations for enrolling women within one year postpartum [16, 17] -- high infant care demands prevent women from participating in intervention studies [16]. This is a missed opportunity to have broader impact on the obesity epidemic [19] and pregnancy-related maternal outcomes, because 40-50% of obese women gain at least 2 body mass index (BMI) units between pregnancies [20].
We conducted a randomized controlled community-based lifestyle behavior intervention aimed at prevention of further weight gain for low-income overweight or obese mothers with young children (up to 4.5 years old). Intervention effects on body weight [21], dietary intake [22], and psychosocial health [23, 24] have been previously published. In the current paper, we present results of the intervention on physical activity. We hypothesized that the intervention group would show improvements in physical activity and its associated self-efficacy, emotional coping, social support, and autonomous motivation over time compared to the comparison group.
2. Materials and Methods
2.1 Setting and study sample
A detailed description of the study setting, sample, and procedure has been published elsewhere [25, 26]. Briefly, participants were recruited (September 2012 - January 2015) from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in Michigan, USA. In order to be qualified and enrolled in WIC, individuals must have income at or below 185% of the federal poverty line. The study-trained peer recruiters personally invited women waiting for their WIC appointment to be screened. Eligible participants were Non-Hispanic Black or White (hereafter Black, White), between 18 and 39 years old, between 6 weeks and 4.5 years postpartum, and had a BMI between 25.0 and 39.9 (calculated using measured height and weight). They provided a written consent prior to participating in the study. Michigan State University Institutional Review Board approved the study procedure.
2.2 Intervention
A detailed description of intervention procedures has been previously published [25]. Briefly, the 16-week intervention had two components: viewing 10 culturally sensitive video lessons in DVD format at home (20 min/video) and joining 10 peer support group teleconferences at convenience locations (30 min/session). The intervention participants were asked to view a video lesson then join the peer support group teleconference every week during weeks 1-4 followed by every other week during weeks 6-16. The intervention topics included stress management (weeks 1-4, weekly, 1 lesson/week) that included walking to reduce stress and improve negative emotion, healthy eating (weeks 6-14, every other week, 1 lesson/every other week), and physical activity (week 16, 1 lesson). A detailed description of stress management (e.g., time management, walking to reduce stress) and healthy eating (e.g., meal planning, grocery shopping) lessons has been published elsewhere [25, 27]. To create culturally sensitive videos, the intervention videos (unscripted) featured peers of the priority population and their family members, especially young children. They wore casual clothes and demonstrated indoor (e.g., jumping jacks with children, marching in place while watching TV, dancing) and outdoor activities (e.g., playing tag with children, walking in the safe neighborhood, parking farther from their destination) that are commonly engaged by the priority population. They also showed how they applied practical ways to overcome daily challenges to be physically active. For example, to overcome lack of time, participants were asked to pay attention to how they spent their day, then identified small chunks of time daily to be physically active (e.g., making several trips to take trash out, climbing stairs at home).
For the intervention videos, we applied 3 key concepts of Social Cognitive Theory [28]. These concepts were self-efficacy, defined as an individual’s belief in his/her ability (confidence) to execute a specific task/behavior, emotional coping response referring to strategies used to manage negative emotion including stress and social support. To build self-efficacy, participants learned ways to identify and build their strengths; for example, being aware of existing strengths, and taking small steps to achieve a realistic and achievable goal. To improve emotional control, participants were for example, encourage to talking a walk while feeling upset. Participants also learned ways to elicit and/or build social support (e.g., asking family members or friends to provide positive verbal support for being physically active). For the peer support group teleconference, we utilized motivational interviewing techniques, which have been closely aligned with Self-Determination Theory and its key concept of autonomous motivation [24]. Autonomous motivation refers to one’s interest to modify or maintain behaviors that are consistent with individuals’ personal values (for example, being a good role model for children). During the peer support group teleconference, the trained moderators elicited participants’ personal values, motivation, and challenges in being physically active. Each session was audio recorded with participants’ permission and we listened to 25% randomly selected audios for the purpose of monitoring intervention fidelity.
2.3 Measures
Participants completed the demographic questions via a pencil-and-paper survey while at the WIC office. They completed survey data collection (described below) via phone interviews at baseline (T1), immediately after the intervention (T2), and at a 3-month follow up (T3).
2.3.1 Self-efficacy for physical activity, hereafter, self-efficacy: A self-efficacy survey (10 items) with previously established construct validity and reliability for the priority population was used to measure self-efficacy [29]. Participants were asked to rate their confidence level, ranging from 1 (not at all confident) to 4 (very confident), toward engaging in physical activity in a various situations (e.g., stress, exercising alone) [29]. We averaged responses to the 10 items to create a self-efficacy score, where higher scores means higher self-efficacy.
2.3.2 Emotional coping response for physical activity, hereafter, emotional coping: An emotional coping response survey (5 items) with previously established construct validity and reliability for the priority population was used to measure emotional coping [29]. Participants were asked to rate their degree of agreement, ranging from 1 (strongly disagree) to 4 (strongly agree), with engaging in physical activity when experiencing negative emotions (e.g., upset, frustrated) [29]. We averaged responses to the 5 items to create an emotional coping score, where higher scores indicate greater use of physical activity for emotional coping.
2.3.3 Social support for physical activity, hereafter, social support: A 6-item survey with previously established construct validity and good reliability for the priority population was used to measure social support [29]. Participants were asked to rate the frequency, ranging from 1 (rarely or never) to 4 (usually or always) of receiving encouragement from their family members, friends, co-workers or others to be physically active (e.g., praise you for exercising) [29]. We averaged responses to the 6 items to create a social support score, where higher scores means more social support.
2.3.4 Autonomous motivation for physical activity, hereafter, autonomous motivation: The Treatment Self-Regulation Questionnaire (6 items) with previously established construct validity and reliability was used to measure autonomous motivation [30]. Participants were asked about the reasons for exercising or being physically active. For example, “the reason I exercise regularly is because I have carefully thought about it and believe it is very important to me.” Responses ranged from 1 (not at all true) to 7 (very true). We averaged responses to the 6 items to create an autonomous motivation score, where higher scores mean higher autonomous motivation.
2.4 Physical activity: leisure time physical activity
We used a subscale of the Pregnancy Infection and Nutrition Survey (3 items) with reasonable validity to assess leisure time physical activity [31, 32] Participants self-reported non-work-related leisure time physical activity (walking, swimming, and dancing) that caused them to feel some increase in heart rate and breathing in the last 7 days. For each leisure time activity, participants responded “Yes” or “No” to whether they engaged in the activity. If participants responded “Yes” to the activity, they provided responses on frequency (total), mean duration/frequency, and intensity (light, moderate, or vigorous physical activity). If participants responded “No” to the activity, they skipped the frequency, duration, and intensity questions. To compute minutes/week for each level of physical activity, we first multiplied frequency by duration for the activity followed by summing up the 3 types of physical activity (walking, swimming, dancing) for a specific level (light, moderate, or vigorous).
2.5 Statistical analysis
All analyses were performed using SAS version 9.4 (Carry, NC, USA: SAS Institute Inc). We excluded 43 women who became pregnant during the trial, which resulted in 569 women (intervention group = 387 and comparison group = 182) in the analysis. We conducted descriptive analysis on demographic variables. The variables of interest included self-efficacy, emotional coping, social support, autonomous motivation, and amount of leisure time physical activity (light, moderate, and vigorous) at T2 (338; 212 intervention, 126 comparison) and T3 (311; 196 intervention, 115 comparison). We included light physical activities because growing evidence has shown their long-term health benefits [33, 34]. Because of high dropout rates (T2 = 41% and T3 = 45%), we did not apply intent-to-treat analysis. Instead, we performed a general linear mixed model for repeated measures and used all available data without any ad hoc imputation. In the analysis, we also adjusted for baseline measurements. For longitudinal studies with a high dropout rate, the use of a general liner mixed model including all available data is a more powerful approach than applying mixed model analysis with ad hoc imputation or intent-to-treat [35]. Cohen’s d was used to calculate effect size and 95% confidence intervals.
3. Results
3.1 Baseline demographic characteristics
Figure 1 depicts the study consort chart. Table 1 shows demographic characteristics of the study sample. The demographic characteristics were similar between the intervention and comparison groups. Most participants were White, non-smokers, and had some college or higher education.
3.2 Intervention adherence
Of intervention participants, 73% viewed at least one video lesson (total of 10 available), and 53% joined at least one peer support group teleconference session (total of 10 available) [21]. The intervention adherence rates for the physical activity were 49.4% for viewing the video lesson and 18.1% for joining the peer support group teleconference sessions.
3.3 Psychosocial concepts
Table 2 presents the intervention effects on the psychosocial concepts: self-efficacy, emotional coping, social support, and autonomous motivation. Compared with the comparison group, the intervention group reported a significantly higher mean score on self-efficacy at both T2 (mean difference = 0.22, d = 0.38, p < 0.001) and T3 (mean difference = 0.14, d = 0.24, p = 0.04). The intervention group also reported a significantly higher mean score on use of physical activity for emotional coping than the comparison group at T2 (mean difference = 0.21, d = 0.21, p < 0.00), but there was no significant group difference at T3. There was no significant group difference on reported social support at both T2 and T3. Finally, the intervention group reported a significantly higher mean score on autonomous motivation than the comparison group at T2 (mean difference = 0.21, d = 0.26, p = 0.02); however, there was no group difference at T3.
3.4 Leisure time physical activity
There were no significant differences between the intervention and comparison groups on light and moderate physical activity at T2 and T3. The intervention group reported a significantly higher mean score on vigorous physical activity than the comparison group at T2 (mean difference = 22.29, d = 0.28, p = 0.02), but there was no group difference at T3.
Table 1: Study Participant Characteristics (N = 569).
|
Demographic Characteristics |
Intervention (n = 387) |
Comparison (n = 182) |
|
Mean (SD) |
Mean (SD) |
|
|
Age (years) |
28.4 (5.0) |
28.9 (5.0) |
|
Postpartum status (years) |
1.6 (1.2) |
1.9 (1.3) |
|
Body mass index (BMI, Kg/m2) |
32.2 (4.4) |
31.7 (4.2) |
|
n (%) |
n (%) |
|
|
Race |
||
|
Non-Hispanic Black |
81 (21%) |
40 (22%) |
|
Non-Hispanic White |
306 (79/%) |
142 (78%) |
|
Smoking |
||
|
Never smoked |
167 (43%) |
93 (51%) |
|
Smoked, but quit |
114 (30%) |
47 (26%) |
|
Smoker |
106 (27%) |
42 (23%) |
|
Education |
||
|
High school or less education |
126 (32%) |
61 (34%) |
|
Some college or technical school |
186 (48%) |
84 (46%) |
|
College graduate or higher |
75 (19%) |
37 (20%) |
|
Employment |
||
|
Full-or part- time |
162 (42%) |
84 (46%) |
|
Unemployed |
76 (20%) |
42 (23%) |
|
Homemaker |
110 (28%) |
38 (21%) |
|
Self-employed/student/other |
39 (10%) |
18 (10%) |
Table 2: Means, Standard Deviations, (Adjusted) Effect Sizes and 95% CIs of Self-efficacy, Emotional Coping Response, Social Support, and Autonomous Motivation for the Intervention and Comparison Groups.
|
Intervention M (SD) |
Comparison M (SD) |
Effect Size |
95% CI |
|
|
Baseline |
||||
|
Self-efficacy |
2.38 (0.60) |
2.35 (0.59) |
NA |
NA |
|
Emotional coping |
2.50 (0.73) |
2.48 (0.70) |
NA |
NA |
|
Social support |
1.82 (0.62) |
1.84 (0.66) |
NA |
NA |
|
Autonomous motivation |
5.54 (1.40) |
5.40 (1.49) |
NA |
NA |
|
At the end of the 16-week intervention (T2) |
||||
|
Self-efficacy |
2.68 (0.63) |
2.45 (0.63) |
0.38* |
0.15, 0.60 |
|
Emotional coping |
2.75 (0.67) |
2.54 (0.65) |
0.21* |
0.10, 0.54 |
|
Social support |
1.93 (0.67) |
1.80 (0.64) |
0.18 |
-0.04, 0.40 |
|
Autonomous motivation |
5.98 (1.16) |
5.73 (1.39) |
0.26* |
0.04, 0.48 |
|
At 3-month follow up (T3) |
||||
|
Self-efficacy |
2.70 (0.63) |
2.56 (0.64) |
0.24* |
0.01, 0.47 |
|
Emotional coping |
2.74 (0.67) |
2.62 (0.61) |
0.20 |
-0.03, 0.43 |
|
Social support |
1.87 (0.65) |
1.84 (0.69) |
0.02 |
-0.21, 0.25 |
|
Autonomous motivation |
5.98 (1.03) |
5.84 (1.35) |
0.13 |
-0.10, 0.36 |
*p < 0.05 and CI = confidence interval. Baseline: N = 569 (387 intervention, 182 comparison). T2: N = 338 (212 intervention, 126 comparison). T3: N = 311 (196 intervention, 115 comparison).
Table 3: Means, Standard Deviations, and (Adjusted) Effect sizes and CIs for Physical Activity between the Intervention and Comparison Groups.
|
Intervention M (SD) |
Comparison M (SD) |
Effect Size |
95% CI |
|
|
Baseline |
||||
|
Light Activity |
161.99 (470.08) |
231.87 (699.20) |
NA |
NA |
|
Moderate Activity |
174.20 (1129.01) |
125.21 (506.73) |
NA |
NA |
|
Vigorous Activity |
22.84 (117.92) |
1.49 (10.35) |
NA |
NA |
|
At the end of the 16-week intervention (T2) |
||||
|
Light Activity |
97.77 (245.52) |
179.98 (588.00) |
-0.11 |
-0.37, 0.15 |
|
Moderate Activity |
122.20 (333.49) |
91.95 (135.58) |
0.04 |
-0.22, 0.30 |
|
Vigorous Activity |
23.46 (86.12) |
0 (0) |
0.28* |
0.04, 0.52 |
|
At 3-month follow up (T3) |
||||
|
Light Activity |
233.18 (1282.40) |
102.85 (393.45) |
0.18 |
-0.08, 0.45 |
|
Moderate Activity |
91.29 (167.78) |
81.98 (183.08) |
0.01 |
-0.25, 0.28 |
|
Vigorous Activity |
5.56 (30.23) |
17.60 (70.52) |
-0.16 |
-0.41, 0.09 |
*p < 0.05 and CI = confidence interval. Baseline: N = 569 (387 intervention, 182 comparison). T2: N = 338 (212 intervention, 126 comparison). T3: N = 311 (196 intervention, 115 comparison).
4. Discussion
Low-income overweight or obese mothers with young children are at high risk for many chronic conditions, which can be delayed or improved by being physically active. This study is one of the first to enroll these mothers, and results of the present study partially supported our hypotheses. The 16-week lifestyle intervention boosted the intervention participants’ self-efficacy for physical activity, though the effect size slightly decreased overtime. The present study also revealed that the intervention increased reported use of physical activity for coping with negative emotions (emotional coping) and increased autonomous motivation at the end of the intervention. The lack of intervention effect beyond intervention period might be related to relapse or to devoting relatively little time in the intervention to physical activity per se (i.e., most of the intervention focused on stress management and healthy eating).
Despite our efforts to help participants increase social support, we did not find group differences at any time point of data collection. There are possible explanations based on listening to the randomly selected peer support group teleconference audio recording (with participants’ permission). We learned that many women expressed negative relationships with their own mothers or family members. Others were hesitant to ask for support because they were afraid of being rejected. Also, some partners of our intervention participants discouraged them from being physically active because the partners did not want them to lose weight.
Consistent with a prior systematic review [36] and an integrative review of physical activity in postpartum women, regardless of participants’ socioeconomic status [37], we found a small intervention effect on physical activity (vigorous only) immediately after the 16-week intervention but the effect diminished over time. Taking together our and prior research findings [36, 37], the length of intervention and mode of delivery do not seem to play a role in the size of the intervention effect.
Also, in order to maximize effects, the theory used to guide interventions might need to go beyond the Social Cognitive Theory. For example, our and a prior intervention study of working mothers [38] applied the Social Cognitive Theory and yielded the same results: only short-term improvement. Despite our lack of intervention effect on moderate physical activity, our findings of light activity are promising. Whereas the mean minutes of the comparison group declined overtime (from 179.48 at T2, to 107.50 at T3), the mean minutes of light activity in the intervention group more than doubled (from 103.6 at T2, to 235.7 at T3). The 235.7 minutes/week translated to 9.4 METs/hour (metabolic equivalent task, a measure of energy expenditure). Prior studies have shown the health benefit of increases in light physical activity in the long term, for example for weight loss and improved blood lipids [34]. Others have reported the health benefits of 7.5 to 15 METs/week regardless of intensity. Given the continued challenges in maintenance of moderate and vigorous physical activity over time and the health benefits of light physical activity, lifestyle interventions or physical activity interventions might emphasize the adoption of light physical activity that can be easily to incorporated into daily life instead of emphasizing moderate or vigorous activity.
Barriers preventing women from engaging in physical activities include lack of time and childcare, family responsibilities, not prioritizing one’s health over other competing responsibilities, neighborhood safety concern, and lack of a physical activity role model [39, 40]. Motivators for physical activity in the priority population include a focus on benefit (e.g., stress relief, increased energy), weight loss, and social support [39]. Our intervention had addressed these barriers and motivators. However, lack of childcare and social support, competing priorities or responsibilities, and living in an unsafe neighborhood might not be easily addressable. Such barriers might have been especially constraining for our participants who moved to a new area that is far away from close family members or friends or who experienced unexpected life events (e.g., being evacuated, taking care of a sick a child or family member, violence).
Nevertheless, there are possible explanations for why our participants did not undertake greater (moderate or vigorous) physical activity and/or maintain. First, our participants were mothers of young children and might have engaged in casual walking (light physical activity) with children instead of brisk walking (moderate physical activity). Also, in our stress management lessons, we recommended walking as a way to better manage stress and/or negative emotion and did not emphasize brisk walking. Thus, many women might have engaged in casual walking, which is supported by our finding—the amount of light physical activity doubled between T2 and T3, though with particularly high variance. Moreover, our intervention encouraged women to make small and gradual changes. Thus, casual walking might have the first step for the target population to be physically active. The intervention adherence rate for joining the peer support group for physical activity was disappointing, perhaps because physical activity was the last lesson presented based on suggestions from our peer advisory group. The group thought that participants must know ways to manage stress followed by healthier eating before starting to think about being more physically active. The physical activity survey asked participants to report their physical activity over the last 7 days and did not ask whether this was a typical week for engaging in physical activity. Therefore, we do not know whether the data collected reflected participants’ typical week or an unusual week.
4.1 Limitations
There are study limitations. The physical activity was measured using self-report rather than an objective measure (e.g., Actigraph accelerometer). Yet, there are limitations of using an Actigraph accelerometer, such as being unable to measure activity when swimming. Also, participants reported their level of physical activity based on perceived exertion. Thus, we might have misclassified participants into the 3 different levels (intensity) of physical activity. Our intervention only included 1 physical activity lesson (1 video and 1 peer support group teleconference), but our stress management lesson included walking as a strategy to manage stress and negative emotion. Time conflicts and competing interests were given as the most frequent reasons for low intervention adherence rates for joining peer support groups. Finally, results of this study might not be generalizable to low-income overweight or obese women of young children in a different geographic location because differences in weather or layout of living spaces might affect physical activity.
5. Conclusion
The 16-week lifestyle behavior intervention delivered through culturally sensitive videos and peer support group teleconferences promoted self-efficacy, use of physical activity to cope with negative emotions, autonomous motivation for physical activity, and vigorous physical activity in low-income overweight or obese mothers with young children. However, the gains for emotional coping, autonomous motivation and vigorous physical activity only accrued in the short-term, not in the long-term. The intervention did not influence social support. Future study of interventions for this population might involve identifying motivators for adoption of moderate physical activity and maintenance of physical activity over time. Also, rather than emphasizing moderate or vigorous physical activity, future interventions might emphasize light physical activity that can be easily incorporated into daily life. This approach might be easier for mothers of young children to adopt.
Acknowledgement
The work was supported by a grant (R18-DK-083934) from the National Institute of Diabetes and digestive and Kidney Diseases (NIDDK).
Conflict of Interest
All authors declare no conflict of interest.
References
- Hales CM, Fryar CD, Carroll MD, et al. Differences in Obesity Prevalence by Demographic Characteristics and Urbanization Level Among Adults in the United States, 2013-2016. JAMA 319 (2018): 2419-2429.
- Matthews CE, Moore SC, Arem H, et al. Amount and Intensity of Leisure-Time Physical Activity and Lower Cancer Risk. J Clin Oncol 38 (2020): 686-697.
- Zheng Y, Manson JE, Yuan C, et al. Associations of Weight Gain From Early to Middle Adulthood With Major Health Outcomes Later in Life. JAMA 318 (2017): 255-269.
- Marshall NE, Abrams B, Barbour LA, et al. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol 226 (2022): 607-632.
- Hedderson MM, Gunderson EP, Ferrara A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet Gynecol 115 (2010): 597-604.
- Ren M, Li H, Cai W, et al. Excessive gestational weight gain in accordance with the IOM criteria and the risk of hypertensive disorders of pregnancy: a meta-analysis. BMC Pregnancy Childbirth 18 (2018): 281.
- Johansson S, Villamor E, Altman M, et al. Maternal overweight and obesity in early pregnancy and risk of infant mortality: a population based cohort study in Sweden. BMJ 349 (2014): g6572.
- Goldstein RF, Abell SK, Ranasinha S, et al. Association of Gestational Weight Gain with Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA 317 (2017): 2207-2225.
- Lau EY, Liu J, Archer E, et al. Maternal Weight Gain in Pregnancy and Risk of Obesity among Offspring: A Systematic Review. Journal of Obesity (2014).
- Mamun AA, Mannan M, Doi SA. Gestational weight gain in relation to offspring obesity over the life course: a systematic review and bias-adjusted meta-analysis. Obes Rev 15 (2014): 338-347.
- Dipietro L, Evenson KR, Bloodgood B, et al. Benefits of Physical Activity during Pregnancy and Postpartum: An Umbrella Review. Med Sci Sports Exerc 51 (2019): 1292-1302.
- Centers for Disease C, Prevention. Adult participation in aerobic and muscle-strengthening physical activities--United States, 2011. MMWR Morb Mortal Wkly Rep 62 (2013): 326-330.
- Durham HA, Morey MC, Lovelady CA, et al. Postpartum physical activity in overweight and obese women. J Phys Act Health 8 (2011): 988-993.
- Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med 28 (1999): 313-323.
- Shuval K, Li Q, Gabriel KP, et al. Income, physical activity, sedentary behavior, and the 'weekend warrior' among U.S. adults. Prev Med 103 (2017): 91-97.
- Lim S, O'Reilly S, Behrens H, et al. Effective strategies for weight loss in post-partum women: a systematic review and meta-analysis. Obes Rev 16 (2015): 972-987.
- Lim S, Liang X, Hill B, et al. A systematic review and meta-analysis of intervention characteristics in postpartum weight management using the TIDieR framework: A summary of evidence to inform implementation. Obes Rev 20 (2019): 1045-1056.
- Phelan S, Hagobian T, Brannen A, et al. Effect of an Internet-Based Program on Weight Loss for Low-Income Postpartum Women: A Randomized Clinical Trial. JAMA 317 (2017): 2381-2391.
- McKinley MC, Allen-Walker V, McGirr C, et al. Weight loss after pregnancy: challenges and opportunities. Nutr Res Rev 31 (2018): 225-238.
- Jain AP, Gavard JA, Rice JJ, et al. The impact of interpregnancy weight change on birthweight in obese women. Am J Obstet Gynecol 208 (2013): 205 e201-207.
- Chang MW, Brown R, Nitzke S. Results and lessons learned from a prevention of weight gain program for low-income overweight and obese young mothers: Mothers In Motion. BMC Public Health 17 (2017): 182.
- Chang MW, Brown R, Nitzke S. A Community-Based Intervention Program's Effects on Dietary Intake Behaviors. Obesity (Silver Spring) 25 (2017): 2055-2061.
- Chang MW, Nitzke S, Brown R. Mothers in Motion intervention effect on psychosocial health in young, low-income women with overweight or obesity. BMC Public Health 19 (2019): 56.
- Markland D, Ryan RM, Tobin VJ, et al. Motivational interviewing and self-determination theory. Journal of Social and Clinical Psychology 24 (2005): 811-831.
- Chang MW, Nitzke S, Brown R, et al. A community-based prevention of weight gain intervention (Mothers In Motion) among young low-income overweight and obese mothers: design and rationale. BMC Public Health 14 (2014): 280.
- Chang M, Nitzke S, Brown R, et al. Recruitment Challenges and Enrollment Observations from a Community Based Intervention (Mothers In Motion) for Low-Income Overweight and Obese Women. Contemporary Clinical Trials Communication 5 (2017): 26-33.
- Chang M, Brown R, Nitzke S. A Community-based Intervention Program: Intervention Effect on Dietary Intake Behaviors. In press.
- McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behavior interact: Social Cognitive Theory. In: Glanz K, Rimer BK, Viswanath K, eds. Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco: Jossey-Bass Publishers (2008): 169-188.
- Chang M, Brown R, Nitzke S. Scale development: Factors affecting diet, exercise, and stress management (FADESM). BMC Public Health 8 (2008).
- Pelletier LG, Tuson KM, Haddad NK. Client Motivation for Therapy Scale: a measure of intrinsic motivation, extrinsic motivation, and amotivation for therapy. J Pers Assess 68 (1997): 414-435.
- Evenson KR, Wen F. Measuring physical activity among pregnant women using a structured one-week recall questionnaire: evidence for validity and reliability. Int J Behav Nutr Phys Act 7 (2010): 21.
- Chang MW, Hales D, Brown R, et al. Validation of PIN 3 physical activity survey in low-income overweight and obese young mothers. BMC Public Health 15 (2015): 121.
- Loprinzi PD. Light-Intensity Physical Activity and All-Cause Mortality. Am J Health Promot 31 (2017): 340-342.
- Fuzeki E, Engeroff T, Banzer W. Health Benefits of Light-Intensity Physical Activity: A Systematic Review of Accelerometer Data of the National Health and Nutrition Examination Survey (NHANES). Sports Med 47 (2017): 1769-1793.
- Chakraborty H, Gu H. A mixed model approach for intent-to-treat analysis in longitudinal clinical trials with missing values. North Carolina: Research Triangle Park (2009).
- Gilinsky AS, Dale H, Robinson C, et al. Efficacy of physical activity interventions in post-natal populations: systematic review, meta-analysis and content coding of behaviour change techniques. Health Psychol Rev 9 (2015): 244-263.
- Gilbert L, Gross J, Lanzi S, et al. How diet, physical activity and psychosocial well-being interact in women with gestational diabetes mellitus: an integrative review. BMC Pregnancy Childbirth 19 (2019): 60.
- Mailey EL, McAuley E. Impact of a brief intervention on physical activity and social cognitive determinants among working mothers: a randomized trial. J Behav Med 37 (2014): 343-355.
- Chang M, Nitzke S, Guilford E, et al. Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J Am Diet Assoc 108 (2008): 1023-1028.
- Joseph RP, Ainsworth BE, Keller C, et al. Barriers to Physical Activity Among African American Women: An Integrative Review of the Literature. Women Health 55 (2015): 679-699.


 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 