Lumbar Disc Nucleus Replacement for Refractory Back Pain: A Case Report
Jeff D. Golan, MD1*, Michael G. Hess, MD2, Francisco Javier Duarte, MD3, Loren Francis4, Maren Lange5
1Jewish General Hospital, Division of Neurosurgery, 3755 Cote Ste-Catherine Rd, Suite E-929 Montreal, Quebec, H3T 1E2 Canada
2116 Harley Street London W1G 7JL, UK
3Sanatorio Americano España 935 c/, Washington, Asunción 1101, Paraguay
41918 Southard St. Erie, CO. 80516
5Margarethenstraße 18, 47198 Duisburg, Germany
*Corresponding Author: Jeff D. Golan, Jewish General Hospital, Division of Neurosurgery, 3755 Cote Ste- Catherine Rd, Suite E-929, Montreal, Quebec, H3T 1E2 Canada.
Received: 07 July 2023; Accepted: 17 July 2023; Published: 27 July 2023
Article Information
Citation: Jeff D. Golan, Michael G. Hess, Francisco Javier Duarte, Loren Francis, Maren Lange. Lumbar Disc Nucleus Replacement for Refractory Back Pain: A Case Report. Journal of Spine Research and Surgery 5 (2023): 65-68.
View / Download Pdf Share at FacebookAbstract
Back pain is one of the most common sources of pain and disability in the world. The value of surgically treating discogenic low back pain (dLBP) is controversial and currently limited to fusion or total disc replacement. The clinical case presented is a 25-year-old man with 5 years of spontaneous onset low back pain refractory to medical care. The patient was enrolled in a Phase 1 clinical trial designed to test the safety profile of a novel nucleus replacement device. He underwent a left-sided anterior retroperitoneal approach, nuclectomy and implantation of the PerQdisc. At the 2-year follow up period his pain scores had improved significantly. Dynamic radiographs demonstrated 23.4 degrees of segmental motion with no suggestion of inflammation on MRI.
This case demonstrates successful diagnosis of dLBP and surgical treatment using a novel motion-sparing and form-fitting nucleus replacement device, in the context of a clinical trial. While the diagnostic criteria used in this case report may be a useful guide to identify other patients with dLBP, the surgical treatment offered should be interpreted with caution until appropriate clinical trials are presented.
Keywords
<p>Lumbar disc; discogenic low back pain (dLBP)</p>
Article Details
Introduction
Back pain is one of the most common sources of pain and disability in the world[1]. There are various types of pain commonly grouped into this broad pathological entity. Discogenic low back pain is a term generally applied when the affected disc is the actual source of pain. The cause of dLBP may be related to injury sustained by the nucleus pulposus (NP) or the annulus fibrosis (AF) by excessive wear and tear from poor biomechanics, significant accident, or injury [2]. The damage to the disc leads to inflammation within the NP and microtearing of the AF of the disc that contains the nucleus[3]. The nucleus tissue has poor blood supply and inflammation accumulates while abnormally sensitive nerve endings grow into microtears and render the disc hypersensitive to movements that would not otherwise cause pain[4].
The gold standard for surgical treatment of dLBP is controversial[5] but is currently limited to fusion and in some cases total disc replacement. Nucleus replacement alternatives have been tried in the past with varying success[6][7][8].
Case Report
The patient is a 25-year-old man with 5 years of spontaneous onset low back pain. He underwent extensive physical therapy, taken anti-inflammatory medication and low-grade opioids, as well as undergone facet-joint blocks at L4-5 and injections to his bilateral Bertolotti’s joints all without lasting relief or improved function. The patient was unable to perform his semi-manual job as a pharmacist, standing 8-hours per day. On physical examination, he was 170 cm and 83 Kg, there were no neurological deficits found. In addition, the straight-leg test, femoral stretch test, and sacroiliac joint provocative maneuvers were all negative.
On MRI there was minimal degenerative disc changes (Pfirrmann Grade 2) and facet changes (Weishaupt grade 1) at L4-5 with minimal right-sided L4-5 partial-thickness annular tear (Figure 1).
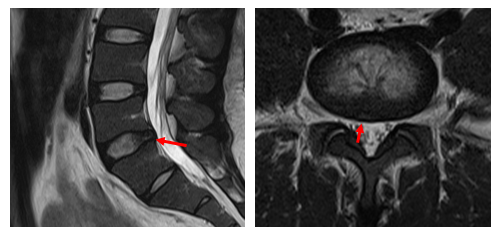
Figure 1: Pre-OP sagittal (left) and axial (right) T2 weighted MRI for Patient 01-017. Red arrows indicating annular tear.
A partial sacralization of the L5 vertebra and bilateral Bertolotti’s joints was also present. All other disc levels were very well preserved with Pfirrmann grade 1. On weight bearing radiographs, there was mild scoliosis with no signs of instability on dynamic views. At L4-5, there was segmental range of motion of 20.3 degrees, 11.8 mm of disc height, and 2.0 mm of antero-posterior translational motion.
On standard patient-reported questionnaires, the patient demonstrated severe disability (Table 1). He was identified by the treating surgeon as a potential candidate for enrollment into LOPAIN1 (Lumbar Operatively Inserted PerQdisc Artificial Implant following Nuclectomy), a Phase 1 prospective clinical trial designed to test the safety profile of a novel nucleus replacement device, based on the clinical presentation, annular disc defect on MRI, and the enrollment algorithm (Figure 2). The patient was approved by the Medical Advisory Board and underwent a left-sided anterior retroperitoneal approach, nuclectomy and implantation of the PerQdisc nucleus replacement device.
|
PROM |
Baseline |
At 2-year follow up |
|
VAS-back |
80/100 |
1/100 |
|
VAS-leg |
20/100 |
1/100 |
|
Oswestry Disability Index |
80/100 |
0/100 |
|
SF12 – Physical Component |
26.42 |
56.65 |
|
SF12 – Mental Component |
35.78 |
55.86 |
Table 1: Patient Reported Outcome Measures (PROMs) including Visual Analogue Scale for back and leg pain, Oswestry Disability Index and physical and mental components at Pre-OP and 2 years after the surgery.
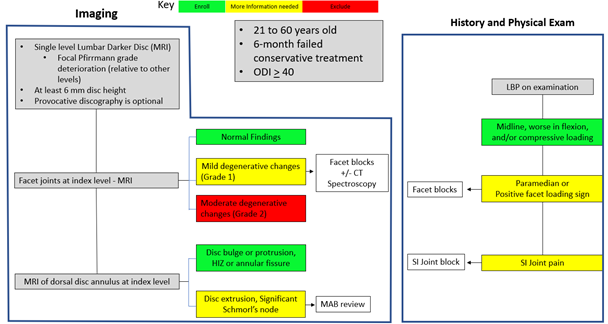
Figure 2: Clinical Assessment Algorithm for enrollment of patients into the LOPAIN1 clinical trial considering patient´s imaging, demographics, history and their physical exam.
A standard PerQdisc procedure was performed on Apr 17, 2021 using an anterior retroperitoneal approach, in the supine position, to gain access to the L4/5 intervertebral disc. Dissection was straightforward to expose 1 cm² of the anterolateral surface area of the annulus. Exposure was maintained using the Phantom AL ™Retractor by TeDan Surgical Innovations. Sequential dilation was used to minimize trauma and access the nucleus pulposus. A nuclectomy was performed through the stoma using different rongeurs. Imaging balloon devices were used to confirm sufficient nuclectomy and disc space integrity before the final implant was positioned and filled with a room temperature vulcanizing silicone polymer. The instruments were removed after 10 minutes of curing time and a multilayered closure was performed.
The patient had a smooth postoperative recovery. He was discharged at POD 2 and progressively improved his overall function[4]. He returned to work on Jun 7, 2021. At the 2-year follow up period his pain scores had improved significantly. At 2-year follow up, dynamic radiographs demonstrated 23.4 degrees of segmental motion with no suggestion of inflammation on MRI (Figure 3).
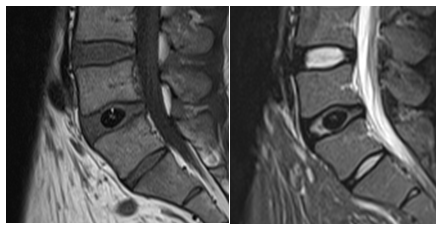
Figure 3: Lumbar sagittal T1 (left) and T2 MRI (right) at the 24 Months Follow-Up timepoint for patient 01-017.
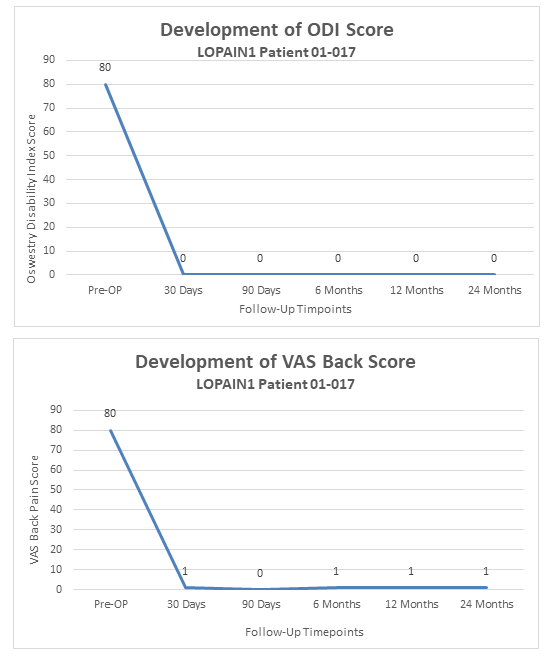
Figure 4: Graphical development of Oswestry Disability Index (left) and Visual Analogue Scale for Back Pain (right) over 24 Months. X-axis showing follow-up timepoints where patients status was assessed. Y-axis showing score value on scale from 0-100.
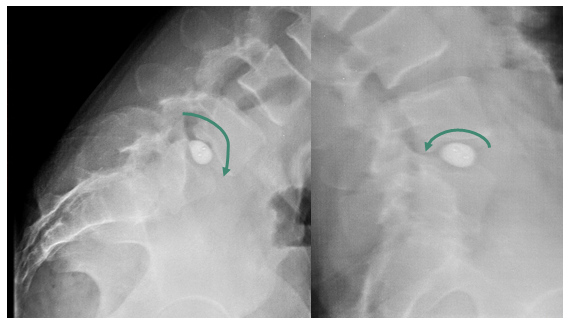
Figure 5: Dynamic radiographs showing behavior of PerQdisc implant under flexion (left) and extension (right) movements at the 24 Months follow-up timepoint for patient 01-017.
Discussion
The biggest challenge of treating dLBP is making the correct diagnosis. Normal degenerative changes to the disc and other spinal elements are very common and differentiating such changes from pathological manifestations is radiologically difficult and unreliable making diagnosis of dLBP difficult. Additional diagnostic tools have been utilized in the past in making the correct diagnosis and physicians have mostly relied on provocative discography, intradiscal anesthetic blocks, and MR-spectroscopy[9][10][11] which are cause of significant debate and discord among experts[12]. As such, dLBP is largely diagnosed today by clinical suspicion and excluding other more tangible sources of pain, such as facet joint inflammation, nerve root compression, mechanical instability, and SI-joint dysfunction.
The treatment for dLBP includes physical therapy to improve biomechanics and pharmaceutical management to reduce pain and inflammation. Multiple types of intradiscal injection therapies have not had reliable results[8]. Some spinal societies recommend against the surgical treatment of dLBP[5] but nonetheless, some patients have convincing clinical presentations. Current surgical treatments target the total removal of disc material and/or the elimination of disc motion, through either various fusion techniques or total disc replacement. Multiple efforts have been made to develop selective nucleus disc replacement devices, but none are commercially available[8].
Spinal Stabilization Technologies™ developed the PerQdisc™ Nucleus Replacement System as a surgical alternative to fusion and total disc replacement in patients with dLBP. The PerQdisc replaces the physical space of the nucleus, in an attempt to recreate physiological motion, and redistribute the weight bearing forces and mechanical properties of the disc in a more natural fashion. It is presumed to treat dLBP by removing the damaged nucleus tissue, while the nucleus replacement implant supports the annulus fibers and nearby tissues. It can be implanted anteriorly via a retroperitoneal approach or laterally via a transpsoas approach and a posterolateral access via a minimally invasive percutaneous approach through Kambin’s triangle is currently being evaluated in clinical studies. The PerQdisc is only available through clinical trial enrollment. Similar devices have demonstrated long-term efficacy[13] but have also been fraught by high failure rates, including subsidence, migration and expulsion[14][15][16]. Nonetheless, a true nucleus replacement device would represent a major engineering and medical feat as an ideal solution for many patients suffering from dLBP, as showcased in this clinical case report. While such results are encouraging, the challenge of reliability, clinical safety, and broad use of such devices will depend entirely on diagnostic accuracy and carefully designed clinical trials, which are underway.
Conclusion
This case demonstrates successful diagnosis of dLBP and surgical treatment using a novel motion-sparing and form-fitting nucleus replacement device, in the context of a clinical trial. While the diagnostic criteria used in this case report may be a useful guide to identify other patients with dLBP, the surgical treatment offered should be interpreted with caution until appropriate clinical trials are presented.
Conflict of Interest Statement:
Funding for this study was provided by Spinal Stabilization Technologies (SST). Authors 1, 2 & 3 have received honoraria from SST. Authors 4 and 5 are employees of SST.
National Competent Authority:
Paraguay Ministry of Health
References
- Collaborators, GBD 2015 Disease and Injury Incidence and Prevalence. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388 (2016): 1545-1602.
- Adams PhD, Michael A. and Roughley PhD, et al. What is Intervertebral Disc Degeneration, and What Causes It? Spine 31 (2006): 2151-2161.
- Erwin DC PhD, W. Mark and Hood DC, et al. The cellular and molecular biology of the intervertebral disc: A clinician´s primer. The Journal of the Canadian Chiropractic Association 58 (2014): 246-257.
- Peng MD, PhD, Boagan, et al. Possible Pathogenesis of Painful Intervertebral Disc Degeneration. Spine 31 (2006): 560-566.
- Airaksinen O, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. European Spine Journal 2 (2006): 192-300.
- Bertagnoli MD, Rudolf, Karg MSc, et al. Lumbar Partial Disc Replacement. Orthopedic Clinics of North America 36 (2005): 341-347.
- Pimenta MD PhD, Luiz, et al. Lessons Learned After 9 Years’ Clinical Experience with 3 Different Nucleus Replacement Devices. Seminars in Spine Surgery 1 (2012): 43-47.
- Raley, Thomas J, Bao, et al. Nucleus Augmentation (2017).
- Taher, Fadi, et al. Lumbar Degenerative Disc Disease: Current and Future Concepts of Diagnosis and Management. Advances in Orthopedics (2012).
- Cohen, Steve P, et al. Lumbar discography: a comprehensive review of outcome studies, diagnostic accuracy, and principles. Regional anesthesia and pain medicine 30 (2005): 163-183.
- Gornet, Matthew F, et al. Magnetic resonance spectroscopy (MRS) identification of chemically painful lumbar discs leads to improved 6 , 12 , and 24 month outcomes for discogenic low back pain surgeries. European Spine Journal. Online ahead of print 32 (2023): 1973-1984.
- Staartjes BMed, Victor E, et al. Identifying subsets of patients with single-level degenerative disc disease for lumbar fusion: the value of prognostic tests in surgical decision making. The Spine Journal 18 (2018): 558-566.
- Golan MD, Jeff D, et al. Long-Term Outcomes Following Lumbar Nucleus Replacement. International Journal of Spine Surgery 15 (2022): 1096-1102.
- Rosales-Olivares, LM. Experience with prosthetic disc nucleus device in Mexico. Final report of a 4-year folllow-up. Cirugia y cirujanos. 75 (2007): 31-36.
- Beaubien BP, Freemann AL and Sherman TN. Subsidence characteristics of two nucleus replacement devices compared to a PEEK interbody fusion device. Spine Arthroplasty Society (SAS) 1(2007): 52-57.
- Schnake KJ, Weigert F and Kandziora, F. Local vertebral body destruction after migration of a nucleus replacement. Zeitschrift für Orthopädie und Unfallchirurgie 145 (2007): 649-651.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 