Survey on Spinal Injections for lumbar degenerative stenosis among spine surgeons in Latin America
Marcelo Molina1,2,5*, Ramon Torres2,3, Ratko Yurac1,6, Samuel Pantoja4, Lucio Gonzales2
1Orthopedic Surgery dept, Spine Surgery Unit, Clínica Alemana, Santiago, Chile
2Orthopedic Surgery dept, Spine Surgery Unit, Instituto Traumatológico, Santiago, Chile
3Orthopedic Surgery dept, Spine Surgery Unit, Clínica Santa María, Santiago, Chile
4Orthopedic Surgery dept, Spine Surgery Unit, Clínica Universidad de los Andes, Santiago, Chile
5Universidad Finis Terrae, School of Medicine
6Universidad del Desarrollo, School of Medicine
*Corresponding Author: Marcelo Molina, Orthopedic Surgery dept, Spine Surgery Unit, Clínica Alemana, Santiago, Chile.
Received: 09 October 2023; Accepted: 16 October 2023; Published: 09 November 2023
Article Information
Citation: Marcelo Molina, Ramon Torres, Ratko Yurac, Samuel Pantoja, Lucio Gonzales. Survey on Spinal Injections for lumbar degenerative stenosis among spine surgeons in Latin America. Journal of Spine Research and Surgery. 5 (2023): 96-105.
View / Download Pdf Share at FacebookAbstract
Introduction:
Epidural and facet joint injections are usually used as part of the treatment algorithm for low back and radicular pain. Current clinical practice in Latin America is not well described in the literature.
Objectives:
Evaluate the indications and techniques of spinal injections (SI) in patients with degenerative lumbar spinal stenosis (DLSS) among spine surgeons in Latin America.
Study Design:
Cross-sectional, international survey, narrative literature review.
Methods:
An online survey was sent to spine surgeons and members of the AOSpine Latin America. Data included surgeon geographic information, specialty, time in professional activity, SI indications, and techniques in different scenarios of pain and stenosis localization.
Results:
A total of 446 surgeons, 291 (65%) orthopedic surgeons, and 155 (35%) neurosurgeons replied to the survey. 92% of spine surgeons indicated a spinal steroid injection to treat DLSS. Most spinal surgeons (54%) would simultaneously perform both peridural and intraarticular lumbar facet (combined) steroid injections in patients with low back pain and radicular pain. Foraminal injection is a preferred technique for patients with central and foraminal stenosis. There are no significant differences in most of the answers between orthopedic surgeons and neurosurgeons. Almost 80% of respondents expect a good result from the injection. However, 86% of surgeons believe injection effects last less than 6 months, and only 12% think surgery will not be necessary in the future. Only 15% of spine surgeons irrespective of specialty adhere to a guideline on spine injections for DLSS.
Conclusion:
This study provides a global perspective on how Latin American spine surgeons treat patients with DLSS concerning the use of spinal steroid injections. We observed that more than 90% of respondents use this procedure to treat DLSS. There are almost no differences between orthopedic spine surgeons and neurosurgeons when performing SI. A foraminal injection is preferred for lateral recess and foraminal stenosis. Most of the respondents expect to achieve positive results with the procedure, but they believe that its effect will last for less than 6 months and possible need for surgery.
Keywords
<p>Survey; spinal stenosis; spinal injection; lumbar; degenerative; sciatic pain; spine surgery; spine surgeon</p>
Article Details
Introduction
Lumbar spinal stenosis is defined as the narrowing of the cross-sectional area of the spinal canal, localized at the central canal, lateral recess or foraminal space, and frequently generates an encroachment on the neural structures [1-4].
Degenerative changes of the spine are the most common etiology of lumbar spinal stenosis and it is considered the most frequent cause of radicular pain and neurogenic claudication in the population over 60 years old [1].
The natural history of degenerative lumbar spinal stenosis (DLSS) tends to be benign in terms of progression rate; almost 70% of the patients report no changes in their symptoms at 4 years of following [3]. Nevertheless, almost 30% of patients present progression of symptoms, leading to severe pain and functional impairment. Lumbar stenosis leads to inflammation of the nerve root resulting from compression, usually presenting as mono or multi-radicular pain, and frequently with both axial and leg pain.
Another established cause of chronic back pain is facet joint inflammation, with an incidence of 15 to 45% in the general population [1]. Facet joint arthropathy and synovitis may present with axial or buttock pain. Both facet joint arthropathy and DLSS are usually present at the same time in the degenerative spine, making it sometimes difficult to identify the specific origin of pain [5]
Initial treatment includes oral pain medication and physical therapy. If symptoms persist, spinal corticosteroid injections can be considered [6,7]. Corticosteroids can inhibit edema in mechanically compressed nerve roots exhibiting microlesions, decrease inflammation by altering leukocyte function through stabilization of lysosomal membranes, reduce the activity of phospholipase A2 and block nociceptive transmission in C fibers.
There are different types of spinal injections (SI) depending on the predominant pathology, and they can be divided into 2 groups: facet joint injections and epidural injections. The latter can be subdivided in 3 depending on the route of administration: interlaminar, transforaminal and caudal. An epidural injection is indicated when it is suspected that axial and or radicular pain are associated to stenosis of the lumbar canal. Facet joint injections are indicated in patients in which the facets are considered as the origin of the symptoms [6].
Despite a moderate and low level of evidence, there are some guidelines and consensus concerning the use of corticosteroid injections in DLSS [4,6,7]. However, substantial heterogenicity in interventions regarding timing, number of injections and patient selection is found in the literature. More importantly, to our knowledge, there is no specific evidence-based clinical guideline that defines when it is advisable to perform a facet infiltration over an epidural injection or when it is reasonable to perform both in DLSS pathology.
Our main goal was to evaluate the indications and techniques for spinal injections in DLSS of spinal surgeons in Latin America, with particular attention to indications and preference of single or combined injection techniques. Our secondary goal was to review the literature available regarding epidural and facet corticosteroid injection in the treatment of DLSS.
Methods
Study Design
Prospective, therapeutic opinion survey. Cross-sectionally study using a purpose-built electronic survey. Narrative review.
Population studied
An electronic questionnaire was created by the authors to evaluate spinal injection use in DLSS among spine surgeons in Latin America (LA). This was distributed to LA members of AOSpine. AOSpine is an internationally-recognized professional community of spine physicians and investigators with a total of 6.403 members, 1.288 from LA. The survey respondent characteristics are resumed in Table 1.
An e-mail request to participate in the survey was sent to all LA members, accompanied by a cover letter explaining study objectives and a link to the survey, created in Survey Monkey software. Portuguese and Spanish versions of the questionnaire were created. This link was made available for 14 days, during which up to three reminder emails were sent to non-respondents.
|
Survey respondent characteristics |
||
|
n |
% |
|
|
Total |
446 |
100 |
|
Specialty |
||
|
Neurosurgeon |
155 |
34.75 |
|
Orthopedic surgeon |
291 |
65.25 |
|
Time of professional activity in spine surgery |
||
|
Less than 5 years |
75 |
16.82 |
|
Between 5 and 10 years |
91 |
20.4 |
|
Between 10 and 15 years |
94 |
21.08 |
|
Between 15 and 20 years |
79 |
17.71 |
|
More than 20 years |
107 |
23.99 |
|
Country |
||
|
Argentina |
113 |
25.34 |
|
Brazil |
100 |
22.42 |
|
Chile |
60 |
13.45 |
|
Mexico |
60 |
13.45 |
|
Colombia |
34 |
7.62 |
|
Other* |
79 |
17.71 |
*Uruguay, Paraguay, Panama, Guatemala, Ecuador, Dominican Republic and Costa Rica
Table 1: Survey respondent characteristics
Assessment
Assessment was based on a questionnaire consisting of 19 multiple-choice questions addressing indications and technique chosen depending on the location of the dominant pain (lumbar or radicular) and on location of the pathology (central, lateral recess or foraminal stenosis). The survey also included outcome expectations and complications of this procedure. The questions included in the questionnaire are presented in Table 2.
|
Survey on Spinal Injections for lumbar degenerative stenosis questionary |
||
|
Questions |
Response options |
|
|
1 |
Time of professional activity in spine surgery |
Less than 5 years |
|
Between 5 and 10 years |
||
|
Between 10 and 15 years |
||
|
Between 15 and 20 years |
||
|
More than 20 years |
||
|
2 |
Specialty |
Orthopedic Surgeon |
|
Neurosurgeon |
||
|
3 |
Country where you work |
|
|
4 |
What percentage of your patients with lumbar degenerative stenosis (DLSS) with significant radicular pain and failure to conservative treatment you perform a spinal steroid injection? |
Never |
|
1 to 25% |
||
|
26 to 50% |
||
|
51 to 75% |
||
|
76 to 100% |
||
|
5 |
In a patient with symptomatic DLSS with sciatic or leg pain without significant pain relief after conservative treatment, for how long you maintain conservative treatment before considering a spinal steroid injection? |
Less than 1 week |
|
Between 1 and 2 weeks |
||
|
Between 2 and 4 weeks |
||
|
Between 1 and 3 months |
||
|
I never perform or indicate spinal injections |
||
|
6 |
In a patient with DLSS with significant low back pain and radicular pain do you perform: |
Peridural steroid injection |
|
Intraarticular lumbar facet steroid injection |
||
|
Both injections in the same opportunity |
||
|
I never perform or indicate spinal injections |
||
|
7 |
In a patient with DLSS with significant low back pain without radicular pain you perform: |
Peridural steroid injection |
|
Intraarticular lumbar facet steroid injection |
||
|
Both |
||
|
I never perform or indicate spinal injections |
||
|
8 |
In a patient with DLSS with significant radicular pain without (or minimal) low back pain you perform: |
Peridural steroid injection |
|
Intraarticular lumbar facet steroid injection |
||
|
Both |
||
|
I never perform or indicate spinal injections |
||
|
9 |
In a patient with DLSS and lumbosciatic pain secondary to nerve root compression in the lateral recess area, if you decide to perform a spinal injection which technique would you use? |
Interlaminar steroid injection |
|
Foraminal steroid injection (or selective nerve root block/injection) |
||
|
Caudal steroid injection |
||
|
I never perform or indicate spinal injections |
||
|
10 |
In a patient with DLSS and lumbosciatic pain secondary to nerve root compression in the foramina, if you decide to perform a spinal injection which technique would you use? |
Interlaminar steroid injection |
|
Foraminal steroid injection (or selective nerve root block/injection) |
||
|
Caudal steroid injection |
||
|
I never perform or indicate spinal injections |
||
|
11 |
In a patient with DLSS and neural claudication secondary to central spinal stenosis, if you decide to perform a spinal injection which technique would you use? |
Interlaminar steroid injection |
|
Foraminal steroid injection |
||
|
Caudal steroid injection |
||
|
I never perform or indicate spinal injections |
||
|
12 |
In what percentage (in average) of your patients would you expect a good result (defined as a relief of more than 50% of the pain)? |
0 to 20% |
|
21 to 40% |
||
|
41 to 60% |
||
|
61 to 80% |
||
|
81 to 100% |
||
|
13 |
For how long (in average) do you expect a good result (defined as a relief of more than 50% of the pain) with the spine injection? |
Less than 1 month |
|
Between 1 and 3 months |
||
|
Between 3 and 6 months |
||
|
Between 6 month and 1 year |
||
|
More than 1 year |
||
|
14 |
What percentage of your patients in which you perform a spine injection due to DLSS you believe will not require surgery in the future? |
0 to 20% |
|
21 to 40% |
||
|
41 to 60% |
||
|
61 to 80% |
||
|
81 to 100% |
||
|
15 |
You think the best result of an intraarticular lumbar facet steroid injection is when in the MRI you see: |
Significant facet joint fluid (more than 1.5 mm) |
|
Facet Synovitis |
||
|
Severe facet osteoarthritis |
||
|
Any of the above |
||
|
Results depend on clinical presentation, not MRI findings |
||
|
16 |
Do you think the addition of intraarticular lumbar facet steroid injection significantly improves the result of an epidural steroid injection to relief the pain in a patient with DLS? |
Yes |
|
No |
||
|
I do not combine both injections |
||
|
17 |
Select the 3 most frequent effect adverse of the spinal injection including intraarticular lumbar facet steroid injection and peridural interlaminar steroid injection |
Insomnia |
|
Hiccup |
||
|
Allergic reaction |
||
|
Facial Flushing |
||
|
Headache |
||
|
Peridural hematoma |
||
|
Infection |
||
|
Pain in the punction site |
||
|
Vaso vagal reaction |
||
|
18 |
In a patient with DLSS how many spine injections you would perform (repeat procedure) if you obtain a good pain relief with them before suggesting surgery? |
None |
|
1 injection |
||
|
2 injections |
||
|
3 injections |
||
|
4 or more |
||
|
19 |
Are you aware of valid guidelines on spine injections for DLSS? |
No |
|
Yes, and I adhere to them |
||
|
Yes, but I do not always adhere to them (do not consider them always valid) |
||
Table 2: Survey on Spinal Injections for lumbar degenerative stenosis questionary
Statistical Analysis
The survey data was compiled in Excel spreadsheet files. The study sample was described by calculating the frequencies and percentages for categorical variables. The statistical analysis was performed using the Pearson χ2 analysis. Key questions were analyzed according to countries, specialty (neurosurgery versus orthopedic surgery) and years of practice. p < 0.05 was considered to be statistically significant. All analyses were performed using Minitab18 and RStudio Version 1.1.383.
Results:
Sample characteristics
Responses were received from 446 surgeons, including 291 (65.25%) orthopedic surgeons and 155 (34.75%) neurosurgeons. The majority of respondents had more than 10 years of professional activity in spine surgery (62.7%) (Table 1). The largest number of responses were from Argentina (25.34%), Brazil (22.42%), Chile (13.45%) and Mexico (13.45%) (Figure 1).
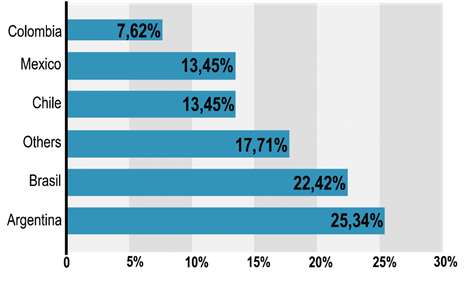
Figure 1: Overall responses by country.
Spinal infiltration indication
Regarding current practices, 92.5% of spine surgeons performed a spinal steroid injection in patients with DLSS, with no difference between orthopedic surgeons (96%) and neurosurgeons (84%) (Table 3, Figure 2).
As to the number of SI, 59% of spine surgeons would perform up to 2 injections if they obtain a good result on the first procedure. Only 4% would infiltrate 4 or more times in the same scenario (Figure 3).
Regarding timing, 70 % of the spine surgeons surveyed waited for more than 2 weeks of conservative treatment before indicating a SI and 38% waited more than 1 month (Figure 4).
Only a 14.8% of spine surgeons, irrespective of specialties replied they followed the indications of an epidural/facet injection guideline (Figure 5).
|
What percentage of your patients with lumbar degenerative stenosis (DLSS) with significant radicular pain and failure to conservative treatment you perform a spinal steroid injection? |
||||||||
|
Specialty % |
Country % |
|||||||
|
Options |
NS |
OS |
Argentina |
Brazil |
Chile |
Colombia |
Mexico |
Other* |
|
1% to 25% |
30.97 |
29.9 |
14.16 |
37 |
23.33 |
8.82 |
48.33 |
45.57 |
|
26% to 50% |
26.45 |
24.05 |
25.66 |
30 |
23.33 |
29.41 |
21.67 |
18.99 |
|
51% to 75% |
17.42 |
23.37 |
31.86 |
16 |
31.67 |
32.35 |
6.67 |
11.39 |
|
76% to 100% |
9.68 |
19.24 |
24.78 |
10 |
16.67 |
23.53 |
11.67 |
10.13 |
|
Never |
15.48 |
3.44 |
3.54 |
7 |
5 |
5.88 |
11.67 |
13.92 |
*Uruguay, Paraguay, Panama, Guatemala, Ecuador, Dominican Republic and Costa Rica with less than 7% of representation. NS, neurosurgeon; OS, orthopedic surgeon.
Table 3: What percentage of your patients with lumbar degenerative stenosis (DLSS) with significant radicular pain and failure to conservative treatment you perform a spinal steroid injection?
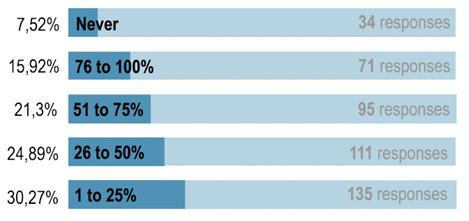
Figure 2: What percentage of your patients with DLSS with significant radicular pain and failure to conservative treatment you perform a steroid injection?
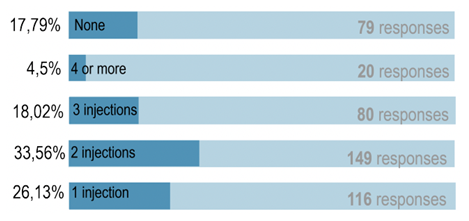
Figure 3: In a patient with DLSS, how many spine injections would you perform (repeat procedure) before suggesting surgery?
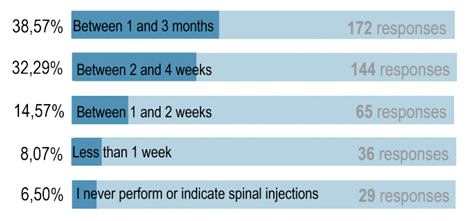
Figure 4: In a patient with symptomatic DLSS with sciatic pain without significant pain relief after conservative treatment, for how long do you maintain conservative treatment before considering a spinal steroid injection?
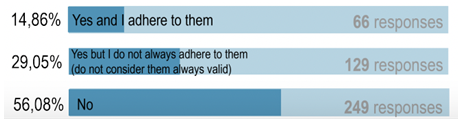
Figure 5: Do you follow the indications of any epidural or facet joint infiltration guidelines?
Spinal infiltration type
As for the type of injection performed, 54% of spine surgeons would indicate both peridural and intraarticular lumbar facet steroid injections in patients with low back pain and radicular pain, with no difference between orthopedic surgeons and neurosurgeons (Figure 6). After analyzing the distribution by country, it was found that 81.7% of spine surgeons in Chile would perform both spinal infiltration types to treat patients with radicular pain and low back pain (p<.001).
In patients with low back pain without radicular pain, 54% of the surgeons would perform only a facet steroid injection (Figure 7).
In case of patients with radicular pain and no low back pain, 55.6% of the surgeons would perform a peridural injection without facet injection, with no significant differences between orthopedic and neurosurgeons. In the same scenario, 10% of neurosurgeons and 24% of orthopedic surgeons (p=0.018) would indicate an injection of both peridural and intra-articular lumbar facet steroid injection, with significant difference between specialties (Table 4).
|
Spinal infiltration type performed for different pain scenarios |
||||||||
|
Peridural steroid injection |
Intraarticular lumbar facet steroid injection |
Both |
I never perform or indicate spinal injections |
|||||
|
Scenarios |
NSU |
OS |
NSU |
OS |
NSU |
OS |
NSU |
OS |
|
Low back pain and radicular pain |
27.74 |
23.02 |
10.32 |
12.03 |
45.81 |
59.79 |
16.13 |
23.02 |
|
p = 0.546 |
p = 0.873 |
p = 0.066 |
p = 0.022 |
|||||
|
Low back pain without radicular pain |
14.19 |
11.68 |
53.55 |
54.3 |
12.26 |
18.9 |
20 |
15.12 |
|
p = 0.750 |
p = 1.000 |
p = 0.27 |
p = 0.471 |
|||||
|
Radicular pain and no low back pain |
54.84 |
56.01 |
9.03 |
6.19 |
10.97 |
24.74 |
25.16 |
13.06 |
|
p = 0.981 |
p = 0.624 |
p = 0.018 |
p = 0.046 |
|||||
a Calculation of P values was performed using Χ2 test. Abbreviations: NSU, neurosurgeon; OS, orthopedic surgeon. Bolded value indicates statistical significance at P<.05
Table 4: Spinal infiltration type performed for different pain scenarios
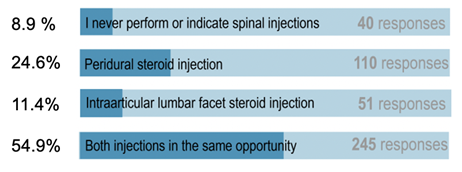
Figure 6: In a patient with DLSS with significant low back and radicular pain what do you perform?
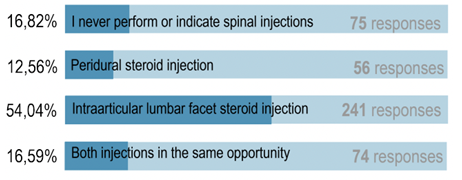
Figure 7: In patients with DLSS with significant low back pain without radicular pain, what do you perform?
Spinal infiltration technique
Regarding techniques employed according to stenosis location, the vast majority of spine surgeons (85%) would use a foraminal steroid injection technique in patients with DLSS and sciatic pain secondary to nerve root compression in the lateral recess area (Figure 8). Similar trends were observed in patients with DLSS and sciatic pain secondary to nerve root compression in foraminal space (69%) (Figure 9).
For patients with central canal stenosis, 37% of spine surgeons performed an interlaminar steroid injection. In this group, 26% decide against a spinal injection (Figure 10).
Significant differences were observed between specialties when selecting to never indicate a spinal infiltration technique for foraminal (p=0.036) and also for central (p=0.049) stenosis location (Table 5), neurosurgeons indicate a spinal injection less often.
|
Spinal injection technique according to stenosis location |
||||||||
|
Interlaminar |
Foraminal |
Caudal |
None |
|||||
|
Stenosis location |
NSU |
OS |
NSU |
OS |
NSU |
OS |
NSU |
OS |
|
Lateral recess area |
4.52 |
4.12 |
66.45 |
70.79 |
15.48 |
19.93 |
13.55 |
5.15 |
|
p = 1.000 |
p = 0.610 |
p = 0.523 |
p = 0.070 |
|||||
|
Foraminal |
4.52 |
4.47 |
78.71 |
89.35 |
3.23 |
2.06 |
13.55 |
4.12 |
|
p = 1.000 |
p = 0.063 |
p = 0.940 |
p = 0.036 |
|||||
|
Central |
29.03 |
41.58 |
5.16 |
9.97 |
30.97 |
27.15 |
34.84 |
21.31 |
|
p = 0.088 |
p = 0.308 |
p = 0.660 |
p = 0.049 |
|||||
Calculation of P values was performed using Χ2 test. Abbreviations: NSU, neurosurgeon; OS, orthopedic surgeon. Bolded value indicates statistical significance at P<.05
Table 5: Spinal injection technique according to stenosis location
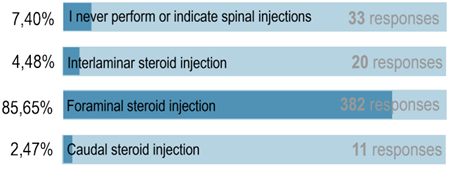
Figure 8: In a patient with DLSS and lumbosciatic pain due to compression in the lateral recess area, if you decide to perform a spinal injection, which technique would you use?
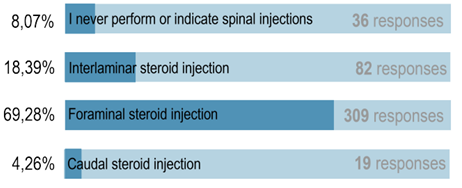
Figure 9: In a patient with DLSS and lumbosciatic pain due to compression in the foramina, if you decide to perform a spinal injection, which technique would you use?
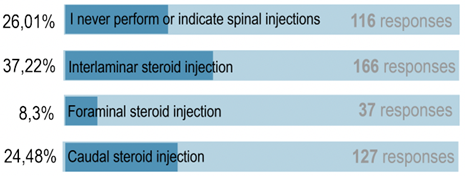
Figure 10: In a patient with DLSS and lumbosciatic pain due to compression in the central canal, if you decide to perform a spinal injection, which technique would you use?
Procedure expectations
78% of the spine surgeons expected a good outcome (defined as a relief of more than 50% of the pain) with a SI in over 40% of the patients (Figure 11). Also, 86% of the spine surgeons expected the effects to last no longer than 6 months and 59% not more than 3 months (Figure 12). Only 12% of spine surgeons believe that more than 60% of patients with DLSS will prevent the need for surgery in the future with SI (Figure 13).
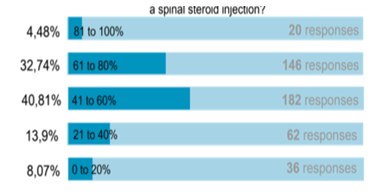
Figure 11: Thhe spine surgeons expected a good outcome (defined as a relief of more than 50% of the pain) with a SI in over 40% of the patients

Figure 12: For how long do you expect a good result (pain relief > 50%) with the spine injection?
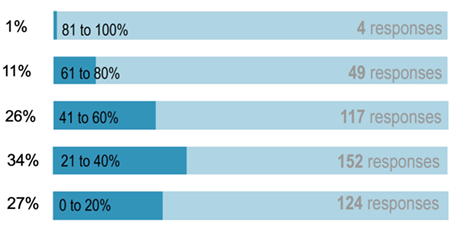
Figure 13: What percentage of your patients in which you perform a spine injection due to DLSS will not require surgery in the future?
Facet Joint Steroid Injections
Almost 50% of the surgeons believed that the results of an intraarticular lumbar facet steroid injection depend on clinical presentation, not on MRI findings. The other 50% think that results depend on facet synovitis (24%), severe facet osteoarthritis (15%) or significant facet joint fluid (11%) as seen in the MRI (Figure 14).
63% of the surgeons believed that adding an intraarticular lumbar facet steroid injection significantly improved the results of an epidural steroid injection in a patient with DLSS. In the other hand, 36% of respondents think it has no impact on the improvement of pain relief (Figure 15)
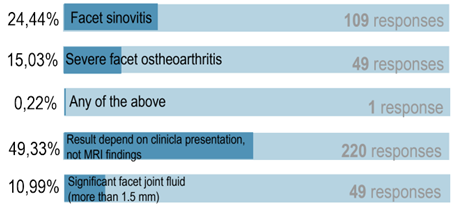
Figure 14: The best result of an intra-articular lumbar facet steroid injection is when the MRI shows
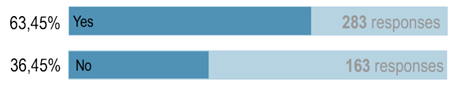
Figure 15: Do you think that the addition of an intra-articular facet steroid injection significantly improves the results of an epidural steroid injection in terms of pain relief in the DLSS patient?
Complications
The 3 most frequent adverse effects from SI, including both intraarticular lumbar facet and epidural steroid injections, was pain in the punction site (70%), cephalea post punction (38%) and vasovagal reaction (26%). Less frequent were facial flushing, allergic reaction, infection and insomnia (Figure 16).
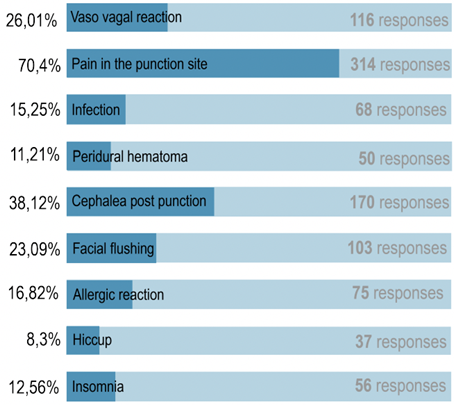
Figure 16: Select the 3 most frequent adverse effects of spinal injection (including facet and epidural steroid injection)
Discussion:
DLSS is one of the most common causes of low back and radicular pain in older adults. According to the Framingham study cohort, a 4% prevalence of absolute lumbar stenosis was found in those under 40 years of age, increasing to 19.4% in patients between 60 to 69 years [1]. Conservative management is considered the initial treatment, except in rare situations such as progressive neurological deficit or cauda equina syndrome. Conservative treatment consists of physical therapy, analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids [4]. When the clinical response is insufficient, the use of epidural injections of corticosteroids plus local anesthetics can be considered as a treatment option [7,8].
The North American Spine Society (NASS) guidelines indicate that in patients with radiculopathy or claudication due to DLSS, short-term pain relief can be achieved with an epidural injection regimen [3]. The American Society of Interventional Pain Physicians (ASIPP) published an extensive evidence-based guideline regarding epidural interventions in the management of chronic spinal pain. Their recommendation in LSS is moderate to strong for interlaminar and caudal epidural injections, and moderate in foraminal injections, all for long-term improvement [7]. A recent meta-analysis comparing surgical treatment versus conservative treatment, including the SPORT cohort, fails to conclude which treatment is better in both groups and cannot offer a clinical recommendation, but clarifies that surgical treatment presents rates of complications and collateral effects between 10% to 24% of cases, with no collateral effects or complications in the case of non-surgical treatment [2]. Considering this information, it is to be expected that a large number of patients will choose to undergo spinal injections before considering surgical treatment. On the other hand, the 2016 National Institute for Health and Care Excellence (NICE) guidelines, which include 20 RCTs, recommend against the use of epidural injection in the setting of central canal stenosis, since they found that there was no evidence for any of the critical outcomes in the sciatica caused by spinal stenosis [4]. In our survey, we found that 92.5 % of spine surgeons would perform an SI in patients with DLSS who do not respond to conservative treatment.
There is no agreement on the recommended period of conservative treatment in before indicating a spinal injection in DLSS. Some trials performed 2 to 4 weeks before an epidural injection [9,10]. The 2013 NASS guidelines indicate that the use of epidural corticosteroids can provide short-term pain relief (2 to 6 weeks) in patients with radicular pain and neurogenic claudication secondary to DLSS, with a type B grade of recommendation [4], but they do not give any recommendation regarding conservative treatment and its duration. In our survey, 70.8 % of spine surgeons wait for more than 2 weeks before performing a corticosteroid injection and 38.5% wait more than 1 month.
As commented before, facet joint arthropathy is one of the most common causes of low back pain. Frequently, both facet joint arthropathy and DLSS are usually present at the same time in the degenerative spine, and the physician should try to identify the specific origin of the pain based on its clinical characteristics and images [6]. Since this differentiation is quite difficult in some cases, or the origin of the pain is probably mixed, in clinical practice the use of an epidural and facet injection may be combined.
There is some evidence to support the use of facet injections in patients with DLSS. Hwang et al. [11] described that the use of facet infiltration in patients with DLSS and radiculopathy was effective for pain relief in 59.5% of patients with follow-up at 145 days. Shim et al. [12] report that 66% of patients with DLSS who received sequential infiltrations with corticosteroids, either epidural or facet joint infiltration, opted for a facet joint infiltration as a third procedure. In addition, they found that 68.4% of patients who experienced an “ineffective” first epidural injection perceived the second facet injection as “effective” for the pain relief. The retrospective study by Park et al. [13] found that 45% of DLSS patients who received facet injection had more than 30% of pain relief post-procedure. In our study, 63% of the surgeons think that the addition of intraarticular lumbar facet steroid injection significantly improves the result of an epidural steroid injection to relieve the pain in a patient with DLSS, but 36% think it is not effective in obtaining a good result. However, when presented with the case of a patient with radicular pain and no low back pain, 55.6% of the spine surgeons surveyed would opt for an epidural injection without facet injection. On the other hand, when the patient presented both, radicular and low back pain, 54.9% of the surgeons would indicate both peridural and facet steroid injection. Analysis of distribution by countries revealed that 81.7% of spine surgeons from Chile would perform both spinal infiltration types when treating patients with radicular pain and low back pain (p<.001).
When reviewing the literature available, we found contradictory evidence regarding the use of epidural corticosteroids in degenerative lumbar stenosis, with studies showing a favorable effect [7, 8, 14-20] and others in which pain reduction is insufficient [14,21,22]. Part of this contradiction possibly is due to the heterogeneity or methodological laxity of some studies [23-25], in which patients with different degrees of severity are mixed, with insufficient classification of the severity of the pathology. Some studies also mix different techniques of spinal injection (caudal, interlaminar, and transforaminal) or even avoid standardizing the corticosteroid used [15]. All of this has already been highlighted by some authors who have drawn attention to the most important points in controversy in an effort to advise future publications [26,27].
The authors believe that the lack of specificity on the recommendations made in well-known guidelines such as NICE and NASS, in terms of timing, route of administration, and pathology involved plus these controversies found in the literature may be the reason why only a 14.7% of the surveyed surgeons claim to adhere to guidelines in DLSS pathology. Probably, the more recent evidence-based ASIPP guidelines could change this in the future [3,4,6,7].
Regarding the use of epidural corticosteroids in patients with central canal stenosis there is both evidence for and against a good outcome. To our best knowledge, the RCT by Manchiati et al. 2015 [8] represents the best evidence available, they studied 120 patients with central canal stenosis who presented low back and radicular pain for more than 6 months and no response to conservative treatment. In their study they compared epidural injections of local anesthetic versus local anesthetic plus betamethasone, finding significant relief and functional status improvement in 72% and 73% of patients in each group at 2 years follow-up. Manchikanti et al. 2014 [27] also found a 44% success rate when infiltrating corticosteroid plus local anesthetic via caudal and 73% via interlaminar. Do et al. 2020 [28] in contrast, describes that this is achieved only in 30% of patients with moderate central stenosis and 17.9% of the group with severe stenosis. Also, Olguner et al. 2020 [29] described that only 33.9% of patients who underwent transforaminal corticosteroid injections presented more than 50% pain relief at one year of follow-up.
When comparing transforaminal versus interlaminar techniques in DLSS, Smith et al. 2010 [30], found no difference in short-term pain improvement, long-term surgical interventions, or repeat injections between the two techniques. In 2020 Sencan et al. [31] published the results of their prospective study comparing bilateral TF and IL steroid injections in 72 patients with lumbar central canal stenosis. They reported better ODI and pain-free walking distance in the IL group at 3-month follow-up. However, the TF route showed better results in patients with more prominent neuropathic pain. As a counterpart, the meta-analysis of Wei et a. 2016 [32], including 931 patients with LSS from 9 RCT found that TF patients experienced superior pain relief compared with IL patients (p=0.01) but similar functional and ODI improvement between the two groups.
The meta-analysis by Meng et al 2015 [20] that included 13 randomized clinical studies with 1465 patients found a significant decrease in pain in 53.7% of the patients who received local anesthetic plus corticosteroid and 56.4% of those who received local anesthetic alone. Historically, the beneficial effect of epidural injection has been considered to be in the short and medium term [10,27,33]. However, as mentioned, there is evidence of good results up to 1 and 2 years of follow-up [7,8,14,34]. In the aforementioned meta-analysis by Meng [20], significant pain relief was found for 6.8 ± 4.6 months in the group with corticosteroids plus local anesthetic and for 7.8 ± 4.5 months in the group with local anesthetic alone.
In our survey, we defined a good result as pain relief greater than 50%. When asked about the outcome, 78% of surgeons expected to achieve a good result.. Interestingly, expectations of a good result did not exhibit a time pattern, with 23%, 36%, and 27% of those surveyed expecting a good result in their patients of less than 1 month, between 1 to 3 months, and between 3 to 6 months, respectively. When enquired about longer-term response to injections, 86% of spine surgeons would expect a good result for less than 6 months and 59% not more than 3 months. Only 1% of those surveyed believe that the effect could be longer than a year.
Regarding expectations of obtaining results leading to avoidance of surgery, only 12% of spine surgeons believe that over 60% of patients with DLSS will avoid future surgery. On this subject, the subgroup analysis of the SPORT study published by Radcliff et al. 2013 [35], found that 33% of patients with spinal stenosis who received epidural corticosteroids, chose to maintain conservative treatment during the first 3 months, and 42% of patients who received epidural corticosteroids and were initially assigned to conservative treatment, avoided surgery for the same period.
Side effects related to the use of corticosteroids tend to be minor and include facial flushing, low-grade fever, insomnia, anxiety, agitation, hyperglycemia, fluid retention, vasovagal reaction, nerve root injury, allergy, and temporary exacerbation of pain. Although serious complications from epidural infiltration with corticosteroids are uncommon, these have been reported [36-42]. They may result from the inadvertent puncture of the nerve root or spinal cord arteries and embolization by the use of particulate corticosteroids [12,43]. Other possible mechanisms of spinal cord damage could be puncture-induced vasospasm and direct compression caused by a hematoma or abscess [43]. According to our survey, the 3 most frequent adverse effects after epidural and facet injections with corticosteroids were: pain at the puncture site (70%), cephalea post punction (38%), and vasovagal reaction (26%).
Study strengths and limitations:
A strength of the current study is the high volume of respondents, frequently difficult to achieve, given typically low response rates among surgeons. Furthermore, the responses were from surgeons experienced in the management of these patients, both neurosurgeons and orthopedic surgeons. Respondents were recruited from a range of countries across Latin America, providing an adequate representation of the clinical practice in the region.
There are several limitations. First, 5 countries accounted for roughly 90% of the respondents, which implies that the overall results might not be generalizable to some of the under-represented countries. Second, the responses regarding clinical practice are not objectively verifiable, and the surgeon’s actual and perceived practice may differ. Finally, this survey aims to assess spinal surgeons' perception of spinal injections, not to evaluate their efficacy.
Conclusion
This study provides a global perspective on how Latin American spine surgeons manage patients with DLSS with respect to the use of spinal steroid injections. We observed that 92% of orthopedic surgeons and neurosurgeons would use this procedure to treat DLSS.
More than 50% of patients with low back pain and radicular pain receive a combination of intra-articular lumbar facet steroid injection and epidural steroid injection. Most answers show no significant differences between orthopedic spine surgeons and neurosurgeons in performing steroid injections on DLSS patients.
For lateral recess and foraminal stenosis, a foraminal injection is the preferred approach. Respondents expect positive results with injection, but the effects may last less than 6 months, and surgery may eventually be necessary for most patients.
Scientific evidence is fair for low back pain and radicular pain treated with spinal injections due to lumbar spinal stenosis with steroids. There is however no evidence-based guideline with strong recommendations for selecting a facet injection, a peridural injection or both. Better designed studies are needed to improve the quality of the current recommendations.
Acknowledgment:
This study was organized by the AO Spine Latin America Study Group «pathology». AO Spine is a clinical division of the AO Foundation, which is an independent medically-guided not-for-profit organization. Study support was provided directly through AO Spine Latin America regarding «support provided»
References
- Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J 9 (2009): 545-550.
- Aleem IS, Drew B. Cochrane in CORR (®): Surgical Versus Non-surgical Treatment for Lumbar Spinal Stenosis. Clin Orthop Relat Res 475 (2017): 2632-2637.
- Kreiner DS, Shaffer WO, Baisden JL, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 13 (2013): 734-743.
- National Guideline C. National Institute for Health and Care Excellence: Guidelines. Low Back Pain and Sciatica in Over 16s: Assessment and Management. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE (2016).
- Shim DM, Kim TG, Koo JS, et al. Is It Radiculopathy or Referred Pain? Buttock Pain in Spinal Stenosis Patients. Clin Orthop Surg 11 (2019): 89-94.
- Manchikanti L, Kaye AD, Soin A, et al. Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines Facet Joint Interventions 2020 Guidelines. Pain Physician 23 (2020): S1-s127.
- Manchikanti L, Knezevic NN, Navani A, et al. Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines. Pain Physician 24 (2021): S27-s208.
- Manchikanti L, Cash KA, McManus CD, et al. A randomized, double-blind controlled trial of lumbar interlaminar epidural injections in central spinal stenosis: 2-year follow-up. Pain Physician 18 (2015):79-92.
- Spijker-Huiges A, Vermeulen K, Winters J, et al. Epidural Steroids for Lumbosacral Radicular Syndrome Compared to Usual Care: Quality of Life and Cost Utility in General Practice. Archives of Physical Medicine and Rehabilitation (2014): 96.
- Spijker-Huiges A, Winters JC, van Wijhe M, et al. Steroid injections added to the usual treatment of lumbar radicular syndrome: a pragmatic randomized controlled trial in general practice. BMC Musculoskeletal Disorders 15 (2014): 341.
- Hwang SY, Lee JW, Lee GY, et al. Lumbar facet joint injection: feasibility as an alternative method in high-risk patients. European Radiology 23 (2013): 3153-3160.
- Shim E, Lee JW, Lee E, et al. Facet joint injection versus epidural steroid injection for lumbar spinal stenosis: intra-individual study. Clin Radiol 72 (2017): e7-.e14.
- Park CJ, Shin YD, Lim SW, et al. The effect of facet joint injection on lumbar spinal stenosis with radiculopathy. Pak J Med Sci 34 (2018): 968-973.
- Ammendolia C, Stuber KJ, Rok E, et al. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst Rev 8 (2013): Cd010712.
- Friedly JL, Comstock BA, Turner JA, et al. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med 371 (2014): 11-21.
- Botwin K, Brown LA, Fishman M, et al. Fluoroscopically guided caudal epidural steroid injections in degenerative lumbar spine stenosis. Pain Physician 10 (2007): 547-558.
- Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil 81 (2002): 898-905.
- Park CH, Lee SH. Correlation between severity of lumbar spinal stenosis and lumbar epidural steroid injection. Pain Med 15 (2014): 556-561.
- Manchikanti L, Knezevic NN, Boswell MV, et al. Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis. Pain Physician 19 (2016): E365-410.
- Meng H, Fei Q, Wang B, et al. Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug Des Devel Ther 9 (2015): 4657-4667.
- Atlas SJ, Keller RB, Wu YA, et al. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976); 30 (2005): 936-943.
- Brown LL. A double-blind, randomized, prospective study of epidural steroid injection vs. the mild® procedure in patients with symptomatic lumbar spinal stenosis. Pain Pract 12 (2012): 333-341.
- Chou R, Hashimoto R, Friedly J, et al. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Ann Intern Med 163 (2015): 373-381.
- Kovacs FM, Urrútia G, Alarcón JD. Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials. Spine (Phila Pa 1976); 36 (2011): E1335-1351.
- Bresnahan BW, Rundell SD, Dagadakis MC, et al. A systematic review to assess comparative effectiveness studies in epidural steroid injections for lumbar spinal stenosis and to estimate reimbursement amounts. Pm r 5 (2013): 705-714.
- Engel AJ, Scott Kreiner D, Stojanovic MP. Finding an Answer: Comments on a Randomized Trial of Epidural Glucocorticoid Injections for Lumbar Spinal Stenosis. Pain Medicine 18 (2016): 204-210.
- Manchikanti L, Falco FJ, Pampati V, et al. Lumbar interlaminar epidural injections are superior to caudal epidural injections in managing lumbar central spinal stenosis. Pain Physician 17 (2014): E691-702.
- Do KH, Kim TH, Chang MC. Effects of interlaminar epidural steroid injection in patients with moderate to severe lumbar central spinal stenosis: a prospective study. Ann Palliat Med 9 (2020): 163-168.
- Olguner SK, Celiktas M, Oktay K, et al. Comparison of 1-year results of single transforaminal epidural steroid injection among patients with different spinal pathologies-related radicular pain. Niger J Clin Pract 23 (2020): 835-841.
- Smith CC, Booker T, Schaufele MK, et al. Interlaminar versus transforaminal epidural steroid injections for the treatment of symptomatic lumbar spinal stenosis. Pain Med 11 (2010): 1511-1515.
- Sencan S, Edipoglu IS, Celenlioglu AE, et al. Comparison of treatment outcomes in lumbar central stenosis patients treated with epidural steroid injections: interlaminar versus bilateral transforaminal approach. Korean J Pain 33 (2020): 226-233.
- Wei G, Liang J, Chen B, et al. Comparison of transforaminal verse interlaminar epidural steroid injection in low back pain with lumbosacral radicular pain: a meta-analysis of the literature. Int Orthop 40 (2016): 2533-2545.
- Sivaganesan A, Chotai S, Parker SL, et al. Predictors of the efficacy of epidural steroid injections for structural lumbar degenerative pathology. Spine J 16 (2016): 928-934.
- Manchikanti L, Kaye AD, Manchikanti K, et al. Efficacy of epidural injections in the treatment of lumbar central spinal stenosis: a systematic review. Anesth Pain Med 5 (2015): e23139.
- Radcliff K, Kepler C, Hilibrand A, et al. Epidural steroid injections are associated with less improvement in patients with lumbar spinal stenosis: a subgroup analysis of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976); 38 (2013): 279-291.
- Rozin L, Rozin R, Koehler SA, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol 24 (2003): 351-355.
- Somayaji HS, Saifuddin A, Casey AT, et al. Spinal cord infarction following therapeutic computed tomography-guided left L2 nerve root injection. Spine (Phila Pa 1976); 30 (2005): E106-108.
- Ziai WC, Ardelt AA, Llinas RH. Brainstem stroke following uncomplicated cervical epidural steroid injection. Arch Neurol 63 (2006): 1643-1646.
- Kennedy DJ, Dreyfuss P, Aprill CN, et al. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med 10 (2009): 1389-1394.
- Lyders EM, Morris PP. A case of spinal cord infarction following lumbar transforaminal epidural steroid injection: MR imaging and angiographic findings. AJNR Am J Neuroradiol 30 (2009): 1691-1693.
- Wybier M, Gaudart S, Petrover D, et al. Paraplegia complicating selective steroid injections of the lumbar spine. Report of five cases and review of the literature. Eur Radiol 20 (2010): 181-189.
- Yoo HS, Park SW, Han JH, et al. Paraplegia caused by an epidural hematoma in a patient with unrecognized chronic idiopathic thrombocytopenic purpura following an epidural steroid injection. Spine (Phila Pa 1976); 34 (2009): E376-379.
- Dietrich TJ, Sutter R, Froehlich JM, et al. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiol 44 (2015): 149-155.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 