Minimally Invasive Approach of Lumbar Plasmacytoma: Case Report
André Guimarães* , Rita Sousa, Sara Neves, Pedro Teixeira Gomes, Luís Castelo
, Rita Sousa, Sara Neves, Pedro Teixeira Gomes, Luís Castelo
Orthopedics and Traumatology Service, Trás os Montes and Alto Douro Hospital Center, Vila Real, Portugal
Corresponding Author: André Guimarães, Orthopedics and Traumatology Service, Trás os Montes and Alto Douro Hospital Center, Portugal.
Received: 22 August 2022; Accepted: 06 September 2022; Published: xx September 2022
Article Information
Citation: André Guimarães, Rita Sousa, Sara Neves, Pedro Teixeira Gomes, Luís Castelo. Minimally Invasive approach of Lumbar plasmacytoma: Case Report. Journal of Surgery and Research 4 (2022): 092-095
View / Download Pdf Share at FacebookAbstract
Solitary Bone Plasmacytoma is a subtype of Solitary Plasmacytoma characterized by a mass of monoclonal plasma cells with involvement of bony structures. This pathology presents a high risk of progression to Multiple Myeloma with systemic involvement. In vertebral involvement it can lead to lytic lesions with progression to vertebral collapse and instability. The clinical case is a female patient with no medical history, with a clinic of low back pain with evolution for more than 1 month, radiography showed wedge of L4 and computed tomography a lytic lesion of that level, was hospitalized for pain control and study. The Magnetic Resonance came to discard the compression of noble parts. She was admitted for surgery due to vertebral instability and minimally invasive L2-L3-L5 posterolateral fixation was performed with transpedicular bars and screws, tissue biopsy and decompression with L4 partial facetectomy laminectomy. Surgery was uneventful and the patient was discharged 3 days after a complementary study of the disease. After 1 month, the patient showed clear improvement in pain and after half a year, the fixation was stable without instability or deformities. The patient was followed up by Orthopedics and Hematology. Plasmacytoma is an uncommon neoplasm and the main symptoms are low back pain, as in the case described. Radiotherapy is the treatment of choice, however surgery has been growing as an adjuvant and clinical improvement. This case demonstrates a unique treatment, not previously described with a percutaneous fixation with good results.
Keywords
Solitary Plasmacytoma; Solitary Bone Plasmacytoma; Vertebra; Minimally Invasive Fixation; Spine Surgery
Solitary Plasmacytoma articles Solitary Plasmacytoma Research articles Solitary Plasmacytoma review articles Solitary Plasmacytoma PubMed articles Solitary Plasmacytoma PubMed Central articles Solitary Plasmacytoma 2023 articles Solitary Plasmacytoma 2024 articles Solitary Plasmacytoma Scopus articles Solitary Plasmacytoma impact factor journals Solitary Plasmacytoma Scopus journals Solitary Plasmacytoma PubMed journals Solitary Plasmacytoma medical journals Solitary Plasmacytoma free journals Solitary Plasmacytoma best journals Solitary Plasmacytoma top journals Solitary Plasmacytoma free medical journals Solitary Plasmacytoma famous journals Solitary Plasmacytoma Google Scholar indexed journals Solitary Bone Plasmacytoma articles Solitary Bone Plasmacytoma Research articles Solitary Bone Plasmacytoma review articles Solitary Bone Plasmacytoma PubMed articles Solitary Bone Plasmacytoma PubMed Central articles Solitary Bone Plasmacytoma 2023 articles Solitary Bone Plasmacytoma 2024 articles Solitary Bone Plasmacytoma Scopus articles Solitary Bone Plasmacytoma impact factor journals Solitary Bone Plasmacytoma Scopus journals Solitary Bone Plasmacytoma PubMed journals Solitary Bone Plasmacytoma medical journals Solitary Bone Plasmacytoma free journals Solitary Bone Plasmacytoma best journals Solitary Bone Plasmacytoma top journals Solitary Bone Plasmacytoma free medical journals Solitary Bone Plasmacytoma famous journals Solitary Bone Plasmacytoma Google Scholar indexed journals Vertebra articles Vertebra Research articles Vertebra review articles Vertebra PubMed articles Vertebra PubMed Central articles Vertebra 2023 articles Vertebra 2024 articles Vertebra Scopus articles Vertebra impact factor journals Vertebra Scopus journals Vertebra PubMed journals Vertebra medical journals Vertebra free journals Vertebra best journals Vertebra top journals Vertebra free medical journals Vertebra famous journals Vertebra Google Scholar indexed journals Minimally Invasive Fixation articles Minimally Invasive Fixation Research articles Minimally Invasive Fixation review articles Minimally Invasive Fixation PubMed articles Minimally Invasive Fixation PubMed Central articles Minimally Invasive Fixation 2023 articles Minimally Invasive Fixation 2024 articles Minimally Invasive Fixation Scopus articles Minimally Invasive Fixation impact factor journals Minimally Invasive Fixation Scopus journals Minimally Invasive Fixation PubMed journals Minimally Invasive Fixation medical journals Minimally Invasive Fixation free journals Minimally Invasive Fixation best journals Minimally Invasive Fixation top journals Minimally Invasive Fixation free medical journals Minimally Invasive Fixation famous journals Minimally Invasive Fixation Google Scholar indexed journals Spine Surgery articles Spine Surgery Research articles Spine Surgery review articles Spine Surgery PubMed articles Spine Surgery PubMed Central articles Spine Surgery 2023 articles Spine Surgery 2024 articles Spine Surgery Scopus articles Spine Surgery impact factor journals Spine Surgery Scopus journals Spine Surgery PubMed journals Spine Surgery medical journals Spine Surgery free journals Spine Surgery best journals Spine Surgery top journals Spine Surgery free medical journals Spine Surgery famous journals Spine Surgery Google Scholar indexed journals L2-L3-L5 articles L2-L3-L5 Research articles L2-L3-L5 review articles L2-L3-L5 PubMed articles L2-L3-L5 PubMed Central articles L2-L3-L5 2023 articles L2-L3-L5 2024 articles L2-L3-L5 Scopus articles L2-L3-L5 impact factor journals L2-L3-L5 Scopus journals L2-L3-L5 PubMed journals L2-L3-L5 medical journals L2-L3-L5 free journals L2-L3-L5 best journals L2-L3-L5 top journals L2-L3-L5 free medical journals L2-L3-L5 famous journals L2-L3-L5 Google Scholar indexed journals posterolateral fixation articles posterolateral fixation Research articles posterolateral fixation review articles posterolateral fixation PubMed articles posterolateral fixation PubMed Central articles posterolateral fixation 2023 articles posterolateral fixation 2024 articles posterolateral fixation Scopus articles posterolateral fixation impact factor journals posterolateral fixation Scopus journals posterolateral fixation PubMed journals posterolateral fixation medical journals posterolateral fixation free journals posterolateral fixation best journals posterolateral fixation top journals posterolateral fixation free medical journals posterolateral fixation famous journals posterolateral fixation Google Scholar indexed journals Traumatology articles Traumatology Research articles Traumatology review articles Traumatology PubMed articles Traumatology PubMed Central articles Traumatology 2023 articles Traumatology 2024 articles Traumatology Scopus articles Traumatology impact factor journals Traumatology Scopus journals Traumatology PubMed journals Traumatology medical journals Traumatology free journals Traumatology best journals Traumatology top journals Traumatology free medical journals Traumatology famous journals Traumatology Google Scholar indexed journals CT Sagittal articles CT Sagittal Research articles CT Sagittal review articles CT Sagittal PubMed articles CT Sagittal PubMed Central articles CT Sagittal 2023 articles CT Sagittal 2024 articles CT Sagittal Scopus articles CT Sagittal impact factor journals CT Sagittal Scopus journals CT Sagittal PubMed journals CT Sagittal medical journals CT Sagittal free journals CT Sagittal best journals CT Sagittal top journals CT Sagittal free medical journals CT Sagittal famous journals CT Sagittal Google Scholar indexed journals facetectomy laminectomy articles facetectomy laminectomy Research articles facetectomy laminectomy review articles facetectomy laminectomy PubMed articles facetectomy laminectomy PubMed Central articles facetectomy laminectomy 2023 articles facetectomy laminectomy 2024 articles facetectomy laminectomy Scopus articles facetectomy laminectomy impact factor journals facetectomy laminectomy Scopus journals facetectomy laminectomy PubMed journals facetectomy laminectomy medical journals facetectomy laminectomy free journals facetectomy laminectomy best journals facetectomy laminectomy top journals facetectomy laminectomy free medical journals facetectomy laminectomy famous journals facetectomy laminectomy Google Scholar indexed journals
Article Details
1. Introduction
Solitary Plasmacytoma (PS) is a single mass of neoplastic clones of plasma cells, representing about 5% of all cellular dyscrasias[1-4] with an incidence of 0.15/100,000 people [2]. It can be subdivided into Solitary Bone Plasmacytoma (PSO) or Solitary Intramedullary Plasmacytoma (PSE), depending on the location it involves, PSO involves only the bone structure and PSE the soft tissues or other organs such as Head, neck and respiratory and gastrointestinal tract [1,2]. 70% of all PS are PSO and comprise all bones with bone marrow respectively: vertebra, femur, pelvis and ribs [2]. Radiotherapy and alternative surgery are treatment modalities, but the results are variable, with a high risk of progression to Multiple Myeloma (MM) 50% PSO and 30% in 10 years [2,4]. PSO can rarely lead to pathological vertebral fractures and consequently to spinal cord instability and compression [5].
2. Case Report
The clinical case is of a 66-year-old female patient, with no relevant personal and family history, who went to the emergency department for non-radiating low back pain with evolution for 1 month. On physical examination, the patient was in good general condition, hemodynamically stable and apyretic, with normal gait but with pain on trunk mobilization, without sciatica, negative provocation tests and normal neurological examination. Lumbar spine radiography (RX) showed L4 wedge (Figures 1,2), but no other changes. Computed Tomography (CT) was performed on the lumbar spine and showed a vertebral canal with normal dimensions and an osteolytic expansive lesion of the L4 body with erosion of the cortical walls, with somatic flattening and bulging of its contours extending to the pedicles of greater area. Left (Figures 3,4). There were no other associated bone lesions, there was also an anterior thickening at this level that could compromise the thecal sac and its roots. Therefore, the patient was hospitalized for pain control and study of the lytic lesion. During hospitalization, an MRI was performed, which showed no apparent endocanal involvement of the lesion and adjacent tissues. Due to her L4 instability, she was admitted for orthopedic surgical treatment.

Figure 1: RX Sagittal.

Figure 2: RX Coronal.
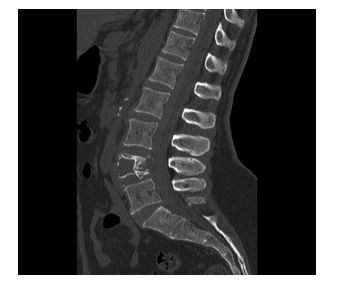
Figure 3: CT Sagittal.
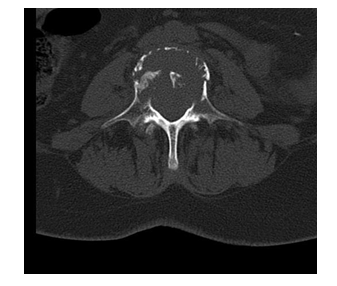
Figure 4: CT Horizontal.
Minimally invasive posterolateral fixation (Orthofix MBA) L2-L3-L5 with transpedicular bars and screws was performed percutaneously, tissue biopsy and decompression with partial facetectomy laminectomy of L4 through a small midline incision (Figures 5,6). The surgery was uneventful, the next day the patient presented with clear improvement in pain and no deficits again. During hospitalization, the patient underwent the analytical study with no evidence of anemia with normal renal function and no other changes and underwent a bone marrow biopsy. After 3 days, the patient was discharged with controlled pain. After 2 weeks, the patient had some discomfort in the area of the surgical scar, but no other changes. Tissue biopsy revealed a cluster of well-differentiated plasma cells with CD138 and CD56 staining and the myelogram showing 6.8% of plasma cells, also in this period a study of Positron Emission Tomography with Fluorie-18-Fluodesoxyglucose (PET - FDG) was carried out. did not mark uptake at other sites of the lesion.
Therefore, the diagnosis of PSO was obtained and 40GY Radiotherapy was started for 4 weeks. After 1 month, the patient had a well-healed surgical scar with improvement in pain, on CT he showed a stable fixation and without deformities again. He maintained follow-up in Hematology every 4 months and Orthopedics every 6 months in the first year (Figure 7,8), and then annually from the 2nd year onwards with interspersed surveillance of X-ray and CAT scans and without a news deficits or failure of percutaneous fixation.
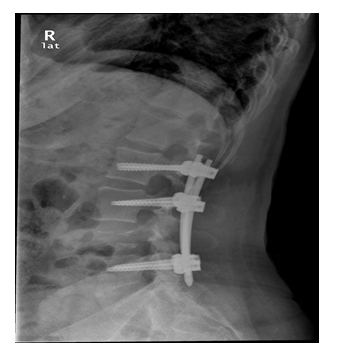
Figure 5: Post-surgery Sagittal
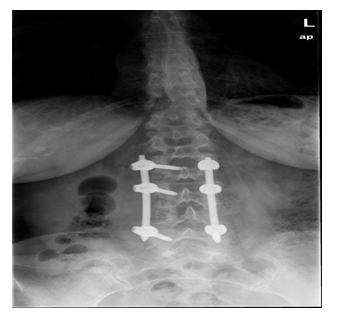
Figure 6: Post-surgery Coronal RX.

Figure 7: Sagittal MRI after 6 months of surgery.
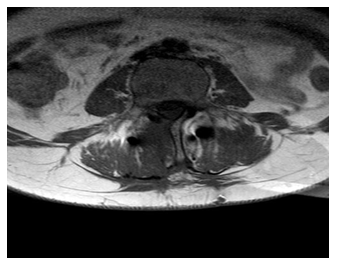
Figure 8 : Horizontal MRI after 6 months of surgery
3. Discussion
The diagnosis of PSO or PSE requires tissue biopsy with monoclonal infiltration of plasma cells. PSO requires the presence of a lytic lesion [1,2]. For the diagnosis of PS there must be no organ damage including hypercalcemia, renal dysfunction and anemia [1,2], which the patient did not have. According to the immunohistochemical characteristics of the plasma cells, the tissue biopsy should reveal characteristics of a homogeneous monoclonal infiltration with the expression of CD138 and/or CD38 [2], being consistent with the diagnosis of the patient with the expression of CD138. To exclude MM, it is necessary that there is no damage to other organs, nor must there be bone marrow infiltration or the presence of up to <10% of monoclonal plasma cells. If there is bone marrow infiltration, there is an increased risk of progression to MM with a mean progression without bone marrow infiltration of 42 months and with monoclonal infiltration of 15 months [1,2]. While monoclonal proteins, Bence Jones, can be detected in the blood up to 72%, however, their persistence for more than one year leads to a risk of progression of 71% to MM, constituting a risk factor and a poor prognosis factor [1,2]. Low back pain is one of the main symptoms of medical consultation and is associated with greater disability in the population. Low back pain can be the first manifestation of malignant pathology attributed to up to 1% [2,5]. Consistent with our case, PS is usually indolent or the first clinical manifestations are low back pain [6], although about 25% develop neurological dysfunction in the form of foraminal or spinal cord compression [4]. These lesions present with a mean age of 55 years and are more frequent in men [1] with an overall incidence of 0.191 for men and 0.090 per 100,000 people for women [2]. Conventionally, radiography and CT have been recommended as the first evaluation imaging tests. In PSO, the trabecular bone is preferably replaced and the cortical bone is preserved or partially sclerosed. However, about two thirds show mixed pattern features predominantly with lithic pattern [2,6]. Although MRI has a lower sensitivity to detect lytic lesions compared to CAT, it is the best exam to detect bone marrow injury and spinal cord compression [1,2], and in this clinical case, confirmation of the absence of spinal cord involvement was crucial. . It is currently the gold standard for imaging. PSO typically involves the vertebrae, half of which cause myelopathy to patients 7]. The vertebral affection is preferential in the body of the vertebra, being more frequent in the thoracic vertebrae [1,2,6,7]. However, vertebral involvement has been reported to have a worse prognosis compared to other sites of skeletal involvement [7]. The pathological fracture similar to this case results from the collapse of the vertebral body and, consequently, the biomechanical instability of the spine and neurological compromise.
Radiotherapy is the treatment of choice [1,2], whereas surgery is not the first line in patients, because in the long term, studies reveal that it does not change the progression of the disease after 10 years, but there is always an indication in the presence of intractable pain, instability and progression of neurological impairment [1,2,8]. Many authors advocate surgery with posterior radiotherapy to minimize local recurrence [5]. Xie L [9] and colleagues in a study of 1275 patients who were treated with radiotherapy alone and radiotherapy plus surgery concluded that progression to MM was much slower in people aged <45 years treated with surgery and radiotherapy. The surgical approach to the patient followed the principles of decompression with laminectomy and stabilization with a more recent percutaneous technique. There are several cases described with radical spondylectomy in bloc surgery or corpectomy with a dual approach [4-6,8], but in cases with involvement of the entire vertebra and with involvement of the extramedullary, dura mater and with severe neurological impairment. Our case did not present spinal cord involvement or involvement of the entire vertebra, so we opted for a minimally invasive fixation, avoiding further sequelae to the patient.
4. Conclusion
This case demonstrates a total benefit in the surgical treatment of PSO with decompression and instrumentation for stabilization, supporting the literature of the great clinical benefit in improving neurological function. Evidencing something that is not demonstrated in the current literature, the possibility of minimally invasive treatment.
References
- Pham A, Mahindra A. Solitary Plasmacytoma: a Review of Diagnosis and Management. Curr Hematol Malig Rep 14 (2019): 63-69.
- Caers J, Paiva B, Zamagni E, et al. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. J Hematol Oncol 11 (2018):
- von der Hoeh NH, Tschoeke SK, Gulow J, et al. Total spondylectomy for solitary bone plasmacytoma of the lumbar spine in a young woman: a case report and review of literature. Eur Spine J 23 (2014): 35-39.
- Yang JS, Cho YJ, Kang SH, et al. Rapid progression of solitary plasmacytoma to multiple myeloma in lumbar J Korean Neurosurg Soc 54 (2013): 426-430.
- Eseonu KC, Middleton SD, Subramanian AS. Paraplegia Secondary to Plasmacytoma of the Lumbar Spine. Int J Spine Surg 14(2020): 559-562.
- Pashayan R, Cavanaugh WM, Warshel CD, et al. Plasmacytoma of the Cervical Spine: A Case Study. J Chiropr Med 16 (2017): 170-174.
- Takahashi, T, Koshu K, Tominaga T, et al. Solitary plasmacytoma in the thoracic spine. Two case reports. Neurosurg Rev 21 (1998): 121-125.
- Mirzashahi B, Mazoochy H, Jamnani RK, et al. Contribution of surgery in solitary plasmacytoma of spine; a case Arch Bone Jt Surg 2 (2014): 121-125.
- Xie L, Wang H, Jiang J. Does Radiotherapy with Surgery Improve Survival and Decrease Progression to Multiple Myeloma in Patients with Solitary Plasmacytoma of Bone of the Spine? World Neurosurg 134 (2020): 790-798.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 