Prematurity of Less than 1000 Grams: Epidemiological, Diagnostic and Prognostic Aspects in a Neonatology Unit at Dakar (Senegal)
Yaay Joor Koddu Biigé DIENG1*, Djénéba Fafa CISSE2, Ndèye Fatou SOW3, Aminata MBAYE1, Awa KANE1, Bienfait MUNDEKE MUJINYA1, Guillaye DIAGNE2, Amadou SOW4, Idrissa Demba BA1, Papa Moctar FAYE1, Ousmane NDIAYE1
1Centre Hospitalier National D’Enfants Albert Royer, SN, Av. Cheikh Anta Diop, Dakar, Senegal
2Centre Hospitalier National de Pikine, Dakar, Senegal
3Hôpital Dalal Jamm, Dakar, Senegal
4Centre Hospitalier Abass Ndao, Avenue Cheikh Anta Diop Dakar fann gueule tapée, Senegal
*Corresponding Author: Yaay Joor Koddu Biigé DIENG, National Children's Hospital Albert Royer, Dakar, Senegal.
Received: 21 January 2024; Accepted: 26 January 2024; Published: 12 February 2024
Article Information
Citation: Yaay Joor Koddu Biigé DIENG, Djénéba Fafa CISSE, Ndèye Fatou SOW, Aminata MBAYE, Awa KANE, Bienfait MUNDEKE MUJINYA, Guillaye DIAGNE, Amadou SOW, Idrissa Demba BA, Papa Moctar FAYE, Ousmane NDIAYE. Prematurity of Less than 1000 Grams: Epidemiological, Diagnostic and Prognostic Aspects in a Neonatology Unit at Dakar (Senegal). Journal of Pediatrics, Perinatology and Child Health 8 (2024): 19-22.
View / Download Pdf Share at FacebookAbstract
Introduction: The aim of this study was to assess morbidity and mortality in premature infants with a birth weight of less than 1000 grams in a referral hospital in Senegal.
Patients and method: We conducted a retrospective, descriptive and analytical study of 142 cases of premature infants weighing less than 1000 grams admitted between January 2014 and December 2020 (7 years) to the neonatology department in Dakar.
Results: The most common maternal age group in our population was under 25 years (56.2%). Primiparous mothers were strongly represented (34.2%). The sex ratio was 1.1. The mean age on admission was 4.7 days, with predominance of 0 days (58.8%). The most common respiratory complications were apnoea (85.6%) and hyaline membrane disease (65.9%), others were jaundice (60.6%), secondary neonatal infections (53.5%), intraventricular haemorrhage (47.5%), persistent patent ductus arteriosus (22.6%). The most common associated pathologies were intrauterine growth retardation (32%) and congenital heart disease (28.8%). Mortality was 55.6% and the bivariate analysis found the following factors: Extreme prematurity (p = 0.004), admission time > 24 hours (p = 0.003), IUGR (p = 0.002), shock (p = 0.000), secondary infection (p = 0.004), respiratory distress (p = 0.003), multiple pregnancies (p = 0.033) and absence of breastfeeding (p = 0.000).
Conclusion: Improving the technical platform, increasing the number of staff and organising perinatal networks remain key areas to be developed in order to improve the survival rate of premature babies weighing less than 1000 grams in our regions.
Keywords
<p>Morbidité; Mortalité; Grande prématurité; Sénégal</p>
Article Details
1. Introduction
In Senegal, and in most countries south of the Sahara, the care of very premature babies and low birth weight babies poses many problems, linked to the technical facilities and the qualifications of the staff. The mortality rate for these very premature babies is therefore high [1]. Most authors in Africa report mortality rates for babies weighing less than 1000 grams of more than 80%, or even close to 100% [2,3]. In addition, estimating their age at birth is difficult due to a number of factors, including pregnancy monitoring and the organisation of care [4].
Survival of premature babies has improved considerably in developed countries, unlike in developing countries [5]. This improvement is the result of various factors, including improved insurance coverage during pregnancy, advanced obstetric and antenatal care and improved systems of risk-adapted care, including resuscitation and stabilisation of high-risk newborns [6-8]. In our department, a great deal of effort has been made in recent years to improve the care of these newborns. These efforts have included building staff capacity and improving the technical platform.
It was in this context that we initiated this study, the main objective of which was to evaluate the morbidity and mortality of premature babies weighing less than 1000 grams in our unit.
2. Patients and Methods
The Centre Hospitalier National d'Enfants Albert Royer (CHNEAR), the setting for this study, is one of the national reference centres for neonatology, with the highest level of neonatal intensive care activity. The centre does not have a maternity unit, so all newborns admitted are transferred or come from home. The neonatology department has a bed capacity of 38, including sixteen intensive care beds (eight incubators and eight resuscitation tables), six intermediate care beds, ten continuous care beds and six kangaroo beds. The medical staff is made up of an associate paediatrician and neonatologist, two paediatricians, one of whom is an assistant university clinical director and a neonatologist, interns and DESs (doctors in specialisation). The paramedical staff includes a state-qualified nursery nurse supervisor, six state-qualified nurses, two midwives, nine nursing assistants and three service agents. The paramedical s serious or unstable patients are rewarmed and monitored clinically for vital parameters, and infusions are carried out using an electric syringe pump. The department has artificitaff is divided into four on-call teams and permanent staff who work 12-hour shifts. There are five service staff. In terms of equipment, allal respirators, a mobile ultrasound machine and a baby feeding station. Premature babies are all referred, with no regulatory limits on gestational term or birth weight. They are cared for in an incubator until they have stabilised haemodynamically, cardio-respiratorily and neurologically, before being transferred to the Kangaroo Unit, where they receive continuous skin-to-skin care with their mother or another family member. This was a historical, descriptive and analytical cohort study conducted from 01 January 2014 to 31 December 2020, a period of 7 years. We included all premature babies weighing less than 1000 grams admitted alive to the department during the study period. Premature babies who died on arrival and those whose records were incomplete or unusable were not included. Data were collected using a standard data collection form. For each newborn included, we collected : sociodemographic aspects (term and age of the newborn on admission, sex, age of the mother, educational and socio-economic level of the family); history (obstetric follow-up and complications, circumstances and place of delivery, route and personnel who attended the delivery) ; data on adaptation to extra-uterine life (time to cry, Apgar score, notion of resuscitation, staff who performed resuscitation and resuscitation manoeuvres); management, evolution and outcome of the newborn during hospitalisation. The data were analysed using Microsoft Excel and expressed as a percentage, mean (with standard deviation) and median. The analytical study was carried out using cross-tabulations in order to determine the Pearson correlation coefficient using the analysis of variance and correlation test with a significance threshold of P ≤ 0.05.
3. Results
During the study period, 142 premature infants weighing less than 1000 grams were admitted to the neonatology department, out of a total of 4553 admissions to the department, including 863 premature infants, representing 3.1% of admissions and 16.4% of premature infants hospitalised. The sex ratio was 1.1 (53% boys). All newborns were referred and almost half (46%) had been admitted after the 24th hour of life. The majority of children (60.1%) came from the suburbs of Dakar.
In terms of mothers and pregnancy, the under-25 age group was the most represented, at 56.2%. Half came from the Dakar suburbs and a quarter from other parts of the country. Primigravida accounted for 34.2%. Ten percent (10%) of the mothers had not had any follow-up during their pregnancy, and less than half (48.3%) had had an early ultrasound scan. Multiple pregnancies concerned 47 children (36%). It should be noted that in many cases of multiple pregnancies, one or more of the twins had died before the transfer. Less than half of the mothers (47.6%) had received antenatal corticosteroids.
Nearly a third of deliveries (30.6%) took place in a health centre and 10.7% were unannounced at home. Caesarean section was used for 27 premature babies (19%) and 34 babies (23.9%) were resuscitated in the delivery room. When specified, gestational age was most often estimated on the basis of clinical maturation scores (40.4%) and the mean was 28SA and 2D. In our population, 121 babies (85.2%) were very premature at less than 33 days' gestation, of whom 37 (26.1%) were very premature at less than 28 days' gestation. Table I summarizes the mode of delivery and the events that occurred.
|
Event |
Number |
Frequency |
|
Maternal fever during labour |
5 |
5,2 % |
|
Premature rupture of membranes |
13 |
13,4 % |
|
Stained amniotic fluid |
38 |
39,1 % |
|
High route |
19 |
19,6 % |
|
No cry at birth |
20 |
20,6 % |
|
Resuscitation (at least until ventilation) |
16 |
16,5 % |
Table 1: Distribution of premature babies according to events at delivery.
On admission, 46% of premature babies had more than 24 hours to live; for 45 newborns (31.6%), prematurity was associated with IUGR and almost ¾ of babies had a birth weight of more than 800 grams. MMH was found in 2/3 of cases (65.9%). Respiratory distress and neonatal infection were the main complications, with 74.2% and 50.5% of cases respectively. The other complications most frequently encountered during the stay were: respiratory: apnoea (85.6%) and MMH (65.9%), infectious: secondary neonatal infections (53.7%), neurological: intraventricular haemorrhage (47.5%), haemodynamic: persistent ductus arteriosus (22.6%) and shock (8.8%) and metabolic: jaundice (60.6%). In addition, exclusive breastfeeding was only possible in less than a third of newborns (31.1%).
|
Complications |
Number |
Frequency |
|
|
Respiratory |
apnea |
85 |
87,6 |
|
respiratoire destress |
72 |
74,2 |
|
|
bronchodysplasia |
3 |
3,1 |
|
|
Hemodynamic |
persistent patent ductus arteriosus |
12 |
12,4 |
|
shock |
5 |
5,2 |
|
|
high blood pressure |
2 |
2,1 |
|
|
Infectious |
neonatal infections |
49 |
50,5 |
|
Digestive |
necrotizing enterocolitis |
6 |
6,2 |
|
Neurological |
intraventricular haemorrhage |
17 |
17,5 |
|
periventricular leukomalacia |
3 |
3,1 |
|
|
Metabolic |
jaundice |
20 |
20,6 |
|
metabolic desorder |
10 |
10,3 |
|
Table 2: Distribution of premature babies according to neonatal complications found.
The fatality rate was 53.6% (76 deaths). Infections (early and late) and HMM were the main causes of death. Death occurred early in the vast majority of cases, with half (51%) within 24 hours and a third (33.4%) within 72 hours, giving an average age of one day at the time of death. Of the 66 newborns who survived, 48.5% (32 newborns) were hospitalized for less than 30 days and continued to receive outpatient kangaroo care.
Bivariate analysis found the following factors to be statistically associated with mortality (P ≤ 0.05): extreme prematurity (P = 0.004), admission time > 24 hours (P = 0.003), IUGR (P = 0.002), shock (P = 0.000), secondary infection (P = 0.004), respiratory distress (P = 0.003), multiple pregnancies (P = 0.033) and absence of breastfeeding (P = 0.000).
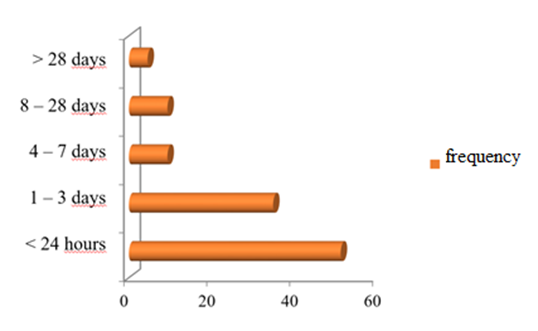
Figure 1: Distribution of premature babies by age at death.
4. Discussion
In our developing countries, most health-related costs are borne by the population, and pregnancy monitoring and the management of many of its complications are no exception. As found in our series, ultrasound dating of pregnancy is not widely available in this context. Only half (51.5%) had had at least one ultrasound scan, and of these only 46% had had an early ultrasound scan in the first trimester [9]. The lack of identification of perinatal networks and the unavailability of obstetric-neonatal liaison forms represent a major difficulty in collecting data relating to the specific history of patients, especially out-borns [10]. The frequency of our cohort is similar to that of Boiro in a neighbouring university hospital with a maternity unit [11] and in Cameroon [4].
The young age of the mothers is a factor commonly found in our regions, most often linked, among other factors, to the lack of socio-economic activity among women [5], although the trend is upwards with the education of girls, who are increasingly taking up professional careers.
The high proportion of premature babies from multiple pregnancies and of births by caesarean section is probably due to the nature of the facility, which is a national reference, and the improved technical facilities for neonatal resuscitation. Despite 90% of births being assisted by qualified staff, only almost half of the cases had received antenatal corticosteroids. This could be linked to premature onset of labour due to the mother's activities, loco-regional infections and, above all, delays in consultation [9]. These delays in consultation also seem to us to have an impact on the administration of complete courses of antenatal corticosteroid therapy. Yet this corticosteroid therapy is one of the essential elements in the fight against premature mortality and should be generalised, especially for these very premature babies weighing less than 1000 grams.
The mean gestational age of 28 days' gestation seems to be linked to: the high proportion of IUGR associated with one third of this series, the frequent multiple pregnancies in this series (36%), the infectious risk factors found (PMR, maternal fever, home birth), all widely reported as contributing to prematurity but also to neonatal mortality [3,9,12].
The negative impact of neonatal transfer on the survival of the newborn is well known [13], especially in the conditions in which we practice in our regions. In our cohort, all newborns were referred, and of these, almost half were referred after the first day of life, most often when complications arose. The main complications found (Table 2) were similar to those already described in premature babies, as were the factors found to correlate with mortality [2,4,7,11].
We noted a mortality rate of 53.6% in our study population. This result, although high, remains lower than those reported in developing countries and in the Dakar region [2,11]. The majority of deaths occurred within the first 24 hours of hospitalisation, mainly in the extreme immature and late transfers [14-16].
5. Conclusion
Improving the technical platform, increasing the number of staff, in-utero transfer and organising perinatal networks remain key areas to be developed in order to improve the survival rate of premature babies weighing less than 1000 grams in our regions.
Study limitations: Historical cohort, small sample size, single-centre study.
References
- Barfield WD. Public Health Implications of Very Preterm Birth. Clin Perinatol 45 (2018): 565-577.
- Balaka B, Baeta S, Agbèrè AD, et al. Assimadi, Prématuré facteurs de risque associes a la prématurité au CHU de LOME TOGO (2002).
- Kalume M, Kizonde K. Mortalité néonatale précoce du prématuré à Lubumbashi- Facteurs de risque. Médecine d'Afrique Noire n°5306 (2006): 343-348.
- Nlend AEN, Zeudja C, Motaze AN, et al. Immediate neonatal outcome of extreme prematurity: retrospective data of a neonatal unit in Yaounde, Cameroon from 2009 to 2013. Pan Afr Med J 20 (2015): 321.
- Schoen CN, Tabbah S, Iams JD, et al. Why the United States preterm birth rate is declining. Am J Obstet Gynecol 213 (2015): 175-180.
- Stoll BJ, Hansen NI, Bell EF, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314 (2015): 1039-1051.
- Lasswell SM, Barfield WD, Rochat RW, et al. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA 304 (2010): 992-1000.
- Engle WA, American Academy of Pediatrics Committee on Fetus and Newborn. Surfactant replacement therapy for respiratory distress in the preterm and term neonate. Pediatrics 121 (2008): 419.
- Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health 10 (2013): S2.
- Ancel PY, Goffinet F, EPIPAGE 2Writing Group, et al. Survival and morbidity of preterm children born at 22 through 34weeks’ gestationin France in 2011.
- Boiro D, Seck N, Thiam L, et al. Les nouveau-nés prématurés de moins de 1000 grammes : morbidité et mortalité en milieu hospitalier à Dakar (Sénégal). PAMJ Clinical Medicine 7 (2021).
- Barkat A, Mdaghri Alaoui A, Hamdani Naima Lamdouar S. Problématique de la prise en charge de la prématurité au Maroc : Expérience du Service de Néonatologie Centre National de Référence en Néonatologie Hôpital d'enfants – Rabat. Santé tropicale.
- Faye PM, Dieng YJ, Diagne-Guèye NR, et al. Problématique des transferts néonatals dans la région de Dakar (Sénégal). Revue de Médecine Périnatale 8 (2016): 94 à 102.
- Messer J. Prematurity and hypotrophy at birth. Epidemiology, causes and prevention. Rev Prat 44 (1994): 679-682.
- Mohammad K, AbuDalou A, Kassab M, et al. Prevalence and factors associated with the occurrence of preterm birth in Irbid governorate of Jordan: a retrospective Study. Int J Nurs Pract 11 (2014).
- Bezzine A, Chebbi I, Ben Hamida E, et al. In-hospital mortality of very preterm infants in a Tunisian neonatal intensive care unit: Prevalence and risk factors. Tunis Med 96 (2018): 884-887.


 Impact Factor: * 4.8
Impact Factor: * 4.8 Acceptance Rate: 69.70%
Acceptance Rate: 69.70%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 