Rehabilitation Protocol for spondylolisthesis Patients: A Treatment Protocol
Majidur Rahman1, Zahid Hasan2, Aminul Islam3, Shahid Afridi4*, Mayesa Nujhat5
1 MscPT, Senior Physiotherapy Officer, Enam Medical College & Hospital
2 Clinical Physiotherapist, Centre for The Rehabilitation of The Paralyzed
3 MscPT, Head of the physiotherapy department, Super Hospital, Dhaka.
4 Intern Physiotherapist, Centre for The Rehabilitation of The Paralyzed
5 MPH, Senior Physiotherapy Officer, Enam Medical College & Hospital
*Corresponding Author: Zahid Hasan, Clinical Physiotherapist, Centre for The Rehabilitation of The Paralyzed, Dhaka.
Received: 14 May 2023; Accepted: 31 May 2023; Published: 02 June 2023
Article Information
Citation: Md Majidur Rahman, Md Zahid Hasan, Aminul Islam, Shahid Afridi, Mayesa Nujhat. Rehabilitation Protocol for spondylolisthesis Patients: A Treatment Protocol. Journal of Spine Research and Surgery. 5 (2023): 35-39
View / Download Pdf Share at FacebookAbstract
Background:
Spondylolisthesis refers to the anterior slippage of one vertebra upon another. Objectives: To assist physiotherapists in decision-making during intervention for patients with spondylolisthesis grades I and II.
Methodology:
Evidence-based physiotherapy treatment protocol for spondylolisthesis. RCT study was used to develop this evidence.
Results:
This study was found evidence-based physiotherapy treatment on spondylolisthesis. There are very few RCT studies is found during searching. This study found that lumbar flexion exercise, as well as stretching of hip flexors, hamstring, piriformis, thoracic mobilization, and others, is effective for the spondylolisthesis.
Conclusion:
More and better research is necessary to establish evidencebased treatment protocol for lumbar spondylolisthesis in the future.
Keywords
<p>Spondylolisthesis; evidence-based treatment; physiotherapy</p>
Article Details
Background
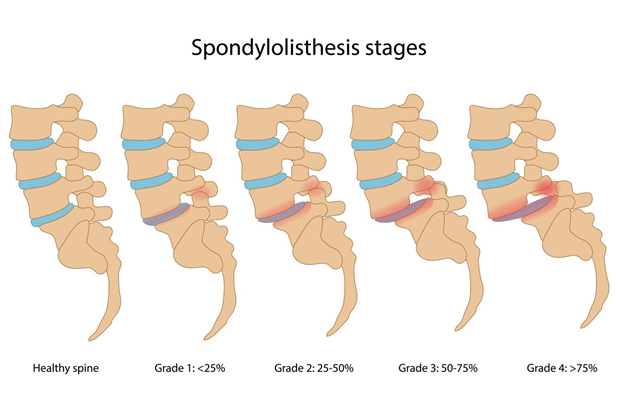
A condition within which a bone slips forward against the caudal one with or while not the separation of posterior parts is termed dislocation. just about some roughly more or less around or so about 2 to 6 % of the overall population is plagued by this disorder[1]. As per the Wiltse-Newman arrangement, there square measure 5 styles of dislocation, that square measure follows-dysplastic, isthmic, chronic, awful, and neurotic. abnormality is the inborn deformity somewhere within the vary of L5 and S1. Isthmic sort characterizes dislocation that outcomes from imperfections of the standards interarticularis. chronic dislocation is attributable to long-standing intersegment insecurity and is viewed as a standard case of spinal shakiness occurring attributable to dynamic degeneration of the feature joints and also the bone plates with maturing[2]. Another framework is used, within which the extent of slippage is decided. during this manner, it okay could also be considered: grade I - twenty-fifth or less, grade II - somewhere within the vary of twenty-fifth and, grade III - somewhere within the vary and seventy-fifth, and grade IV - a lot of noteworthy than seventy-fifth[3].
Aim of study:
To find out evidence-based physiotherapy treatment protocol for a physiotherapist on the lumbar spondylolisthesis.
Literature Review
Spondylolisthesis alludes to the foremost movement or slippage of one vertebra according to the nearby lower vertebrae. It most usually happens between L5 and S1 vertebrae and followed by a slip between L4 and L5 is normal [4]. Spondylolisthesis happens in roughly 6% of the populace. Commonness appraisals of spondylolisthesis among females go from 6% in Taiwan to 20-25% in the United States, while those among guys extend from 3% in Taiwan and 4-8% in the United States. In Japan there is one investigation discovered, they revealed that the predominance of spondylolisthesis at any level was 15.8% in the all-out example, 13.0% in guys, and 17.1% in females[5].
Another research suggests that anywhere from 6-31% of the United States population suffers from degenerative spondylolisthesis. The most common level for degenerative anterolisthesis is L4-L5. Females are 5 times more likely to suffer from anterolisthesis than males[6]. Another study was found on specific stabilization exercise where the researcher hypothesis that specific exercise training of the "stability" muscles of the trunk is effective in reducing pain and functional disability in patients with spondylolisthesis. Forty-four patients with radiologically diagnosed spondylolisthesis were randomly assigned in two groups named specific exercise group and control group. The specific exercise group underwent a 10-week treatment program directed on a weekly basis by one of four manipulative physiotherapists. The intervention program was to train the specific contraction of the deep abdominal muscles, without substitution from large torque-producing muscles such as rectus abdominis and external oblique, using the abdominal drawing-in maneuver, and train the specific contraction of deep abdominal muscles with co-activation of LM proximal to the pars defect. The holding time for these exercises was increased gradually so that patients were able to perform 10 contractions with 10-second holds. Patients also performed this exercise at home. When a patient can perform accurate activation of co-contraction patterns without synergic involvement, encourage the subject to activate these muscles regularly during daily activities, especially in a situation where previously aggravate their symptom. On the other hand, the control group went treatment throughout a 10-week period with general exercises such as swimming, walking, gym work as well as pain-relieving methods such as heat, massage, and ultrasound therapy. After the intervention, they found that the specific exercise group showed a statistically significant reduction in pain intensity and functional disability levels with a 30-month follow-up. On the other hand, CG did not show a significant change[1].

Figure: spondylolisthesis
Description
Lumbar spondylolisthesis causes Segmental instability that results from hypomobility or hypermobility of the spine segment above or below restricted segments. Researchers tried to explore the effects of mobilization of the hypermobile upper thoracic spine along with conventional flexion exercises and stretching of short hip flexors on the degree of slippage and the functions of the persons with lumbar spondylolisthesis. Around 200 patients with spondylolisthesis were randomly assigned into two groups where experimental group treated with mobilization of the thoracic spine along with the conventional physiotherapy and conventional group treated with conventional stretching, strengthening, and lumbar flexion exercise program. The overall results of the study showed that both the groups improved in function as registered by the Modified Oswestry Disability Questionnaire from pre-treatment to post-treatment and the improvement of pain score, flexibility, and strength. The experimental group was treated with passive stretching of bilateral hip flexors, hamstrings, piriformis, passive William’s flexion exercise, myofascial release, posterior pelvic tilt exercise, central PA mobilization of the thoracic spine. The conventional group was advised to do auto hip flexors, hamstrings and piriformis stretching, Williams spinal flexion, and posterior pelvic tilting exercise as a home exercise program. Both groups were given moist heat. Both groups were also instructed to avoid movement and activity that causes spinal extension and use a lumbosacral brace during traveling and exertion. In addition, postural awareness was instructed to maintain normal posture. The experimental group showed a significant reduction in the percentage of vertebral slip from pre-treatment to post-treatment measurement. So, spondylolisthesis patients may be benefited by mobilization of the thoracic spine along with stretching of short hip flexors, piriformis, lumbar flexion range of motion exercises, core strengthening exercises[7].
A study was found wherever researchers have tried to see the results of stabilization exercises on pain and performance in patients with chronic dislocation. it absolutely was a non-randomized test, with six months of follow-up wherever twenty patients over fifty years older with chronic dislocation underwent a 6-month, home-based educational program of stabilization exercises. the house exercise programs comprising of the initial section, with the utilization of therapeutic heat via a hot pack for quarter-hour at the lumbosacral region, stretching exercises of the thoracolumbar facia, hip flexors, hamstrings, triceps, and initial stabilization exercises to encourage helpful motor patterns and confirm the neutral position of the spine, with the target up to the mark of transverses and internal oblique abdominals, multifidus, girdle floor muscles, and diaphragmatic respiratory management. Progression stages enclosed hot packs, stretching exercises, and stabilization exercises with lateral and anterior bridges, leg raises within the supine position, and arm and leg carry in an exceeding quadruped position (“bird-dog”) employing a resistance-progressive program from no weight to zero.5 kilograms and one kilogram within the extremities. Patients were regular for a monthly hour-long session with the healer for elucidative everything. Pain scales (Visual Analogue Scale [VAS] and Oswestry incapacity Index [ODI]) were used as a mensuration tool. each pain and Oswestry Index scores were considerably slashed. Initial and final visual analog scale for “back pain” and “sciatic pain” results slashed. body part stabilization exercises can be a good treatment possibility in dominant pain and up operate in patients with chronic dislocation[8].
A very previous study was found that forty-eight non-operative patients with non-traumatic back pain with lumbar spondylolisthesis are included and maintained for three years follow-up. Participants are randomly assigned to two groups named flexion and extension groups. Prescribed exercise techniques were flexion or extension. Flexion exercises were flexion of the lumbar spine. These exercises consist of abdominal strengthening (isometric or isotonic), pelvic tilt, and chest-to-thigh position. Extension exercises resulted in lumbar extension beyond the neutral position. These exercises consist of upper back extension in prone lying and hip extension prone lying. The instructions had given to both groups about posture (dynamic and static), lifting techniques, and the use of heat for the relief of symptoms. This study stated that flexion exercises are more beneficial than extension exercises for symptomatic relief and also recommended heat to relieve symptoms, posture and lifting instructions to decrease faulty body mechanics and to decrease lumbar lordosis, flexion exercises to stretch rectus spinal muscles, and exercises to strengthen the abdominal muscles and lower back musculature[9].
The patient received lower body part traction victimization the whole target force counter stress traction unit. The patient was positioned supine on a customary medical care table whereas the target force elevated the pelvis with a posterior-to-anterior (PA) force applied at S1-S2 with Associate in Nursing AP force applied at L4-L3 so as to correct the dislocation. the aim is to produce long-duration deformation forces to the soft tissues that have habituated to a patient’s abnormal posture. the standard patient starts with traction to their tolerance two for two to four minutes and will increase by two minutes with every visit till fifteen to twenty minutes is achieved. during this case, the patient started with four minutes of traction and bit by bit progressed every visit to achieve the specified fifteen-minute traction session [8].
|
Impairment / Problem |
Physiotherapy treatment |
|
Pain |
Lumbar flexion exercise |
|
Moist heat |
|
|
Hot pack and TENS |
|
|
Faulty body posture |
Educate the patient |
|
Postural awareness |
|
|
Instruction lifting technique |
|
|
Use a lumbosacral brace during traveling and exertion |
|
|
Reduce ROM |
Lumbar flexion exercise |
|
Passive stretching |
|
|
The tight hip flexor, hamstring, piriformis, and thoracolumbar fascia. |
Passive stretching |
|
Pelvic floor and abdominal muscles weakness |
Strengthening exercise |
|
Abdominal and lower back muscles |
Strengthening exercise (Isometric or isotonic). |
|
Hypermobile of the thoracic spine |
Maitland's rhythmical oscillatory central PA |
|
Lumbar instability |
Lumbar stabilization exercise: twice a day, every day, 10 repetitions of each exercise |
|
Specific stabilization exercise |
|
|
Abnormal spinal alignment |
Lumber traction |
|
Supine and Prone lumbar traction |
|
|
Posterior pelvic tilt |
Posterior pelvic tilting exercise |
|
Paraspinal muscle spasm |
Myofascial release |
Table 1: Evidence-based physiotherapy treatment protocol for spondylolisthesis.
Discussion
This evidence-based physiotherapy treatment protocol is developed for physio professionals. Additionally, this protocol addresses the need to decrease inconsistency and increase transparency in clinical practice and legitimize the profession in eyes of external stakeholders. It increases the transparency of evidence to justify intervention. As far, I know there is still no developed physiotherapy treatment protocol on spondylolisthesis. It will assist the Physiotherapist with developing a path for future clinical research. Allow professionals to self-assess their current practice. Provide quick access to the synthesis of evidence. This protocol will help in clinical practice to make conclusions for the patient with radiologically diagnosed spondylolisthesis grades I and II. This protocol was made on the randomized clinical trial about spondylolisthesis. In our clinical practice, we can drive to the lumbar flexion exercise. Lumbar stabilization exercise and thoracic mobilization were also found effective with lumbar flexion exercise. This study did not cover the congenital spondylolisthesis and mainly focused on acquired spondylolisthesis due to degenerative and traumatic. We can advise the patient to wear to lumbosacral brace during traveling. It was a very challenging task for me because I have no experience with such a developing protocol. There are very few RCT-type studies originated during searching literature on the physiotherapy management of spondylolisthesis which is divided into grades I & II. Most of the RCT design type study was the postoperative physiotherapy management of spondylolisthesis regarding grade III & IV.
CONCLUSION
This physical therapy treatment protocol was developed for patients with dislocation United Nations agency is tormented by grades I & II. Low back pain because of dislocation we will begin the direction of flexion exercise of the lower body part spine. Lower body part stabilization exercise additionally should be practiced in our daily clinical exercise to supply body part stability. additionally, pectoral mobilization, stretching of hip flexors and piriformis, myofascial unleash for paraspinal muscle spasms were additionally steered. Teach the patient regarding bodily property alertness and also the correct lifting system. The patient is additionally trained to wear a lumbosacral brace solely throughout traveling and also the remainder of the time don’t wear the brace.
Author contributions
Md Majidur Rahman: Critical intellectual input, read and approval of the final submission, study concept and design, methodology, revision for critically intellectual content.
Shahid Afridi: Critical intellectual input, read and approval of the final submission, study concept and design, methodology, writing manuscript draft, study supervision.
Aminul Islam: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Md Zahid Hasan: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Mayesa Nujhat : Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest:
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Iguchi T, Tomoaki W, Akira K, et al. Lumbar multilevel degenerative spondylolisthesis: radiological evaluation and factors related to anterolisthesis and retrolisthesis. J Spinal Disord Tech 15 (2002): 93-99.
- Ferrero E, Simon AL, Magrino B, et al. Double-level degenerative spondylolisthesis: what is different in the sagittal plane? Eur Spine J 25 (2016): 2546-2552.
- Koslosky E, Gendelberg D. Classification in Brief: The Meyerding Classification System of Spondylolisthesis. Clin Orthop Relat Res [Internet] 478 (2022): 1125.
- Zhang GZ, Deng YJ, He XG, et al. Different Types of Double-Level Degenerative Lumber Spondylolisthesis: What Is Different in the Sagittal Plane? World Neurosurg 150 (2021): e127-134.
- Ferrero E, Ould-Slimane M, Gille O, Guigui P, French Spine Society (SFCR). Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J 24 (2015): 1219-1227.
- Mehta VA, Amin A, Omeis I, et al. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 76 (2015): S42-56.
- Huang KY, Lin RM, Lee YL, et al. Factors affecting disability and physical function in degenerative lumbar spondylolisthesis of L4-5: Evaluation with axially loaded MRI. Eur Spine J 18 (2009): 1851-1857.
- Clare H A, Adams R, Maher C G. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother 50 (2004): 209-216.
- Thoomes E J. Effectiveness of manual therapy for cervical radiculopathy, a review. Chiropr Man Ther [Internet] 24 (2022): 1-11.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 