Team-Based Learning in Emergency Medicine: A Cross-Sectional Analysis of Medical Student Satisfaction
Rabeb Mbarek1*, Haifa Bradai1, Nabil Chebbi1, Lotfi Boukadida1, Chebili Naoufel1
1Faculty of medicine of Sousse; University of Sousse, Tunisia.
*Corresponding author: Rabeb Mbarek, Faculty of medicine of Sousse; University of Sousse, Tunisia.
Received: 12 May 2025; Accepted: 16 May 2025; Published: 16 October 2025
Article Information
Citation: Rabeb Mbarek, Haifa Bradai, Nabil Chebbi, Lotfi Boukadida, Chebili Naoufel. Team- Based Learning in Emergency Medicine: A Cross- Sectional Analysis of Medical Student Satisfaction. Archives of Internal Medicine Research. 8 (2025): 324-330.
View / Download Pdf Share at FacebookAbstract
Background:
Team learning is relatively new to medical education. It was integrated into the preclinical programme of a medical school in 2002, and intoour faculty of medicine of Sousse, Tunisia, in 2017. The aim of this study was to assess the satisfactions of teamwork with this method of "team-based learning" by medical students in the fourth medical year for the topic of disaster management in emergency medicine.
Method:
This was a cross-sectional analytic study describing the first implementation of critical medicine team-based learning among fourth undergraduate medical students in the faculty of medicine of Sousse, Tunisia, during the 2022-2023 university year after institutional educational development committee approval. An anonymous selfadministered questionnaire on their attitudes and satisfactions of team learning was drawn upfor all the fourth-year medical students. Data were analysed using SPSS 20.0.
Results:
Significant attitudinal satisfaction was found in the areas of professional development, satisfaction with the team experience, satisfaction with peer review, the impact of the team on the quality of learning and the impact of the team on clinical reasoning skills.
Conclusion:
This study demonstrates the students' positive attitude towards teamwork, their sense of professional development, and their comfort and satisfaction with peer assessment.
Keywords
<p>Satisfaction- Medical student- Team-Based Learning</p>
Article Details
Introduction
Over the last decade, educators on university campuses have increasingly used a teaching method known as team-based learning (TBL) [1]. The TBL integrates several small groups into one large group [2]. Part of the appeal of TBL for vocational schools is the combination of efficient use of resources (one teacher to manage several groups simultaneously) and the promise of active student participation, which is generally only possible with other small group work methods [3].
Medical education is undergoing a major revolution. With the increasingly accepted idea that adults learn by [4] actively engaging and modifying what they learn in the context of that engagement [2]. Certainly, there are difficulties in applying this method because of the intensity of the resources required to teach in small groups. However, in the last decade, medical educators have begun to use a cost-effective teaching method called team-based learning (TBL). This method, originally used in business schools, allows a single teacher to bring small groups into the teaching room and simultaneously conduct activities with all learners in the room.
In the literature, the impact of this method of teaching and the satisfaction of medical students in various fields were studied [5], but for critical medicine, we did not find studies that speak about it from where the idea of our study followed a first experiment of TBL within the certificate of medical studies of 2nd cycles in medicine "critical medicine" on the course “Disaster management in emergency medicine" in the faculty of medicine of Sousse, As far as we know, our study is unique.
Our objectives in this study were to measure the satisfaction of teamwork with the method "team-based learning" by fourth-year undergraduate medical students for the topic “Disaster management in emergency medicine".
Material and Methods
This was a cross-sectional analytic study describing the first implementation of critical medicine team-based learning among fourth undergraduate medical students in the faculty of medicine of Sousse, Tunisia, during the university year 2022-2023 after institutional educational development committee approval and the faculty of medicine ethics committee approval.
The questionnaire was anonymous and was filled electronically by all fourth-year medical students (exhaustive list of all students) at the end of the TBL course, regarding their attitudes and perceptions about team-based learning.
Inclusion criteria: Students agreeing to participate in this study.
Exclusion criteria: Incomplete survey data.
Composition of the teams
Before the module, 180 fourth-year undergraduate medical students from the Faculty of Medicine in Sousse were divided into two groups of 90. The students in each group were then divided into 9 teams. Each team consisted of nine to 10 students. To avoid organizing the learners into predefined subgroups (for example, a single-sex team) according to their choices, the teachers formed the teams randomly by giving them rules. The teams were given a fixed space in the classroom for the duration of the module. All the procedures for this session were approved in advance by the teaching team in the development centre at the Faculty of Medicine in Sousse and by the coordinators of the "critical medicine" certificate.
Background
The Faculty of Medicine of Sousse has been committed to the quality of medical education since its creation in 1974. Its openness to other French and Canadian faculties of medicine has made it a pioneer in the field of teaching and an innovator, with talk of self-training and student-centered teaching.
In 2006, as part of the Quality Support Program (Programme d'Appui à la Qualité - PAQ), a team of teachers from the Faculty of Medicine involved in teaching submitted a project aimed at strengthening teaching skills, entitled "Pedagogical Development and Learning Management". It was as part of this project that the Pedagogical Development Centre (CDP) was created and became operational in 2009.
This long-term preparatory work facilitated the implementation of the reform, which came into being in 2016. This change of direction subsequently necessitated a vast teacher training operation specific to the different tasks carried out by the teachers involved in this program.
Many active learning methods were used, and to facilitate their implementation, pedagogical training for the faculty's academics in the form of pedagogical seminars, in-service training and an enriched program for a certificate of complementary study in medical pedagogy were developed within the faculty, as well as clear and practical guides on the faculty's website under the heading of pedagogical development center, to help them put these innovative methods into practice, from which we took the basis of our team-based learning session.
Design of TBL sessions according to FMS guidelines
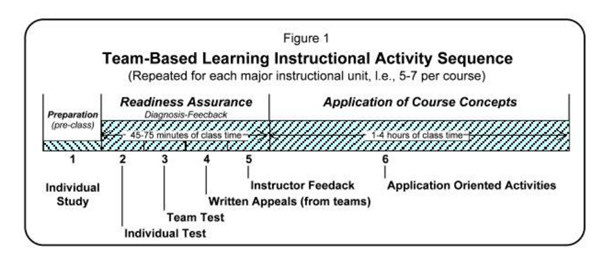
TBL session schedule (6)
15 min: Welcome of student and team organization
15 min: Activity 1: individual test (i-RAT)
15 min: Activity 2: Team test (t-RAT)
30 min: Activity 3: Calls 30 min
30 min: Activity 4: Feedback
15 min: Break
45 min: Activity 5: Application and discussion within and between teams
The course and its objectives are prepared and made available to students on the faculty's virtual platform (ent.uvt.rnu.tn).
Access is based on a code issued to each student at the time of administrative registration.
Location: library room Duration: 03.30 hours (from 12.30 to 15.00 for the 1st group then from 15.30 to 19.00 for the second group)
Teachers: 3 teachers for one TBL session
Target population: fourth-year undergraduate students from the Faculty of Medicine of Sousse. The students are divided by the administration into 8 groups named in alphabetical order from A to H.
For theTBL session, 4 groups were assembled for 2 TBL sessions (one session for groups A, B, C and D and a 2nd session for groups E, F, G and H).
During the TBL session, the students are divided into teams of 8 to 9 students.
The TBL session itself:
According to the founder of this new learning method, the TBL takes place in 3 phases and 6 stages, as explained in the following diagram (Figure 1):
Student satisfactions
The questions in our survey were developed over a period of 5 years as part of the organizational courses in the Department of Communication at Wright State University [8]. These particular questions have been identified in numerous studies of participant satisfaction with previous group experiences [9].
The questionnaire used in this study included 19 statements with Likert-type responses ranging from "Strongly disagree" (1) to "Strongly agree" (4). The consent of students was necessary to complete the questionnaire. The declarations were divided into 5 subgroups: overall satisfaction with the team experience/impact of the team on quality of learning/satisfaction with peer review/impact of the team on clinical reasoning skills and professional development (Figure 2).
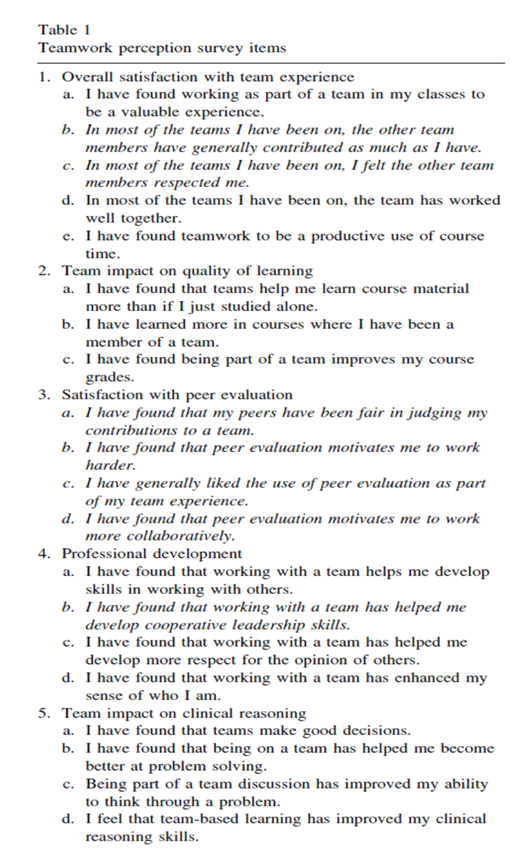
Figure 2: Teamwork perception survey items
The questionnaire for this study was inspired by the Minnesota Satisfaction Questionnaire [7]. Many of the specific questions in our survey can be found in a variety of studies on participants' perceptions of satisfaction with group experiences (Parmele et al. questionnaire).
The assessment instrument used was changed from a 5-point scale to a 4-point scale. The questionnaire was converted into French and distributed online using google forms; the confidentiality of participants was respected.
Informed consent obtained from all participants.
However, no other changes were conducted before obtaining our students' responses.
Data Analyses
Statistical analyses were carried out using SPSS software (statistical package for social science) version 20.0.
Qualitative variables were described by absolute and relative numbers and percentages. Quantitative variables were represented by the median and quartiles after checking the normality of their distribution using the KOLMOGOROV SMIRNOV TEST.
To compare the results, we performed univariate analyses using Pearson's chi2 test and Fischer's test.
We defined the statistical significance threshold at 5% for the different tests used.
Results
Characteristics of the participants
A total of 180 students participated. After excluding students with missing data, complete data were available for 126 students. The effective response rate was 70% (126 out of 180 eligible students). In total, 79.4% (n=100) of the applicants were women. The sex ratio (M/F) was 0.26.
Their median age was 22 years (IQR: [22- 23]). A female predominance was noted (100 (79.4%) women and 26 (20.6%) men).
Four nationalities were present in our study group, the first being Tunisian (118 students; 93.7%), followed by Algerian (4 students; 3.2%), Moroccan and Palestinian (2 students each; 1.6%).
Almost all of the groups (98.4%) had previous experience with this learning method.
The demographic profile of the candidates who took part in the survey is shown in Table I.
Table I: Demographic Characteristics
|
Demographic |
% (n=126) |
Median [IQR] |
|
Age |
- |
22 ans [22-23] |
|
Gender Male |
20.6% (26) |
- |
|
Female |
79.4% (100) |
|
|
|
|
- |
|
Previous experience with TBL |
98.4%(124) |
|
|
Nationality |
|
- |
|
Tunisian |
93.7 (118) |
- |
|
Algerian |
3.2 (4) |
- |
|
Moroccan |
1.6 (2) |
- |
|
Palistinian |
1.6 (2) |
Results of the satisfaction scale
In our population, the satisfaction rate was high, with an “overall satisfaction with team experience” rate of 100 (79.4%).
Analysis of each domain showed greater satisfaction for Team impact on clinical reasoning ability (88.9%), followed by Professional development (82.5%). The results are shown in Table II.
Table II: Student satisfaction in the five domains of the satisfaction survey (n=126).
|
Question |
Insatisfaction |
Satisfaction |
||
|
Overall Satisfaction with Team Experience |
26 (20.6) |
100 (79.4) |
||
|
I have found working as part of a team in my classes to be a valuable experience |
18 (14.3) |
108 (85.7) |
||
|
In most of the teams I have been on, the other team members have generally contributed as much as I have |
54 (42.9) |
72 (57.1) |
||
|
In most of the teams I have been on, the team has worked well together |
0 (0) |
126 (100) |
||
|
In most of the teams I have been on, I felt the other team members respected me |
30 (23.8) |
96 (76.2) |
||
|
I have found teamwork to be a productive use of course time. |
62 (49.2) |
64 (50.8) |
||
|
Team Impact on Quality of Learning |
42 (33.3) |
84 (66.7) |
||
|
I have found that teams help me learn course material more than if I just studied alone |
52 (41.3) |
74 (58.7) |
||
|
I have learned more in courses where I have been a member of a team |
38 (30.2) |
88 (69.8) |
||
|
I have found being part of a team improves my course grade |
28 (22.2) |
98 (77.8) |
||
|
Satisfaction with Peer Evaluation |
38 (30.2) |
88 (69.8) |
||
|
I have found that my peers have been fair in judging my contributions to a team |
18 (14.3) |
108 (85.7) |
||
|
I have found that peer evaluation motivates me to work harder |
48 (38.1) |
78 (61.9) |
||
|
I have generally liked the use of peer evaluation as part of my team experience |
36 (28.6) |
90 (71.4) |
||
|
I have found that peer evaluation motivates me to work more collaboratively |
34 (27) |
92 (73) |
||
|
Team Impact on Clinical Reasoning Ability |
14 (11.1) |
112 (88.9) |
||
|
I have found that being on a team has helped me become better at problem solving |
12 (9.5) |
114 (90.5) |
||
|
I have found that teams make good decisions |
18 (14.3) |
108 (85.7) |
||
|
Being part of a team discussion has improved my ability to think through a problem |
24 (19) |
102 (81) |
||
|
Professional Development |
22 (17.5) |
104 (82.5) |
||
|
I have found that working with a team helps me develop skills in working with others |
20 (15.9) |
106 (84.1) |
||
|
I have found that working with a team has helped me develop cooperative leadership skills |
22 (17.5) |
104 (82.5) |
||
|
I have found that working with a team has helped me develop more respect for the opinions of others |
16 (12.7) |
110 (87.3) |
||
|
I have found that working with a team has enhanced my sense of who I am |
26 (20.6) |
100 (79.4) |
Correlation between gender and satisfaction:
Analysis of the satisfaction rate for each domain by gender showed greater satisfaction among females for Overall Satisfaction with Team Experience, Team Impact on Clinical Reasoning Ability and Professional Development, with p values calculated at 0.012, <0.001 and 0.003, respectively. There was no significantdifference for the other domains (Table III).
Table III: Satisfaction difference between males and females (n=126).
|
|
Insatisfaction |
Satisfaction |
p |
||
|
Overall Satisfaction with Team Experience |
|||||
|
Male |
10 (38.5) |
16 (61.5) |
0.012 |
||
|
Female |
16 (16) |
84 (84) |
|||
|
Team Impact on Quality of Learning |
|||||
|
Male |
12 (46.2) |
14 (53.8) |
0.12 |
||
|
Female |
30 (30) |
70 (70) |
|||
|
Satisfaction with Peer Evaluation |
|||||
|
Male |
8 (30.8) |
18 (69.2) |
0.939 |
||
|
Female |
30 (30) |
70 (70) |
|||
|
Team Impact on Clinical Reasoning Ability |
|||||
|
Male |
10 (38.5) |
16 (61.5) |
<0.001 |
||
|
Female |
4 (4) |
96 (96) |
|||
|
Professional Developement |
|||||
|
Male |
10 (38.5) |
16 (61.5) |
0.003 |
||
|
Female |
12 (12) |
88 (88) |
|||
Discussion
This study investigates the satisfaction with the new practice of TBL in the faculty of Medicine of Sousse among the bloc of critical care for “Disaster management in emergency medicine”.
Our study demonstrates overall students' high level of positive satisfaction with TBL.
Overall, the male and female cohorts agree that TBL in critical medicine is an effective learning process, especially the female group, which is similar to what has been reported in the literature [10]. This highlighted some of the benefits and useful TBL as a precious tool in learning critical medical topics.
Survey data from Parmelee et al. showed that the implementation of this new teaching approach increased students’ satisfaction with teamwork. We believe that this positive perception may be because TBL provided one of the few opportunities for our students to actively discuss and share information and knowledge with other colleagues.
Numerous other studies have evaluated students' feelings about TBL, although they have used different tools to assess it. Irrespective of the category of the population studied and the instrument used, student feedback on this relatively new teaching method was generally judged to be favourable and positive in all the research [11] [12].
The TBL method has been around for over 32 years. Like other innovations, it spread slowly at first, mainly in business education and at the University of Oklahoma, where many of its pioneers were faculty members [5]. This trend has been partly stimulated by the explosion in their use in the scientific field. Moreover, in 1998, TBL was known in medical faculties; today, more than 120 institutions worldwide use this method in their classroom [13].
Apart from the use of team-based learning in various medical school programmes [14] [15] and health training, there is a gap in the literature regarding medical students' attitudes towards team-based learning. Team-based learning was initiated in our medical school in 2017-2018.
During the first two years of a curriculum based mainly on passive receptive teaching, active team learning sessions were offered in all courses, replacing or supplementing lecture-based teaching. We thought it essential to describe students' impressions of teamwork, given that this was a new approach to group teaching in our critical medicine block.
Numerous studies have already described the effectiveness of these methods in learning, mainly from the point of view of specialists, educators and teachers [2] [16]. However, in regard to students' perceptions, it is not always easy to identify a clear choice for the active method over the classic method used. Frame et al. (2015) revealed that learners prefer conventional teaching methods even though they initially have a positive view of active methods, particularly when they have taken courses using both methods in the same session [17].
A research study was conducted with 33 Australian ICU nurses to understand their views of TBL experience. The results indicate that the method is a powerful teaching strategy in terms of student engagement in learning and the outcomes derived from that engagement [18]. Furthermore, to improve learners' learning capabilities, it is important to better understand their conception of the TBL methodology and to identify the facets of this method that need to be perfected.
StudyLimitations
Several potential limitations reduce the possibility of transposing the results to other contexts. For example, the results may be affected by the fact that participation in this study was voluntary and mainly included motivated learners this can introduce a selection bias, as those who choose to participate may be more motivated or have different attitudes to team-based learning (TBL). Another restriction of our research is the fact that long-term effects were not analysed by focusing on a single intervention. Future research could explore the longitudinal effects of Team-Based Learning (TBL) by conducting follow-up assessments to understand its enduring impact on students' perceptions and learning outcomes. This research was restricted by the small participation of candidates, particularly male students.On the other hand, students' lack of familiarity with the modified TBL and the psychological pressure of a busy academic schedule may have played a role in lowering student satisfaction levels, in addition to the use of a self-administered questionnaire, which is more prone to subjectivity.
Using Google Forms with auto marking gave a rapid analysis of students' perception and facilitated the tutor to identify areas of non satisfaction by students to be clarified.
The implementation of Team-Based Learning (TBL) has proven to be a transformative and positively perceived approach among medical students. The findings illuminate a high level of satisfaction and positive attitudes among students, particularly in domains such as professional development, teamwork experience, peer review satisfaction, and the impact of TBL on the quality of learning and clinical reasoning skills.
We considered this study a pilot study for further large studies.
TBL has now been integrated for seven years in our medical school in Sousse, and as this approach has become a fixed part of our medical curriculum and is under development, it would be important to explore the position of our learners. Further study of this type would give us a better idea of the design associated with attitude change when team learning is initially integrated into a block and when it is a truly a part of it.
Conclusion
The study reveals very positive results regarding student satisfaction with team-based learning (TBL) in critical medicine, with an impressive overall satisfaction rate of 79.4%, students strongly approve of TBL as a means of fostering teamwork and collaborative learning experiences. In particular, participants expressed satisfaction in key areas such as peer review, clinical reasoning skills and professional development.
The TBL uses all the levels of knowledge acquisition in Bloom's taxonomy. First, learners use knowledge and comprehension levels through preparatory reading. Then, they call on the higher levels of Bloom's taxonomy, i.e., analysis, re-evaluation and creation, when they are invited to solve a problem in a team and share their solutions with the whole team.
Integrated into our program over the last seven years, e-learning has become a fundamental part of medical education. Getting our students perceptions, we gain valuable insights into the benefits and challenges associated with active learning, contributing to the continuous improvement of medical education strategies.
Active learning methods are now central to the reform of medical studies. Indeed, the new medical education programme aims to adopt teaching approaches that are most likely to lead students to success.
Acknowledgments
The authors would like to acknowledge all the medical trainees who participated in this research and contributed their time. We also express sincere gratitude to the esteemed Committee of Pedagogy at the Faculty of Medicine for their invaluable contribution to the training of teachers in the implementation of Team-Based Learning (TBL), Particularly Dr.Chouchene Imed and Dr.Lasoued Latifa, who played an important role in shaping the successful adoption and application of TBL within our programs. This collaborative effort underscores the importance of ongoing professional development in enhancing teaching methodologies and ultimately enriching the learning experiences of medical students.
Declaration of interest statement:
No conflicts of interest for authors.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Participant consent:
Students were informed at the bottom of the Google forms sheet of the study (anonymity and confidentiality were respected), and it was necessary to check the consent question before completing the questionnaire: written consent
Informed consent obtained from all participants.
References
- Burgess A, Van Diggele C, Roberts C, et al. Team-based learning: design, facilitation and participation. BMC Med Educ 20 (2020): 461.
- Michaelsen LK, Sweet M. The essential elements of team-based learning. New Dir Teach Learn. sept 116 (2008): 7-27.
- Haidet P, Fecile ML. Team-Based Learning: A Promising Strategy to Foster Active Learning in Cancer Education. J Cancer Educ 21 (2006): 125-128.
- How People Learn: Brain, Mind, Experience, and School: Expanded Edition [Internet]. Washington, D.C.: National Academies Press; 2000 [cité 18 juill 2023]. Disponible sur: http://www.nap.edu/catalog/9853
- Haidet P, Kubitz K, McCormack WT. Analysis of the Team-Based Learning Literature: TBL Comes of Age. (2015).
- Pr Ag Jihene Ben Abdallah & Pr Bassem Charfeddine. Scénario d’apprentissage par TBL [Internet]. Faculte de medecine de Sousse; 2018. 12 p. Disponible sur: https://www.medecinesousse.com/useruploads/files/Sc%C3%A9nario-dapprentissage-par-TBL.pdf
- Parmelee D. Medical Students’ Attitudes about Team-Based Learning in a Pre-Clinical Curriculum. Med Educ Online [Internet]. 2009 [cité 17 juill 2023];14. Disponible sur: http://med-ed-online.net/index.php/meo/article/view/4503
- Carless SA, De Paola C. The Measurement of Cohesion in Work Teams. Small Group Res. févr 31 (2000): 71-88.
- Hecht ML. MEASURES OF COMMUNICATION SATISFACTION. Hum Commun Res. juin 4 (1978): 350-368.
- Effectiveness of Team-Based Learning in teaching Medical Genetics to Medical Undergraduates Noor Akmal Shareela IsmaIl Biochemistry Department, Faculty of Medicine, Universiti Kebangsaan Malaysia, Jalan Yaacob Latif, 56000 Kuala Lumpur, Malaysia, Malays J Med Sci. Mar-Apr 23 (2016): 73-77.
- Faezi ST, Moradi K, Ghafar Rahimi Amin A, Akhlaghi M, Keshmiri F. The effects of team-based learning on learning outcomes in a course of rheumatology. J Adv Med Educ Prof 2018; 6 (1): 22-30.
- Teixeira RDC, Magalhaes AB, Palacios VR, et al. Physiotherapy Students’ Perceptions of Team-Based Learning Using the Team-Based Learning Student Assessment. J Educ Learn. 8 (2019): 43.
- Parmelee D, Michaelsen LK, Cook S, et al. Team-based learning: A practical guide: AMEE Guide No. 65. Med Teach. mai 34 (2012): e275-287.
- Sánchez H, Ursell P. Use of Autopsy Cases for Integrating and Applying the First Two Years of Medical Education: Acad Med. mai 76 (2001): 530-531.
- Hunt DP, Haidet P, Coverdale JH, et al. The Effect of Using Team Learning in an Evidence-Based Medicine Course for Medical Students. Teach Learn Med. avr 15 (2003): 131-139.
- Morris J. Implementation of a team-based learning course: Work needed and perceptions of the teaching team. Nurse Educ Today 46 (2016): 146-150.
- Frame TR, Cailor SM, Gryka RJ, Chen AM, Kiersma ME, Sheppard L. Student Perceptions of Team-based Learning vs Traditional Lecture-based Learning. Am J Pharm Educ.
- Currey J, Eustace P, Oldland E, et al. Developing professional attributes in critical care nurses using Team-Based Learning. Nurse Educ Pract. mai 15 (2015): 232-238.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 