Association between Metabolic Syndrome with Subclinical Hypothyroidism
Sharmin Akter1*, Mohammad Maruf Reza2
1Medical Assistant, E-Z Medical Care, New York, United States
2Quality Analyst (Endocrinology), Central Queens IPA, New York, United States
*Corresponding author: Sharmin Akter, Medical Assistant, E-Z Medical Care, 85-50 118th Street, Kew Gardens, NY-11415, United States
Received: 23 December 2021; Accepted: 06 January 2022; Published: 13 January 2022
Article Information
Citation:
Sharmin Akter, Mohammad Maruf Reza. Association between Metabolic Syndrome with Subclinical Hypothyroidism. Archives of Internal Medicine Research 5 (2022): 027-033.
View / Download Pdf Share at FacebookAbstract
Introduction: The worldwide prevalence of metabolic syndrome in the adult population is on the rise and Bangladesh is not an exception. Metabolic syndrome is defined by a constellation of interconnected physiological, biochemical, clinical, and metabolic factors that directly increases the risk of cardiovascular disease, type 2 diabetes mellitus, and all causes of mortality.
Objective: To determine the association of subclinical hypothyroidism with metabolic syndrome.
Materials and methods: The present case-control study was conducted in the department of Internal Medicine, Rangpur Medical College Hospital, Rangpur, Bangladesh from January 2008 to December 2008. Patients of metabolic syndrome were considered as case, while apparently healthy individuals (having no hypertension, central obesity or dyslipidaemia) were taken as control. Metabolic syndrome was defined as having at least three criteria out of five criteria, as recommended by NCEP: ATPIII Diagnostic Criteria for Metabolic Syndrome, while subclinical hypothyroidism was defined, when TSH ranges from 4-20 mU/L with normal FT3 and FT4. Cases were selected from patients attending indoor and outdoor of Medicine Department of RMCH during the study period, while friends and relatives of cases of similar age and sex were selected as control.
Results: In the present study out of 70 cases 48(68.6%) had central obesity (waist circumference > 90 cm for male and > 80 cm for female), 57(81.4%) had raised triglycerides (TG ≥ 150 mg/dl), 61(87.1%) had raised blood pressure (≥130/85), 59(84.3%) had hyperglycemia (fasting blood glucose ≥ 100 mg/dl) and only 11(15.7%) had reduced HDL (<40 mg/dl for male and <50 mg/dl for female) three factors, namely subclinical hypothyroidism,BMI and socioeconomic status were observed to be significantly associated with metabolic syndrome in univariate analysis. After ad
Keywords
<p>Subclinical Hypothyroidism, Metabolic Syndrome, BMI, Risk Factor</p>
Article Details
1. Introduction
The worldwide prevalence of metabolic syndrome in the adult population is on the rise and Bangladesh is not an exception [1]. Metabolic syndrome is defined by a constellation of interconnected physiological, biochemical, clinical, and metabolic factors that directly increases the risk of cardiovascular disease, type 2 diabetes mellitus, and all causes of mortality. Insulin resistance, visceral adiposity, atherogenic dyslipidemia, endothelial dysfunction, genetic susce-ptibility, elevated blood pressure, hypercoagulable state, and chronic stress are the several factors which constitute the syndrome [2]. Metabolic syndrome is now considered as global epidemic [3]. Current estimates revealing that about 20-30% of adult population worldwide affected by this syndrome [4]. The prevalence of metabolic syndrome has increased greatly not only in industrialized nations[5], but also in developing countries as well [6]. In some popul-ations or segments of the population, the prevalence is even higher and its prevalence has been documented as 11–41% [7]. On the other hand, in parts of developing world in which young adults predominate, the prevalence is lower but with increasing affluence and aging of the population, the prevalence undoubtedly is on the rise [8]. Prevalence of metabolic syndrome in USA has been found to be 23.7% [5]. In a multiethnic study in Singapore, 28.8% of Indians, 24.2% of Malaysians 14.8% of Chinese had metabolic syndrome [9]. In Bangladesh the weighted pooled prevalence of metabolic syndrome regardless of gender and criteria used to define metabolic syndrome is 30.0% with high heterogeneity observed. Weighted pooled prevalence of metabolic syndrome is higher in females (32%) compared to males (25%) [1]. Diabetes may affect the thyroid function to variable extent and unreco-gnized thyroid dysfunction not only worsens the metabolic control but also impede the management of diabetes [10]. These similarities in dyslipidemia, hypertension, insulin resistance & dysglycemia in both disorders have lead researchers to posit that metabolic syndrome may be a consequence of some occult abnormality of thyroid gland [11]. As Patients with subclinical hypothyroidism are at an increased risk for atherosclerosis and cardiac manifestations and thus, the thyroxin replacement in these patients has a beneficial effect on the low-density lipoprotein cholesterol levels and the clinical symptoms of hypothyroidism [12].
2. Materials and Methods
This study was a case-control study was conducted in the department of Internal Medicine, Rangpur Medical College Hospital, Rangpur, Bangladesh from January 2008 to December 2008. Total of 140 study subjects were enrolled. Patients of metabolic syndro-me were considered as case, while apparently healthy individuals were taken as control. All cases of metabolic syndrome patients who are diagnosed on the basis of NCEP: ATP III criteria and are 18 years or older as cases. Apparently healthy individuals who were 18 years or above and did not have hyper-tension, diabetes mellitus or central obesity and were willing to participate in the study as control in inclusion critical.
Data were collected on variables of interest using the semi structured questionnaire containing the variables of interest. Both indoor and outdoor basis patient’s data were collected. All cases of metabolic syndrome patients who were diagnosed on the basis of NCEP: ATP III criteria selected as case and persons who did not have hypertension, diabetes mellitus or central obesity were selected as control. The studied variables were age, gender (male and female) occup-ational status, blood pressure, waist circumference, BMI, blood glucose, thyroid function test, lipid profile. Data were collected by face to face interview. The diagnosis of MetS was attained using protocol described by National Cholesterol Education Prog-ram Adult Treatment Panel III which considers that the patient has MetS when three or more risk factors described below are Increased waist circumference, Men: > 40 inches (EURO)/35 inches (SA), Women: > 35 inches (EURO)/31.5 inches (SA), elevated triglycerides > 150 mg/dL or drug treatment for elevated triglycerides, reduced HDL-C Men: < 40 mg/dL ,Women:<50 mg/dL, Elevated blood pressure > 130/85 mm Hg or drug treatment for elevated blood pressure, elevated fasting glucose> 100 mg/dL or drug treatment for elevated glucose.
2.1 Data processing and statistical analysis
Data were processed and analyzed using statistical soft-ware SPSS (Statistical Package for Social Sciences), version 25.0. Both descriptive and infer-ential statistics were used to analyze the data. Prevalence of subclinical hypothyroidism and other confounding variables were compared between case and control groups using Chi-squared (χ2) test, while continuous variables were compared between groups using unpaired t-Test. As more than one factors were found associated with metabolic syndrome in univariate analysis, binary logistic regression analysis was done to find the independent predictors of metabolic syndrome. The level of significance was set at 5% and p-value less than 0.05 was considered statistically significant.
3. Results
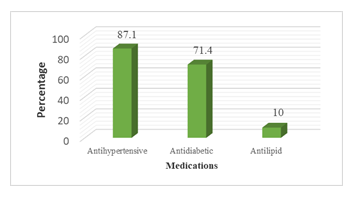
In the present study out of 70 cases 48(68.6%) had central obesity (waist circumference > 90 cm for male and > 80 cm for female). The association of subclinical hypothyroidism with metabolic syndrome patients in RMCH included a total of 70 cases (patients of metabolic syndrome) and an equal number of controls (patients without metabolic syndrome). Of the 70 cases 48(68.6%) had central obesity (waist circumference > 90 cm for male and > 80 cm for female), 57(81.4%) had raised triglycerides (TG ≥ 150 mg/dl), 61(87.1%) exhibited raised blood pressure (≥ 130/85), 59(84.3%) had hyperglycemia (fasting blood glucose ≥ 100 mg/dl) and only 11(15.7%) had reduced HDL (< 40 mg/dl for male and < 50 mg/dl for female) (Table 1). Majority (87.1%) of the cases was under antihypertensive drugs, 71.4% were under antidiabetic drugs and only 10% were receiving anti-lipid drugs (Figure 1). Majority (85.7%) of the cases was overweight or obese compared to 65.7% of the control group (p = 0.006). Overweight and obese individuals carry more than 3-fold (95% CI= 1.3 – 3.9) higher risk of developing metabolic syndrome than the individuals with normal BMI (Table 2). The prevalence of subclinical hypothyroidism was much higher in females (23.1%) than that in males (12.9%) (p = 0.124). The risk of having subclinical hypoth-yroidism in females was found to be 2(95% CI = 0.8 – 5.0) times higher than that in males (Table 3). Subclinical hypothyroidism demonstrated their signi-ficant presence (25.7%) among cases than that among controls (11.4%) (p = 0.030). The risk of having subclinical hypothyroidism among metabolic synd-rome patients (case) 2.7 times more than the non-metabolic syndrome patients (control) which is implied by odd ratio 2.7(95% CI = 1.1 – 6.6). (Table 4).
|
Variables |
Frequency |
Percentage |
|
Central obesity |
48 |
68.6 |
|
Reduced HDL |
11 |
15.7 |
|
Raised triglycerides |
57 |
81.4 |
|
Elevated blood pressure |
61 |
87.1 |
|
Hyperglycemia |
59 |
84.3 |
*Total will not correspond to 100% for multiple responses.
Table 1: Distribution of cases by their metabolic syndrome components (n=70).
|
Demographic characteristics |
Group |
p-value |
Odds Ratio (95% CI of OR) |
|
|
Case (n = 70) |
Control (n = 70) |
|||
|
BMI (kg/m2) * |
||||
|
Overweight & obese |
60(85.7%) |
46(65.7%) |
0.006 |
3.1(1.3 – 7.2) |
|
Normal |
10(14.3%) |
24(34.3%) |
||
|
Mean ± SD |
27.7 ± 3.1 |
26.0 ± 2.5 |
||
Figures in the parentheses indicate corresponding %;
*Chi-squared Test (c2) was done to analyze the data.
Table 2: Association between BMI and metabolic syndrome.
|
Subclinical hypothyroidism |
Sex |
p-value |
Odds Ratio (95% CI of OR) |
|
|
Female (n = 78) |
Male (n = 62) |
|||
|
Present |
18(23.1%) |
8(12.9%) |
0.124 |
2.0(0.8 – 5.0) |
|
Absent |
60(76.9%) |
54(87.1%) |
||
Figures in the parentheses indicate corresponding %;
*Chi-squared Test (c2) was done to analyze the data.
Table 3: Association between subclinical hypothyroidism and sex.
|
Subclinical hypothyroidism |
Group |
p-value |
Odds Ratio (95% CI of OR) |
|
|
Case (n = 70) |
Control (n = 70) |
|||
|
Present |
18(25.7%) |
8(11.4%) |
0.030 |
2.7(1.1 – 6.6) |
|
Absent |
52(74.3%) |
62(88.6%) |
||
Figures in the parentheses indicate corresponding %;
*Chi-squared Test (c2) was done to analyze the data.
Table 4: Association between subclinical hypothyroidism and metabolic syndrome.
4. Discussion
The study found that factors, namely subclinical hypothyroidism, BMI and socioeconomic status to be significantly associated with metabolic syndrome in univariate analysis. After adjustment by binary logistic regression analysis, all these three variables persisted to be significantly associated with meta-bolic syndrome with risk of having the condition being 2.3(95% CI = 0.9 – 5.8) times higher in subclinical hypothyroidism, 2.3(95% CI = 1.4 – 8.1) times higher in overweight/obese individuals and 2.8(95% CI = 1.3 – 5.8) times more in patients with affluent socioeconomic class (p = 0.038, p = 0.007 and p = 0.006 respectively) than those from their respective counterpart. Diverse reports have sugge-sted that the presence of metabolic syndrome can lead to a higher risk for subclinical hypothyroidism [13]. The largest cohort study conducted on 66,822 participants with and without metabolic syndrome Chang and associates [13], made an average follow-up of 4.2 years to see the incident rates for subclinical hypothyroidism. This study show prevalence of subclinical hypothyroidism was considerably higher among females with metabolic syndrome (31.6%) than that among their male (18.8%), although the difference did not turn to significant (p=0.221). Cases were relatively older than the controls (p=0.120) and subclinical hypothyroidism is more common in elderly people. Cases more often belonged to affluent class (upper middle class and rich) and obese individuals than the controls. The positive correlation between subclinical hyperthyroidism and obesity may be due to increased TSH levels in obese individuals include neuroendocrine dysfunction, leptin-induced hypothalamic-pituitary axis alteration, and thyroid hormone resistance due to partially bio-inactive TSH protein. Studies have reported a correlation between TSH and leptin which might indicate that leptin might have an important role in the link between TSH and obesity [14]. Metabolic syndrome appears to be a risk factor for subclinical hypothyroidism. In the context of higher cardiovascular risk associated with subclinical hypothyroidism and the metabolic syndrome, the current analysis suggest that thyroid dysfunction may be one intermediate factor between metabolic syndrome and cardiovascular disease [14]. Subclinical hypothyroidism has clinical importance because of its high prevalence (4–20%), the risk of progression to overt hypothyroidism, and consequ-ences associated with cardiac and lipid abnormalities [15]. In a retrospective study found treatment of subclinical hypothyroidism with levothyroxine was associated with fewer ischemic heart disease events in the younger individuals, supporting a beneficial effect of thyroid hormone on cardiovascular risk fact-ors in hypothyroid patients [16]. This study has found that subclinical hypothyroidism is more common among female patients than male. The prevalence of subclinical thyroid dysfunction among female subj-ects were higher than those among male subjects in the present study, which is consistent with previous reports. Because subclinical thyroid dysfunction is not rare among the elderly and is more common in women, it is necessary to evaluate the thyroid func-tion among elderly women to identify the possible presence of subclinical thyroid dysfunction [16].
5. Conclusion
It concluded that subclinical hypothyroidism might be associated metabolic syndrome. Subclinical hypo-thyroidism demonstrated their significant presence (25.7%) among cases than that among controls (11.4%). The study found that factors, namely sub-clinical hypothyroidism.
References
- Rahim M, Khan AA, Sayeed M, et al. Metabolic syndrome in rural Bangladesh: comparison of newly proposed IDF, modifi-ed ATP III and WHO criteria and their agree-ments. Diab Metabolic Syndrome 1 (2007): 251-257.
- Mohan V, Deepa M. The metabolic syn-drome in developing countries. Diabetes Voice 51 (2006): 15-17.
- Park YW, Zhu S, Palaniappan L, et al. The metabolic syndrome: prevalence and asso-ciated risk factor findings in the US population from the third National Health and nutrition examination survey, 1988-1994. Arch Intern Med 163 (2003): 427-436.
- Stern MP, Williams K, González-Villa-lpando C, et al. Does the metabolic syndro-me improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease?. Diabetes Care 27 (2004): 2676-2681.
- Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 365 (2005): 1415-1428.
- Hildrum BCB, Mykletun A, Hole T, et al. Age-specific prevalence of the metabolic syndrome defined by the International Dia-betes Federation and the National Choles-terol Education Program: the Norwegian HUNT 2 study. BMC Public Health 7 (2007): 220.
- Misra A, Misra R, Wijesuriya M, et al. The metabolic syndrome in south Asians: contin-uing escalation and possible solutions. Indian J Med Res 125 (2007): 345-354.
- Rahim M, Khan AA, Sayeed M, et al. Metabolic syndrome in rural Bangladesh: comparison of newly proposed IDF, modi-fied ATP III and WHO criteria and their agreements. Diab Metabolic Syndrome 1 (2007): 251-257.
- Hu G, Qiao Q, Tuomilehto J, et al. Prevalence of the metabolic syndrome and its relation to all cause and cardiovascular mort-ality in nondiabetic European men and wom-en. Arch Intern Med 164 (2004): 1066-1076.
- Ford ES. Prevalence of the metabolic synd-rome defined by the international diabetes federation among adults in the US. Diabetes Care 28 (2005): 2745-2749.
- Földes J, Bános C, Winkler G. Subclinical Hypothyroidism and Arteriosclerosis. Orvo-si Hetilap, 145 (2004): 1601-1607.
- Walsh J P, Bremner A P, Bulsara M K, et al. Subclinical Thyroid Dysfunction as a Risk Factor for Cardiovascular Disease. Archives of Internal Medicine 165 (2005): 2467-2472.
- Biondi B, Cooper D S. The Clinical Signi-ficance of Subclinical Thyroid Dysfun-ction. Endocrine Reviews 29 (2008): 76-131.
- Surks M I, Hollowell J G. Age-Specific Dis-tribution of Serum Thyrotropin and Antithy-roid Antibodies in the Us Popu-lation: Impli-cations for the Prevalence of Subclinical Hy-pothyroidism. The Journal of Clinical Endo-crinology & Metabolism 92 (2007): 4575-4582.
- Huber G, Staub J-J, Meier C, et al. Prospective Study of the Spontaneous Course of Subclinical Hypothyroidism: Pro-gnostic Value of Thyrotropin, Thyroid Reserve, and Thyroid Antibodies. The Journal of Clinical Endocrinology & Metabolism 87 (2002): 3221-3226.
- Hollowell J G, Staehling N W, Flanders W D, et al. Serum Tsh, T4, and Thyroid Anti-bodies in the United States Population (1988 To 1994): National Health and Nutrition Examination Survey (Nhanes Iii). The Jour-nal of Clinical Endocrinology & Metabolism 87 (2002): 489-499.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 