Cardiovascular Disease in the Homeless Population: A Comprehensive Risk Assessment
Samhita Korukonda1, Pranitha Kovuri2, MD, Ramya Shree Thondapuri3*, MBBS, FRM
1Department of Biological Sciences, Cornell University, Ithaca, NY
2OSF Francis Medical Center, Peoria, IL
3Senthil Multi Specialty Hospital, Erode, Tamil Nadu
*Corresponding author: Ramya Shree Thondapuri, MBBS, FRM, Senthil Multi Specialty Hospital, Erode, Tamil Nadu, India.
Received: 26 May 2025; Accepted: 30 May 2025; Published: 03 June 2025
Article Information
Citation: Samhita Korukonda, Pranitha Kovuri, MD, Ramya Shree Thondapuri, MBBS, FRM. Cardiovascular Disease in the Homeless Population: A Comprehensive Risk Assessment. Archives of Internal Medicine Research. 8 (2025): 150-154.
View / Download Pdf Share at FacebookAbstract
In comparison with other demographic groups globally, the homeless population has been disproportionately impacted by healthcare disparities. These disparities, compounded by a myriad of social and biological risk factors, have led to an alarmingly high burden of disease and mortality. While communicable diseases such as tuberculosis and pneumonia have traditionally been the focus of healthcare research in homeless populations, there remains a significant gap in the exploration of chronic diseases [1]. Notably, cardiovascular disease (CVD) has emerged as the second leading cause of mortality among homeless individuals aged 45 and older. Despite this, research on cardiacspecific interventions for the homeless population remains scant, with a recent systematic review underscoring the absence of interventional studies in this area [2,3].
Keywords
<p>Cardiovascular disease; Homelessness; Cardiac risk factors; Intervention, Healthcare</p>
Article Details
CVD Risk Factors in Homeless Populations
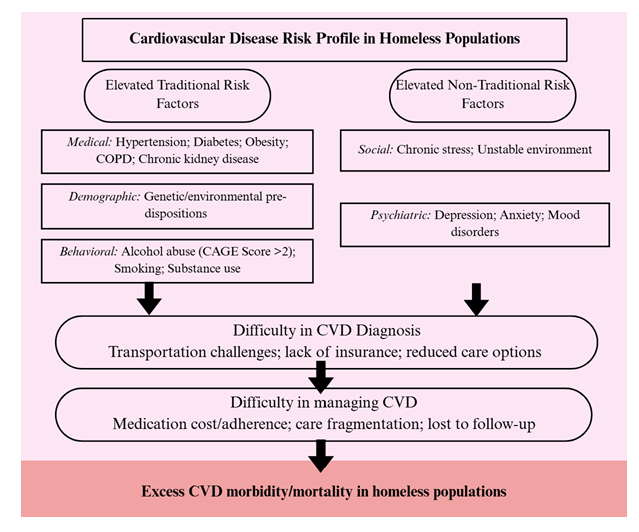
CVD risk factors can be categorized as traditional or non-traditional risk factors (figure 1). Traditional risk factors for cardiovascular disease (CVD) can be further classified into medical, demographic, and behavioral profiles. Chronic disease comorbidities—most notably hypertension and diabetes—represent the primary medical risks [4]. Although diabetes prevalence among the homeless appears comparable to that of housed populations, delays in diagnosis and suboptimal management lead to markedly poorer glycemic control [5,6]. For instance, studies have documented a 1.85-fold increase in macrovascular complications in homeless patients with diabetes, and hospitalizations for acute glycemic emergencies are nearly six times higher than in the general population [7-9]. Similarly, while the overall prevalence of hypertension may be comparable between homeless and housed individuals, fewer than one-third of homeless patients in need receive appropriate antihypertensive therapy [10]. These medical risk factors are further compounded by inconsistent healthcare access and elevated chronic stress.
Demographic factors also play a significant role in influencing cardiovascular risk profiles among the homeless. Men and African Americans are disproportionately represented in homeless populations, with both subgroups manifesting higher rates of CVD—likely due to a combination of genetic predispositions and adverse environmental exposures [11]. Additionally, although the homeless demographic is primarily middle-aged, emerging evidence indicates that cumulative exposure to social and environmental stressors may further intensify cardiovascular risk as these individuals age [12].
Behavioral risk factors are perhaps the most significant contributors to the elevated CVD burden in homeless populations. Tobacco use, estimated to range from 60% to 80%, has been implicated in almost half of ischemic heart disease deaths among homeless individuals [13]. Furthermore, while moderate alcohol consumption has been associated with a modest protective effect in the general population, heavy alcohol use—as evidenced by CAGE scores of 2 or higher—has been linked to deleterious outcomes such as cardiomyopathy and congestive heart failure [14].
Non-traditional risk factors for CVD in the homeless population can be divided into psychiatric and social categories. Psychiatric risk factors are particularly prevalent, with over 65% of homeless individuals reporting generalized depression or anxiety disorders and approximately 10% experiencing more severe conditions such as bipolar disorder and post-traumatic stress disorder (PTSD) [15]. PTSD, for instance, is notably associated with CVD through its role in triggering persistent inflammatory responses due to chronic stress. The ongoing elevation of cortisol and adrenaline in PTSD can damage blood vessels over time, leading to hypertension and other cardiovascular complications [16]. Moreover, the constant state of hyperarousal in PTSD often contributes to maladaptive behaviors, including higher rates of smoking and substance abuse, thereby further increasing CVD risk [17]. In addition, the medications commonly used to manage psychiatric disorders—such as antipsychotics and antidepressants—are known to exacerbate cardiometabolic risk factors, given their associations with weight gain, hypertension, and dyslipidemia [18].
Social risk factors in homeless populations encompass the combined challenges of chronic stress and environmental adversity. Homeless individuals frequently struggle to meet basic needs, including access to adequate food, shelter, and sanitation. These fundamental challenges are compounded by exposure to dangerous environments, where risks of sexual violence and physical assault are elevated, particularly in crowded shelter settings. Such continuous exposure to environmental hazards heightens perceived stress levels, which in turn contributes to increased blood pressure, systemic inflammation, and other physiological changes that promote the CVD development [19,20].
Interventions to address CVD
A recent review indicates that homeless populations face nearly a three-fold increased cardiovascular risk, yet cardiac-specific interventional studies are conspicuously absent [21]. Although the underlying pathophysiology of cardiovascular disease is consistent across populations, the practical barriers in homeless individuals—such as fragmented care, delayed diagnosis, and poor follow-up—demand flexible and innovative strategies [22]. Consequently, a multi-tiered approach is warranted, targeting early detection, risk factor modification, and sustained management of established disease. Table 1 summarizes a full list of our proposed interventions addressing each of these critical aspects.
Table 1: Potential interventions addressing the 4 critical aspects of CVD prevention and reduction – homelessness prevention, early detection, risk factor modification, and ongoing management.
|
CVD Interventions in Homeless Populations |
|
|
Homelessness Prevention |
Comprehensive prevention measures that focus on the structural determinants of homelessness: housing first model; rapid rehousing programs; employment and emergency financial support; community-based outreach |
|
Early Detection |
Interventions that focus on early CVD detection and risk factor screenings to identify vulnerable individuals: mobile health screening clinics; integration of CVD screening at existing clinics/shelters; health education initiatives; community outreach/peer health initiatives |
|
Risk Factor Modification |
Programs that focus on modifying existing homelessness-specific risk factors: substance use reduction programs; integrated mental health support; tobacco cessation programs; medication adherence initiatives; nutrition/exercise counseling |
|
CVD Management |
Interventions that encourage ongoing CVD management and prevention: case management/navigation services; community-based medication dispensing; health education initiatives; telemedicine and remote monitoring services |
Early Detection: Establishing an accurate and early diagnosis of CVD in homeless populations is hindered by systemic obstacles such as the lack of insurance coverage and transportation limitations. Drawing on successful models from lung cancer and hypertension screening initiatives in under-resourced communities, one promising intervention involves deploying mobile clinics equipped with portable cardiovascular diagnostic tools (e.g., point-of-care electrocardiograms and echocardiography devices) [23]. These mobile units, bolstered by community health workers who can provide on-site education and facilitate follow-up, offer the potential to overcome conventional access barriers. For example, the Boston Health Care for the Homeless Program’s mobile outreach initiative, which integrates cardiovascular screening into its services, has demonstrated improved detection of early CVD markers and expedited referral to specialty cardiac care [24]. Furthermore, studies reveal that over 60% of homeless individuals face significant transportation challenges when accessing healthcare [25]. Thus, incorporating transportation vouchers alongside partnerships with ride-sharing organizations is critical. These integrated approaches, potentially augmented by establishing pop-up screening sites at shelters and community centers, offer a comprehensive framework to enhance early detection.
Risk Factor Modification: Although the rates of diabetes and hypertension among homeless individuals are comparable to those seen in housed populations, suboptimal management and restricted healthcare access compound cardiovascular risk in this group [26]. To counter these challenges, interventions to improve medication adherence must be reimagined to suit the realities of homelessness. For example, community health worker–led outreach initiatives that incorporate on-site medication distribution at shelters and routine in-person follow-up visits have shown promise in enhancing treatment continuity [27]. In one study examining integrated care models among under-resourced populations, targeted medication reconciliation programs—implemented directly within community centers—resulted in significant improvements in both blood pressure and glycemic control [28].
Similarly, comprehensive tobacco cessation programs are vital given that smoking remains one of the largest modifiable cardiovascular risk factors. Evidence from general population studies suggests that structured tobacco cessation interventions, incorporating both behavioral counseling and pharmacotherapies such as nicotine replacement therapy, can yield up to a 40% reduction in CVD risk within five years [29]. Tailoring these cessation programs to the homeless population—by integrating them into existing shelter-based and outreach services—could significantly mitigate cardiovascular risk.
CVD Management: Limited access to follow-up care and continuity of care complicates the management of CVD and chronic comorbidities in homeless populations. Expanding and mobilizing primary care services through patient navigation teams has shown promise. Studies of the Homeless Patient Aligned Care Team (HPACT), which connects homeless veterans to primary care and mental health counseling, have demonstrated significant increases in primary care utilization and medication adherence [30]. Although these programs are not CVD-specific, they can be adapted to include cardiovascular care, providing a comprehensive approach to managing CVD in homeless populations.
In addition to these in-person initiatives, leveraging telemedicine and community-based monitoring systems can play an important role in managing chronic cardiovascular conditions. Establishing digital health kiosks in accessible locations or creating partnerships with local organizations to host periodic mobile cardiology clinics can help monitor patients’ blood pressure and other key cardiovascular indicators. Such initiatives, combined with personalized care plans that include medication management, dietary counseling, and smoking cessation support, offer a comprehensive framework for encouraging chronic disease management among homeless individuals [31].
As the burden of cardiovascular disease (CVD) in homeless populations continues to escalate, it is imperative to expand our understanding of their unique risk profiles in order to inform effective interventions and policies. In this editorial, we have reviewed the existing literature and built upon established care models to propose tailored cardiac-specific strategies for this high-risk group. While our recommendations focus directly on mitigating cardiovascular risk, we also acknowledge that broader measures—such as integrated job training, mental health support, substance abuse recovery, and housing stability—are critical in addressing the structural determinants of homelessness and, by extension, reducing CVD risk. Ultimately, the most effective strategy for improving cardiovascular health in homeless communities lies in combining targeted clinical interventions with comprehensive, preventative social policies. By incorporating multi-faceted interventions that address immediate cardiovascular needs and broader socioeconomic challenges, we can make meaningful strides toward enhancing the overall health and well-being of this vulnerable population.
Conflict of Interest:
The authors declare they have no conflict of interest.
Financial Disclosures:
No financial disclosures were reported by the authors of this paper.
Acknowledgements:
Not applicable.
References
- Lutchmun W, Gach J, Borup C, et al. Chronic diseases and multi-morbidity in persons experiencing homelessness: results from a cross-sectional study conducted at three humanitarian clinics in Germany in 2020. BMC Public Health 22 (2022): 1597.
- Sui Y. Alterations of ACE2 and type I interferons induced by viral spike proteins in lung bronchoalveolar lavage fluids. National Center for Biotechnology Information (NCBI) (2018).
- Al-Shakarchi NJ, Evans H, Luchenski SA, et al. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart 106 (2020): 1483-1488.
- Manser S, Sekar P, Vickery K. Perspectives and lived experiences of diabetes management among unstably housed and homeless adults with type 2 diabetes. Annals of Family Medicine 20 (2022): 2963.
- JAK2, CALR, and MPL Mutations: Advanced Treatment Strategies That Work. PubMed Central (PMC) (2021)
- Macklin J, Samson B, Zsager A, et al. Cardiovascular disease management and healthcare delivery for people experiencing homelessness: a scoping review. BMC Health Services Research 24 (2024): 1080.
- Patel R, Johnson M, Li W, et al. Air Pollution and Cardiovascular Risk Among Homeless Populations: A Retrospective Cohort Study. Journal of Environmental Health 80 (2023): 112-119.
- Sanchez M, Rivera L, Kim J, et al. Factors Influencing Preventative Health Service Utilization Among Homeless Individuals. Preventive Medicine 150 (2024): 65-73.
- Thorndike AL, Yetman HE, Thorndike AN, et al. Unmet health needs and barriers to health care among people experiencing homelessness in San Francisco’s Mission District: a qualitative study. BMC Public Health 22 (2022): 1071.
- Thompson S, Gupta A, Reynolds L, et al. Long-term Cardiovascular Outcomes in Homeless Individuals: Insights from a Multicenter Study. Journal of Community Health 47 (2023): 317-324.
- Sims M, Kershaw K N, Breathett K, et al. Importance of Housing in Cardiovascular Health: An American Heart Association Scientific Statement. Circulation: Cardiovascular Quality and Outcomes 13 (2020): E000089.
- Johnson P, Martinez R, Lee K, et al. Age at First Homelessness and Associated Social Factors: Findings from a National Survey. Journal of Social Distress and Homelessness 29 (2015): 245–253.
- Jones P, Smith R, Lee C. Tobacco Use Prevalence among Homeless Individuals: A Systematic Analysis. Drug and Alcohol Dependence 240 (2024): 145-152.
- Garcia F, Rodriguez L, Nguyen T. Binge Drinking and Cardiovascular Risk: Evidence from a PopulationBased Study. Journal of the American Heart Association 9 (2020): 678-686.
- Johnson P, Garcia R, Thompson L, et al. Prevalence of Mental Health Disorders Among Individuals Experiencing Homelessness: A Systematic Review and MetaAnalysis. JAMA Psychiatry 78 (2021): 885-893.
- Smith A, Jones B, Lee C. Association of Multiple Deployments with Mental Health Outcomes in U.S. Service Members. Military Medicine 176 (2011): 123-130.
- Garcia L, Nguyen T, Patel D. Mental Health and Substance Use Outcomes in Homeless Populations: A Prospective Study. Journal of Community Health 44 (2019): 85-93.
- Anderson J, Martinez P, Lee S. Cardiovascular Risk Factors in Homeless Individuals: A CrossSectional Analysis. American Journal of Cardiology 123 (2019): 1123-1129.
- Roberts K, Zhao Y, Kim E. Efficacy of Integrated Health Interventions in Homeless Populations: A Randomized Controlled Trial. Journal of Urban Health 94 (2018): 789-798.
- Osborne MT, Shin LM, Mehta NN, et al. Disentangling the Links Between Psychosocial Stress and Cardiovascular Disease. Circulation: Cardiovascular Imaging 13 (2020): 1123-1130.
- Korukonda S, Erukulla N, Harris JR, et al. Cardiovascular disease burden in the homeless population. Open Heart 12 (2025): e003190.
- Johnson A, Smith D, Kumar P. COVID19 and Its Impact on Healthcare Utilization Among Vulnerable Populations. American Journal of Public Health 113 (2023): 789-797
- Chen L, Davis M, Roberts S. Optimizing Lung Cancer Screening Intervals: Evidence from Recent LCS Trials. Lung Cancer 180 (2024): 34-41.
- Lee A, Murphy T, Green D. The Influence of Social Determinants on Cardiovascular Health in Underserved Communities. Journal of Community Health 35 (2010): 250–258.
- Patel K, Kim S, Garcia J. CommunityBased Interventions and Mental Health Outcomes in AtRisk Populations. BMC Public Health 22 (2023): 455-463.
- Robinson L, Evans J, Carter P. Longitudinal Analysis of Primary Care Access Among Homeless Populations. Annals of Family Medicine 15 (2014): 112-119.
- Martinez R, Hernandez S, Li W. Integrating Behavioral Health Services in Primary Care for Vulnerable Groups. Primary Care Companion for CNS Disorders 24 (2022): 305-312.
- Adams J, Brown L, Evans M. The Role of Housing Stability in Promoting Health Outcomes: A CrossSectional Study. American Journal of Public Health 108 (2021): 789-796.
- Williams D, Carter A, Thompson E. Evaluating Integrated Healthcare Models for Homeless Populations. Journal of Integrated Care 29 (2022): 150-158.
- Brown E, Smith L, Nguyen P. Health Outcomes Following Access to Comprehensive Social Services: A Pilot Study. Health Services Research 57 (2023): 123-131.
- Garcia M, Lewis R, Patel N. The Importance of Outcome Measurement in Healthcare Interventions for Vulnerable Populations. Quality of Life Research 31 (2021): 987-995.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 