Impact of the COVID-19 Pandemic on Florida Medical Students’ Wellbeing and Academic Experience During “Lockdown”
Shadi A. Baajour, Waseem Wahood, Kate J. F. Carnevale*
Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Fort Lauderdale, FL, USA
*Corresponding Author: Kate J. F. Carnevale, Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Fort Lauderdale, FL, USA
Received: 11 July 2022; Accepted: 20 July 2022; Published: 18 October 2022
Article Information
Citation:
Shadi A. Baajour, Waseem Wahood, Kate J. F. Carnevale. Impact of the COVID-19 Pandemic on Florida Medical Students’ Wellbeing and Academic Experience During “Lockdown”. Archives of Internal Medicine Research 5 (2022): 471 - 480.
View / Download Pdf Share at FacebookAbstract
Introduction: The global pandemic of coronavirus disease 2019 (COVID-19) has continued to demonstrate considerable impacts on all aspects of life, as well as mental health across populations. Medical students may be considered a particularly vulnerable population during the COVID-19 pandemic due to the compounding mental stress of a demanding medical education.
Methods: A cross-sectional online survey was designed for medical students in the state of Florida, USA, to collect their perceptions of the impact of COVID-19 on their personal daily habits, perceived social connectedness, academic outlook, and anxiety levels using a General Anxiety Disorder 7-item (GAD-7) scale.
Results: From the ten medical schools in Florida, 96 students responded. 94% of student respondents felt the COVID-19 pandemic impacted their academic experience, but only 55% of students felt their medical school adequately mitigated the negative effect of the pandemic on their education, psychological well-being, and personal health. GAD-7 analysis revealed 36 students with mild, 15 with moderate, and 6 with severe anxiety symptoms. Students rated interruption of daily habits and feeling others were not following health guidelines as the most influential factors for their increased anxiety. Factors related to decreased anxiety were communication with family, practicing relaxation techniques, and avoiding public exposure.
Discussion: Increased levels of anxiety were common amongst students during the pandemic. Students should be encouraged to seek appropriate resources and outlets to mitigate the effects of anxiety on their psychological well-being and academic success.
Keywords
<p style="text-align:justify">COVID-19 pandemic; Medical student; Anxiety and depression; Wellness; Distance learning; Academic impact</p>
Article Details
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) which causes coronavirus disease 2019 (COVID-19), was first identified in December 2019. [1] As of August 12, 2020, it was responsible for over 737,417 deaths around the world according to the World Health Organization (WHO), and the state of Florida (FL) in the United States of America (US) reported over 65,000 cases and 2,712 deaths. [2] The US declared a “State of Emergency” in March of 2020, and in the same month, FL announced an executive order to limit non-essential travel and business known as the stay-at-home or “lockdown” order. [3] At the same time, there was a record-high number of requests for unemployment benefits within the state, indicating significant stress on individuals from all socioeconomic backgrounds. [4] Medical students are a particularly vulnerable population with high levels of stress due to the amount of time spent studying along with personal pressures influenced by high expectations. [5] Even prior to the global pandemic, medical education has been shown to significantly affect stress levels due to factors such as role transition, decreased sleep, relocation, and feelings of isolation. [6] A prospective cohort study from 2010 analyzed 740 interns across 13 U.S. hospitals and found that the incidence of depression increased from 3.9% to 25.7% during their internship year. [7] Thus, analyzing the issues that may be plaguing medical students during a pandemic, and acquiring their attitudes and perspectives, is an integral part of furthering our understanding in this field.
Additionally, during the pandemic, medical schools have had to transition both pre-clerkship lectures and clerkship didactic sessions to online teaching modalities. A cross-sectional survey of medical students across 40 United Kingdom (UK) medical schools evaluated the benefits and barriers of virtual curriculum. Students reported a perceived benefit of increased flexibility, but a proportion of students cited family distraction and poor internet connection to be barriers to their education. [8] However, the additional impacts of online classes on medical students’ psychological well-being was not analyzed.
The aim of this study is to explore the thoughts of Florida medical students during the Florida stay-at-home “lockdown” order on their personal daily habits, perceived social connectedness, academic outlook, and anxiety levels. With this information, we hope to educate medical students regarding the impact that an unexpected interruption to medical school curriculum can have, as well as avenues medical schools can explore in the future to navigate similar circumstances.
Methods
Study rationale
A cross-sectional research study was designed to survey medical students who were enrolled in the state of Florida as of March 2020, when COVID-19 led to declaration of a national emergency in the US. Due to the transition to online learning by every medical school in the state of Florida at that time, the need to understand how the transition to online coursework impacted medical students necessitated development of a survey that queried medical students in Florida about their perceptions of the impact of the pandemic on their medical education and mental health.
Study design
The survey had five broad categories. After obtaining students’ consent to participate, basic demographic information was gathered. The survey then questioned students on their perceptions of how their daily habits had changed due to the COVID-19 pandemic (much less, less, no change, more, much more). The third section surveyed students’ general knowledge and sources of information regarding COVID-19. Next, students were asked to report effects of the COVID-19 pandemic on their personal safety, social connectedness, academic success, and their perception of their individual medical school’s actions to mitigate the negative impact of the pandemic on students. Text boxes allowed for subjective, qualitative responses. Finally, we surveyed participants’ anxiety levels by administering a General Anxiety Disorder 7-item (GAD-7) scale, with each item coded from zero to three, per the frequency of different anxiety symptoms. A score of 10 or greater is diagnostic of general anxiety disorder (GAD) with a sensitivity of 89% and a specificity of 82%[9]. We asked participants to specify what they believed had caused an increase or decrease in their anxiety levels. Our study was deemed exempt by the Nova Southeastern University Institutional Review Board (IRB # 2020-292) and was distributed online via school affiliated emails using REDCap (Research Electronic Data Capture) software,[10] with the help of participating medical school student affairs offices. Students were able to submit their response online from June 18th to August 10th, 2020.
Subjects’ selection
The medical schools surveyed were: Florida International University Herbert Wertheim College of Medicine (FIU), Florida State University College of Medicine (FSU), Nova Southeastern University Dr. Kiran C. Patel College of Osteopathic Medicine (NSU DO), Nova Southeastern University Dr. Kiran C. Patel College of Allopathic Medicine (NSU MD), University of Central Florida College of Medicine (UCF), University of Florida College of Medicine (UF), University of Miami Miller School of Medicine UM), and University of South Florida Health Morsani College of Medicine (USF). While also located in Florida, Florida Atlantic University Charles E. Schmidt College of Medicine (FAU) and Lake Erie College of Osteopathic Medicine - Bradenton Campus (LECOM) declined to participate in the study. The total population of medical students in the state of Florida at the time was 5744. The survey was distributed through the Office of Student Affairs at each medical school, utilizing student email listservs to forward the survey web link, an informational flyer, and the researchers’ contact information. The survey was available online for 8 weeks.
Statistical Analysis
GAD-7 categorical scores were created. A score of 0-4 was indicative of no observed anxiety, 4-9 denoted mild anxiety, 10-14 was moderate, and 15-21 was indicative of severe anxiety. All categorical variables were reported as n (%) and all continuous variables were reported as median (intraquartile range) or mean (standard deviation). A Fisher’s exact test was used to assess if any of the demographic variables, including age, gender, school, year in medical school, and number of people residing in respondents’ households, were confounders for the GAD-7 categorical scores.
Qualitative Analysis
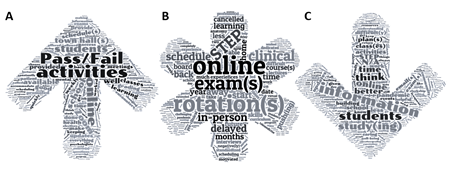
Free responses collected from student respondents were analyzed holistically for common themes across respondents, as well as analyzed by WordCloud online software to generate graphical representations of the most commonly used words or word-groupings (displayed as larger relative font size) amongst all responses in the categories of impact on medical school experience, student perceptions of what medical schools did well, and student perceptions of areas for improvement for their medical schools during the pandemic.
Results
Demographic Information
As can be seen in Supplemental Table S1 in the supporting information, a total of 96 responses were received: 32 (33.3%) from UF; 25 (26.0%) from NSU MD; 16 (16.7%) from FSU; 11 (11.5%) from UCF; 7 (7.29%) from NSU DO; 5 (5.21%) from FIU; and no responses were obtained from USF or UM, in addition to FAU and LECOM which declined to participate (Table S1). As seen in Supplemental Table S1, most of the student respondents were in the age range of 22-25 years old (n=58, 60.4%), and 59 respondents identified as female (61.5%), with one student responded as “not listed” as their gender. Third-year students made up most of the respondents (n=36, 38%). Approximately on-fifth of respondents reported living alone during the pandemic (n=19, 19.8%), with most respondent reporting one 30.2% (n=29) or more housemates, and only 10.4% (n=10) reporting five or more individuals, including themselves, residing in their household during the pandemic (Supplemental Table S1).
Personal Habits
Some of the personal habits that increased in frequency during the pandemic included hand-washing for at least 20 seconds (n=55, 58% responded with “More”), using more sanitizers (n=41, 42.7% responded with “More”), using personal protective equipment (PPE: such as masks or gloves) in public (n=76, 79.2% responded with “Much more”), avoiding non-essential travel (n=47, 49.0% responded with “Much More”), maintaining distance from non-essential businesses (n=48, 51.1% responded with “Much More”), avoiding contact with people (n=57, 60.0% responded with “Much More”), cooking at home (n=45, 46.9% responded with “More”), and communicating with others via phone or video (n=44 45.8% responded with “More”). The personal habits that a majority of respondents reported “no change” in frequency were the following: hair/nail grooming (n=69, 72.0%), household chores (n=58, 60.4%), regular exercise (n=28, 29.2%), ordering takeout (n=30, 31.3%), alcohol consumption (n=53, 55.2%), recreational drug use (n=85, 89.5%), nighttime sleep (n=43, 44.8%), and daytime sleep (n=53, 55.2%).
COVID-19 Knowledge
All respondents agreed that “The symptoms of COVID-19 include: cough, shortness of breath, fever, chills, muscle pain, sore throat, new loss of taste or smell”; 88 (91.7%) agreed that “SARS-CoV-2 RNA has been detected in upper and lower respiratory tract specimens, blood, and stool specimens”; 86 (89.6%) disagreed that “Patients who were diagnosed with COVID-19 are definitively known to be immune to reinfection after they recover”; 68 (70.8%) agreed that “UV light and disinfectants (like bleach) are effective at killing SARS-CoV-2 on non-porous surfaces”.
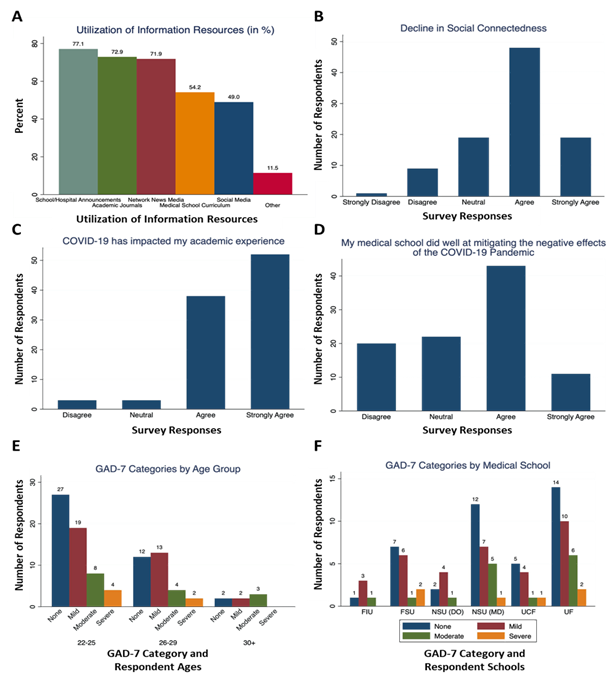
Figure 1A shows the results of respondents when asked to choose their sources of reference information regarding COVID-19 from a list of options. A total of 74 (77.1%) respondents reported that they received information from school/hospital announcements; 70 (72.9%) received information from academic journals; 69 (71.9%) received information from network/news media; 52 (54.2%) from medical school curriculum; and 47 (49.0%) respondents chose that one of their sources for COVID-19 information was social media (Figure 1A).
Effects of the COVID-19 Pandemic
A total of 86 (89.6%) respondents stated that they “followed the Florida stay-at-home mandate to limit non-essential activities” and 79 (82.3%) agreed or strongly agreed that they felt that they are “safe and prepared at home during the Stay-At-Home mandate”. Of the 96 student respondents, 67 (69.8%) agreed or strongly agreed that “My feelings of social connectedness have declined during the COVID-19 pandemic” (Figure 1B), 90 (93.8%) agreed or strongly agreed that “The COVID-19 pandemic has impacted my academic experience” (Figure 1C), and 54 (56.3%) agreed or strongly agreed that “My medical school has done well at mitigating the negative effect of the COVID-19 pandemic on my education, psychological well-being, and personal health,” with only 20 (20.8%) disagreeing with this statement (Figure 1D).
Anxiety levels of medical students
As can be seen in Table 1, Median GAD-7 score was 5 (3.00-8.75), and the average was 6.28 (+/-4.87). A total of 41 (42.7%) respondents were considered to have no anxiety, 34 (35.4%) were in the mild anxiety category, 15 (15.6%) were in the moderate anxiety category, and 6 (6.25%) were considered to be experiencing severe anxiety, according to their score. Higher relative instances of anxiety were noted in older age groups compared to younger, although more participants would be needed to determine any statistical correlation (Figure 1E). Similarly, respondents from NSU MD and UF displayed lower relative rates of anxiety than respondents from FIU, FSU, NSU DO and UCF, but sample sizes were limited for each of the latter (Figure 1F). Respondents were asked questions regarding what factors they considered to increase and decrease their anxiety. The statement ranked to cause the greatest increase in anxiety for respondents was “interruption of daily activities” with 71 (74.0%), followed by “Feeling others are not following guidelines” (n=66, 68.8%). A total of 81 (84.3%) respondents agreed that “communicating with friends and family” decreased their anxiety levels, followed by “practicing relaxation activities (exercise, meditation, prayer, arts & crafts, etc.)” with 67 (69.8%) (Table 1).
|
GAD-7 Category |
||||
|
Severe |
Moderate |
Mild |
None |
|
|
Overall |
6 (6.3%) |
15 (15.6%) |
34 (35.4%) |
41 (42.7%) |
|
Factors that Increased Anxiety |
Severe |
Moderate |
Mild |
None |
|
Direct exposure to someone with COVID-19 |
0 (0%) |
3 (20%) |
8 (23.5%) |
4 (9.8%) |
|
Feeling symptoms of COVID-19 |
2 (33.3%) |
5 (33.3%) |
5 (14.7%) |
6 (14.6%) |
|
Testing positive for COVID-19 |
0 (0%) |
1 (6.67%) |
0 (0%) |
2 (4.9%) |
|
Losing a loved one to COVID-19 |
1 (16.7%) |
3 (20%) |
4 (11.8%) |
5 (12.2%) |
|
Other physical health conditions |
1 (16.7%) |
3 (20%) |
5 (14.7%) |
4 (9.8%) |
|
Mental health |
4 (66.7%) |
11 (73.3%) |
18 (52.9%) |
8 (19.5%) |
|
Financial instability. |
2 (33.3%) |
5 (33.3%) |
7 (20.6%) |
5 (12.2%) |
|
Family physical health |
4 (66.7%) |
5 (33.3%) |
11 (32.4%) |
13 (31.7%) |
|
Family mental health |
3 (50%) |
8 (53.3%) |
11 (32.4%) |
6 (14.6%) |
|
Economic downturn |
2 (33.3%) |
8 (53.3%) |
10 (29.4%) |
12 (29.3%) |
|
Job insecurity |
0 (0%) |
3 (20%) |
2 (5.9%) |
5 (12.2%) |
|
Interruption of daily activities |
5 (83.3%) |
13 (86.7%) |
25 (73.5%) |
28 (68.3%) |
|
Feeling others are not following guidelines |
6 (100%) |
13 (86.7%) |
23 (67.7%) |
24 (58.5%) |
|
News updates on COVID-19 |
3 (50%) |
13 (86.7%) |
14 (41.2%) |
15 (36.6%) |
|
Living alone |
1 (16.6%) |
6 (40%) |
8 (23.5%) |
5 (12.2%) |
|
Living with family |
1 (16.67%) |
5 (33.33%) |
8 (23.53%) |
7 (17.1%) |
|
Factors that Decreased Anxiety |
Severe |
Moderate |
Mild |
None |
|
Positive attitudes from your colleagues |
3 (50%) |
5 (33.3%) |
13 (38.2%) |
20 (48.8%) |
|
Educating yourself on COVID-19 |
2 (33.3%) |
6 (40%) |
14 (41.2%) |
20 (48.8%) |
|
Practicing relaxation activities (exercise, meditation, prayer, arts & crafts, etc.) |
4 (66.7%) |
10 (66.7%) |
25 (73.5%) |
28 (68.3%) |
|
Communicating with friends & family |
6 (100%) |
14 (93.3%) |
28 (82.4%) |
33 (80.5%) |
|
Avoiding exposure in public |
6 (100%) |
11 (73.3%) |
24 (70.6%) |
20 (48.8%) |
|
Feeling others are following guidelines |
3 (50%) |
4 (26.7%) |
10 (29.4%) |
10 (24.4%) |
|
Focusing on current personal affairs |
2 (33.3%) |
5 (33.3%) |
15 (44.1%) |
18 (43.9%) |
|
Living alone |
0 (0%) |
0 (0%) |
4 (11.8%) |
4 (9.8%) |
|
Living with family |
1 (16.7%) |
2 (13.3%) |
12 (35.3%) |
17 (41.5%) |
Table 1: Calculated GAD-7 scores for survey respondents, as well as self-reported factors contributing to or detracting from respondent anxiety by GAD-7 Category, Severe, Moderate, Mild and None. Numbers of respondents given with percentages in parentheses.
Figure 1: Medical student survey results: (A) percentage of respondents who used hospital/school announcements (teal), academic journals (green), network/news media (red), medical school curriculum (orange), social media (blue) or other (pink) information sources about the pandemic [total exceeds 100% as respondents were able to select multiple sources]; (B) Respondent self-reported feelings of social connectedness during the pandemic; (C) Respondent self-reported impact of the pandemic on their academic experience; (D) Respondent self-reported impression of their medical school’s response to mitigating the effects of the pandemic; (E) Correlation of respondents’ age group and (F) respondents’ medical school affiliation with the respondent self-reported General Anxiety Disorder 7-item scale score category: none (blue), mild (red), moderate (green), severe (yellow), numbers of respondents per category are given above each column.
Confounding Analysis
The data was assessed for confounding variables that could have provided any significant difference in GAD-7 scores. After analysis, no differences were found related to gender (p=0.070), age group (p=0.617), medical school (p=0.95), year in medical school (p=0.208), nor number of people residing in household (p=0.605), regarding distribution of GAD-7 categorical scores.
Qualitative Analysis
Free-response prompts were utilized to gain a more complete understanding of respondent perceptions (Figure 2). The question regarding “what your school did well during the pandemic” had a variety of answers, but the overarching themes included mental health services, faculty checking-in on their students, and course directors being less stringent, such as moving classes to pass/fail grades (Figure 2A). When asked how students perceived that the pandemic had affected their academic experience, student respondents indicated that changes to online instruction with no in-person labs or clinical experiences, along with delays of the clinical rotation schedule, and need for Step 1 examination rescheduling, were the major factors impacting their academic experiences (Figure 2B). The majority of students responded to the question, “Please describe what your school could have done better,” with communication between administrators and students, lowering tuition fees since classes became virtual, and awareness of the difficulty of studying for board exams during a pandemic (Figure 2C). The question, “Please describe any factors that made you feel underprepared or unsafe during the stay-at-home mandate,” garnered answers involving house members traveling, financial instability, and lack of emotional support. When students were asked to “Please describe what has affected your feeling of social connectedness” they reported feelings of isolation with no roommates, not being able to go to restaurants and bars, and use of electronic means of keeping in touch with others rather than being together in-person.
Figure 2: Pictorial representation of the qualitative free-responses to (A) what respondents believed their medical schools did well, (B) the ways the pandemic impacted respondents’ medical education, (C) what respondents perceived as areas where their medical schools could have done better. In each graphic, created in WordCloud, the larger the word appears, the more frequently it occurred in the free responses.
Discussion
Conclusion and Implications
In the United States alone, deaths secondary to COVID-19 are estimated at 570,537 as of May 2021.[11] The COVID-19 pandemic is still having a significant effect on the health, economic, environmental, psychological, and social well-being of the world-wide population. It is the most challenging threat to international public health in modern history and will likely impact daily life for the foreseeable future. The information gathered from the survey data demonstrated that the COVID-19 pandemic also had a measurable impact on medical students in the state of Florida. This study aimed to quantify and qualify the effects of the COVID-19 pandemic on a cohort of medical students during the Florida stay-at-home “lockdown” order.[3] Florida medical student respondents were found to rely most on school and/or hospital announcements, then academic journals, and then news media for information related to COVID-19 during the “lockdown” period, with a smaller portion of their information coming from medical school curriculum or social media (Figure 1A). This indicates that the FL medical student respondents were more likely to use more reputable informational resources than social media to stay informed about COVID-19, as social media has been shown to carry more misinformation about COVID-19 and information seeking on social media has been correlated with a lower ability to critically evaluate the validity of COVID-19 information.[12,13] Additionally, during the “lockdown” timeframe in FL (March to May), 69.8% of medical student respondents reported agreeing or strongly agreeing that they experienced a decline in social connectedness (Figure 1B), as is expected with the loss of in-person curricular activities, as well as limited or fully virtual social interactions with classmates, friends, and family. Unsurprisingly, Florida medical student respondents nearly unanimously agreed or strongly agreed (93.8%) that COVID-19 had impacted their medical school experience with only 6.2% of respondents reporting neutral or no effect (Figure 1C). Prior to the COVID-19 pandemic, the general incidence of anxiety amongst medical students was measured to be 33.8%.[9] This study found 57.2% of respondents reported either mild, moderate, or severe anxiety during the COVID-19 stay-at-home orders in FL.
Analysis of response data indicated that a majority of student respondents had some level of anxiety according to their GAD-7 scores, 55 out of 96 students (57.3%). Medical student age and medical school size may provide inverse protective effects against student anxiety, but more data are needed to form a definitive correlation (Figure 1E & F). Although the effects of the pandemic altering academic and social experiences has contributed to this increase in anxiety across student populations,[14–16] when compounded with the baseline stress of medical school curriculum, it is evident that the COVID-19 pandemic affected medical student anxiety substantially. Although 54 student respondents (56.3%) agreed with the statement, “My medical school has done well at mitigating the negative effect of the COVID-19 pandemic on my education, psychological well-being, and personal health,” greater than 40% of students stated they disagreed or felt neutral regarding this statement (Figure 1D), indicating there may be more that medical schools could do to improve conditions for their students. The common positive theme identified by qualitative analysis was a transition of classes to pass/fail, and a negative theme was the lack of adequate communication (Figure 2). Medical schools could focus on bolstering these two aspects of student support in the future to ensure that students feel they are provided with adequate assistance during challenging transitional periods.
In a recent study documenting the effect of the COVID-19 pandemic on medical students in Libya, a higher level of anxiety and depression (31.3%) was found among medical students during the pandemic, as opposed to before (10.5%).[17] Similarly, a study from Saudi Arabia measured an increase in anxiety and feelings of emotional detachment from loved ones and peers.[18] In addition, a study from the UK described a decrease in final year medical students’ feelings of preparedness and confidence as they transitioned into the medical profession.[19] In Sao Paolo, Brazil, COVID-19 impacted medical education at the pre-clerkship level as teachers struggled with technology and implementation of videoconferences and interactive learning sessions, as well as keeping students engaged in discussion, which led to a decrease in quantity and quality of lectures. Furthermore, students were anxious about when and how they would be graded, and when they would make up in-person practical sessions. This anxiety was compounded by the months of social isolation.[20] These findings correlate with the results of this study, indicating potential commonalities for medical students facing the pandemic on different continents.
A proposed method to reduce medical students’ symptoms of anxiety and depression could be inclusion of targeted community programs and communication practices. One such mechanism could potentially be the introduction of a peer-mentorship through a social media platform pairing senior and junior medical students. A recent study found that senior students, who were trained in learning methods, communication skills, and effective consulting techniques were effective in providing wellness guidance to junior students.[21] Senior students assisted by providing input such as stress relaxation techniques, engaging in exercise, continuing online contact with family and friends, time management, and best learning strategies for online learning. A post-intervention questionnaire found that 71% of junior medical students believed the platform had a significant impact on helping them adjust.[21]
In planning for the future, a qualitative study aimed to develop a model for utilizing distance learning in medical schools post-COVID used a 63-item assessment tool to evaluate faculty, student, social, and logistic issues.[22] Overall, participants agreed that face-to-face instruction allowed for better student inspiration, more meaningful personal connections, and better development of professionalism, cognitive, communication and clinical skills. And while distance learning can be a successful learning modality for many students, Ahmed and coworkers found that students with financial challenges and special needs may not have equal opportunities to access technology, thus the logistics for conducting distance learning can be quite complicated.[22]
Study Limitations
As the COVID-19 pandemic has progressed, there has been increasing evidence of disease hotspots around the United States[1] and other countries.[23–26] Since our study only sampled medical students in the state of Florida, an understanding of the full effect that the COVID-19 pandemic had on medical students in other locations can only be inferred. The exact nature of the pandemic effects on medical students is likely dependent on local organization and government rules and regulations. How severely specific communities were and continue to be impacted, and what response and support measures medical schools provide to students will also play a role. However, the results of this study can be used to generalize the effects that stressful events and hardships may have on medical students. This study did not address factors related to local disease prevalence or differences in public perceptions of COVID-19 to determine their impact on medical students. Another limitation of this study was that the survey was distributed in June through August 2020. During this time, the FL stay-at-home orders had been lifted, and restrictions on social interactions were being eased. This time-lag in data collection, after the actual “lockdown” period, could have impacted the participants perspectives and responses. Additionally, the relatively small sample size of this study (below 5% for most schools, except NSU MD at 16%) limited the results found. Additionally, students who were more anxious or who expressed greater concern may have been more inclined to participate in the survey and share their opinions, thus potentially skewing results compared to the whole FL medical student population.
Future Considerations
In the particularly vulnerable population of medical students – who are increasingly affected by stress, financial burden, and social isolation – medical schools might better provide support to their students by working to build safeguards for their students in the event of future unexpected interruptions in curriculum. These safeguards might include mentorship programs, availability mental health and counseling resources, and designated open and frequent communications with students. Future studies evaluating the effect of COVID-19 on medical students’ wellbeing and education outcomes at time points post-pandemic will provide increasing insight regarding the COVID-19 pandemic’s full effects on medical students.
Acknowledgements
The authors would like to thank the dedicated medical students and medical schools throughout the state of Florida for their participation in our survey, and their drive to continue succeeding in and advancing medical education.
Declarations
Funding:
This study was not financially supported.
Conflicts of interest/Competing interests:
The authors claim not conflict of interest.
Availability of data and material:
Data will be made available upon request. Please email the corresponding author at kcarneva@nova.edu.
Code availability:
Not applicable
Ethics approval:
The study was revied by the Nova Southeastern University Institutional Review Board and granted exemption # 2020-292
Consent to participate and for publication: Informed consent was obtained from each survey participant and no identifying information was collected.
References
- Helmy YA, Fawzy M, Elaswad A, Sobieh A, Kenney SP, Shehata AA. The COVID-19 Pandemic: Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J Clin Med Res 9 (2020).
- Organization WH, Others. Coronavirus disease ( COVID-19): situation report, 200. World Health Organization; (2020).
- [cited 2021 May 18]. Available from: https://www.flgov.com/wp-content/uploads/orders/2020/EO_20-91-compressed.pdf
- [cited 2021 May 18]. Available from: https://www.dol.gov/ui/data.pdf
- Nechita F, Nechita D, Pîrlog MC, Rogoveanu I. Stress in medical students. Rom J Morphol Embryol 55 (2014): 1263-1266.
- Goldman ML, Shah RN, Bernstein CA. Depression and suicide among physician trainees: recommendations for a national response. JAMA Psychiatry 72 (2015): 411-412.
- Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter J, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry 67 (2010): 557-565.
- Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open BMJ 10 (2020): e042378.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166 (2006): 1092-1097.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42 (2009): 377-381.
- COVID-19 policy briefings (2020). 2020 [cited 2021 May 18]. Available from: http://www.healthdata.org/covid/updates
- Dadaczynski K, Okan O, Messer M, Leung AYM, Rosário R, Darlington E, et al. Digital health literacy and web-based information-seeking behaviors of university students in Germany during the COVID-19 pandemic: Cross-sectional survey study. J Med Internet Res 23 (2021): e24097.
- Datta R, Yadav AK, Singh A, Datta K, Bansal A. The infodemics of COVID-19 amongst healthcare professionals in India. Med J Armed Forces India 76 (2020): 276-283.
- Pokhrel S, Chhetri R. A literature review on impact of COVID-19 pandemic on teaching and learning. High educ future. SAGE Publications 8 (2021): 133-341.
- Copeland WE, McGinnis E, Bai Y, Adams Z, Nardone H, Devadanam V, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry 60 (2021): 134-141.
- Kee CE. The impact of COVID-19: Graduate students’ emotional and psychological experiences. J Hum Behav Soc Environ 31 (2021): 476-488.
- Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One 15 (2020): e0242905.
- Meo SA, Abukhalaf AA, Alomar AA, Sattar K, Klonoff DC. COVID-19 pandemic: Impact of quarantine on medical students’ mental wellbeing and learning behaviors. Pak J Med Sci Q [Internet]. Pakistan Journal of Medical Sciences 36 (2020): S43-48.
- Choi B, Jegatheeswaran L, Minocha A, Alhilani M, Nakhoul M, Mutengesa E. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Med Educ. 20 (2020): 206.
- Chinelatto LA, Costa TR da, Medeiros VMB, Boog GHP, Hojaij FC, Tempski PZ, et al. What you gain and what you lose in COVID-19: Perception of medical students on their education. Clinics (Sao Paulo). Fundacao Faculdade de Medicina 75 (2020): e2133.
- Rastegar Kazerooni A, Amini M, Tabari P, Moosavi M. Peer mentoring for medical students during the COVID-19 pandemic via a social media platform. Med Educ 54 (2020): 762-763.
- Ahmed SA, Hegazy NN, Abdel Malak HW, Cliff Kayser W 3rd, Elrafie NM, Hassanien M, et al. Model for utilizing distance learning post COVID-19 using (PACT)TM a cross sectional qualitative study. BMC Med Educ. 20 (2020): 400.
- Roy S, Bhunia GS, Shit PK. Spatial prediction of COVID-19 epidemic using ARIMA techniques in India. Model Earth Syst Environ (2020): 1-7.
- Das A, Ghosh S, Das K, Basu T, Dutta I, Das M. Living environment matters: Unravelling the spatial clustering of COVID-19 hotspots in Kolkata megacity, India. Sustain Cities Soc 65 (2021): 102577.
- Hallal PC, Victora CG. Overcoming Brazil’s monumental COVID-19 failure: an urgent call to action. Nat Med (2021).
- Ridde V, Gautier L, Dagenais C, Chabrol F, Hou R, Bonnet E, et al. Learning from public health and hospital resilience to the SARS-CoV-2 pandemic: protocol for a multiple case study (Brazil, Canada, China, France, Japan, and Mali). Health Res Policy Syst 19 (2021): 76.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 