Osteoblastoma-Like Osteosarcoma of the spine: A Case Report and Review of the Literature
Omar Atallah, MBBS, FRCS Neurosurgery1*, Aaron Stevenson, MBBS, FRACS Orthopedic and Spine1
1Spine Department, Royal Adelaide Hospital, Adelaide, South Australia
*Corresponding Author: Omar Atallah, MBBS, FRCS Neurosurgery, Spine Department, Royal Adelaide Hospital, Adelaide, South Australia.
Received: 29 January 2024; Accepted: 05 February 2024; Published: 07 February 2024
Article Information
Citation: Omar Atallah, MBBS, FRCS Neurosurgery, Aaron Stevenson, MBBS, FRACS Orthopedic and Spine. Osteoblastoma-Like Osteosarcoma of the spine: A Case Report and Review of the Literature. Journal of Spine Research and Surgery. 6 (2024): 01-05
View / Download Pdf Share at FacebookAbstract
Background:
OBLOS of the spine is an extremely rare tumor, with 12 cases have been reported in the literature. We present a case of OBLOS affecting the thoracic spine. We also review similar cases in literature.
Clinical Presentation:
A 19-year-old male patient presented to our center with an incidental T7 lesion with a complain of back pain for 2 weeks with altered sensation starting from T7 dermatomal distribution below. Neuro examination showed no significant neurological deficits. He underwent tumor excisional surgery over 2 occasions. Last follow up images showed tumor recurrence despite treatment.
Conclusion:
OBLOS in general is an aggressive tumor and yet best modality of treatment is early surgical excision. Future research should be carried out to determine the best method of adjuvant treatment modality for OBLOS.
Keywords
Osteosarcoma; Osteoblastoma; Osteoblastoma Like Osteosarcoma; Spine Tumor; Neurosurgery; Spine Surgery
Osteosarcoma articles; Osteoblastoma articles; Osteoblastoma Like Osteosarcoma articles; Spine Tumor articles; Neurosurgery articles; Spine Surgery articles
Article Details
Abbreviations list:
CT: Computed Tomography; MRI: Magnetic Resonance Imaging; OBLOS: Osteoblastoma Like Osteosarcoma; COS: Conventional Osteosarcomas; Osteosarcoma NOS: Osteosarcoma Not Otherwise Specified.
Introduction
Osteoblastoma like osteosarcoma (OBLOS) has been described as malignant or aggressive form of osteoblastoma [1] that behaves like osteosarcoma [8]. OBLOS is a rare variant of osteosarcoma, which estimated to be 1% of all osteosarcomas [6]. OBLOS is listed within the malignant osteogenic tumors, under the subdivision of Osteosarcoma Not Otherwise Specified (NOS) as per 2020 WHO classification of tumors of bone [9]. Spine is one of the most common places affected by OBLOS [6]. In this article we will report a case of spinal OBLOS with literature review of affected spinal cases.
Case Presentation:
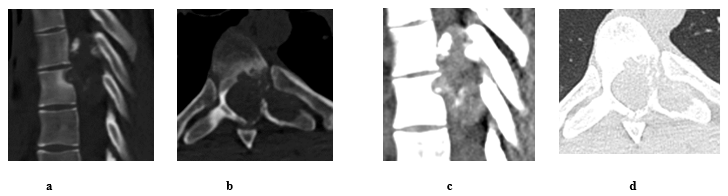
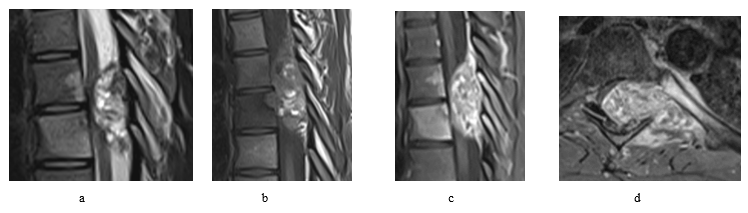
The patient was 19-year-old at time of presentation in early January/2023. He was presented to our spine unit with an incidental finding of T7 lytic lesion with extensive soft tissue involvement (Figure 1 and 2) as seen on CT first, followed by MRI scans. The CT images had been performed as a follow up scans for a previous spontaneous pneumothorax that has been treated for its recurrence with video-assisted thoracoscopic surgery (VATS) combined with left upper lobe apical wedge resection (a bleb inside) and talc pleurodesis in early June/2022. Back then, the x-rays and CT scans for the chest didn’t show a convincing mass lesion (some early lytic changes have been noticed in advance at left T7 pedicle thought to be benign). At presentation, patient had reported 2-week history of back pain and altered sensation from abdomen below with unsteadiness on feet. On exam, patient found to have normal power on limbs, reduced sensation from T7 below and hyperreflexia of knee and ankle. Otherwise, examination was normal. PET scan didn’t show any metastatic lesions.
Based on images, differential diagnosis was osteosarcoma, osteoblastoma and atypical giant cell tumor.
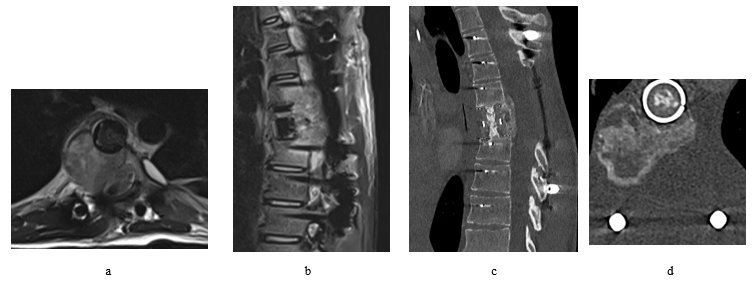
Figure 1: Pre op spinal CT scan shows a lytic mass lesion on bone window sagittal (a) and axial (b) cuts causes nearby soft tissue and intracanalicular extension with intralesional calcifications as seen on soft tissue window sagittal (c) and axial (d) cuts. It extends behind T6 and T7 with epicentre arising from left body/pedicle of T7. Differential diagnosis based on images Osteoblastoma, Aneurysmal bone cyst and Malignant lesion.
Figure 2: Pre op spinal MRI shows aggressive osseous lesion centred at the left T7 pedicle with large soft tissue component. The extra-dural soft tissue extension results in complete effacement and compression of the thoracic cord at the T6-T7 level. Given the aggressive appearance and multiple vertebral level involvement, this is favoured to represent an osteosarcoma but an aggressive osteoblastoma remains a differential as does an aneurysmal bone cyst (though this is felt less likely)
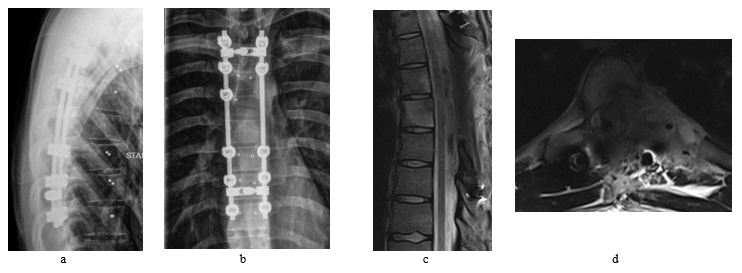
The patient underwent interventional tumor embolization followed the next day by a T4-T10 fusion with posterior decompression and gross total tumor resection. The screws were carbon-based implants and the procedure was carried out with assistance of O-arm, neuromonitoring and a navigation system. Patient had recovered well after the surgery and post-operative MRI revealed a radical resection of the tumor without any complications (Figure 3).
Histopathological analysis of the tumor showed multiple fragments of bone forming tumor composed of anastomosing trabeculae of woven bone with a prominent osteoblastic lining and intervening fibrovascular stroma. In areas, the osteoblastic cells are arranged in solid areas and showed cytological atypia and mitotic activity. Focal ace-like osteoid deposits are also present in these areas. Diffuse aneurysmal bone cyst like lesions are also seen. MDM2 amplification are not detected. Immunohistochemistry showed that scattered tumor cells express c-FOS, FOSB and H3-3. G34W is negative. These features favor an osteoblastoma like osteosarcoma.
After 3 months of the surgery, follow up MRI scans were performed which had revealed recurrence of the tumor within the surgical bed with further bony destruction and epidural extension (Figure 4). The patient underwent T7 vertebrectomy followed by cage implantation then debulking of the residual tumor via left sided transthoracic approach. Patient has developed high fluid output per chest tube found to be due to CSF leakage which has been treated successfully conservatively, other than that, patient had made smooth recovery.
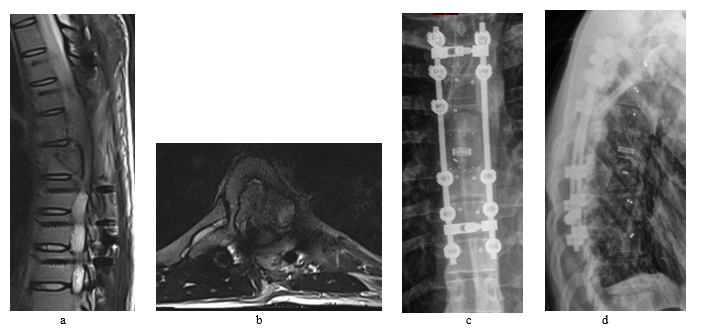
Follow up MRI and CT scans 4 months after the second surgery had revealed aggressive recurrence of the tumor invading nearby tissue and displacing the cord to the left (Figure 5). No metastatic deposits had been found so far on the follow up scans.
Adjuvant radiation therapy (50 Gray in 25 sessions) had been started after recovery and completed in mid-August/2023. Follow up post radiation CT scans showed continuing tumor growth.
Figure 5: Despite all efforts fighting the tumor, follow up images shows recurrence of the tumor that aggressively invading the nearby structures. The MRI was performed 4 months after the second surgery (a + b). CT scans (c + d) were performed after the adjuvant radiation treatment, 7 months from the second surgery.
At time submitting this article, patient was receiving chemotherapy MAP (methotrexate [M] doxorubicin [A] and Cisplatin [P]) that has started in October/2023 with few treatments related side effects and generalized deconditioning. Neuro exam so far is as baseline. No clinical and radiographical evidence so far that chemotherapy and radiotherapy are treating the tumor or controlling its progression.
Discussion:
OBLOS is a rare tumor, and being in the spine is very rare with only 12 cases (including our case) have been reported in the literature (Table 1). Until now, spine has been considered the second most common place to be involved with OBLOS after tibia [8]. The first reported case of OBLOS within the spine was in 1985 for a patient that has been diagnosed with it in 1962 [1]. In 5 of those 12 cases, tumor was incorporating the thoracic spine, 5 in the cervical spine, 1 in the sacrum and one was identified to be in spine without mentioning the exact location. Range of ages at presentation is between 16 to 58 with slight male predominance. It has been noticed in literature that the most common presentation of OBLOS regardless of the affected bone is pain of short duration, on the other hand, pain related to osteoblastoma tend to be of longer duration[8]. Tumor had recurred in 7 of the recorded spine cases regardless of the mode of the treatment. Cases with spinal OBLOS that had complicated with metastasis, lung was the only recorded organ to be affected. It has been noticed in general that lung is the most common affected organ with metastasis in OBLOS [2,8]. Aim of surgery in general was to remove as much as possible of the tumor, as it has been believed that wide surgical resection is the treatment of choice for this tumor [6] without any strong evidence yet supporting the best modality of treatment and whether chemotherapy or radiotherapy are beneficial. With the spine cases recorded, OBLOS had a bad prognosis, 6 of the 12 cases were died with a life span ranging between 6 to 36 months from time of diagnosis. 1 case has no record of follow up and 5 of the 12 cases were alive at time of submitting the articles (including ours) with follow up ranging between 9 to 120 months.
No: Number, G: Gender, F: Female, M: Male, C: Cervical spine, T: Thoracic spine, Chemo: Chemotherapy, Radio: Radiotherapy, FU: Follow up. R: Reference. Jan: January. Apr: April. Oct: October. Nov: November. Dec: December.
Table 1: Recorded cases with spinal OBLOS in literature.
Conclusion:
We have reported an extremely rare tumor affecting the spine with an overview of similar cases. OBLOS in general is an aggressive tumor and yet best modality of treatment is early surgical excision. Future research should be carried out to determine the best method of adjuvant treatment modality for OBLOS.
Declaration of Interest Statement:
The author(s) declared no potential conflicts of interest.
References
- Bertoni F, Unni KK, McLeod RA, et al. Osteosarcoma resembling osteoblastoma. Cancer 55 (1985): 416-426.
- Bertoni F, Bacchini P, Donati D, et al. Osteoblastoma-like osteosarcoma. The Rizzoli Institute experience. Mod Pathol 6 (1993): 707-716.
- Radig K, Schneider-Stock R, Haeckel C, et al. p53 gene mutations in osteosarcomas of low-grade malignancy. Hum Pathol 29 (1998): 1310-1316.
- Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol 125 (2006): 555-581.
- Corradi D, Wenger DE, Bertoni F, et al. Multicentric osteosarcoma: clinicopathologic and radiographic study of 56 cases. Am J Clin Pathol 136 (2011): 799-807.
- Gambarotti M, Dei Tos AP, Vanel D, et al. Osteoblastoma-like osteosarcoma: high-grade or low-grade osteosarcoma? Histopathology 74 (2019): 494-503.
- Camino Willhuber G, Kido G, Estefan M, et al. Osteoblastoma-like osteosarcoma of the cervical spine: a case study. Rev Asoc Argent Ortop Traumatol 84 (2019): 149-154.
- Wu W, Zhao G, Chen J, et al. Osteoblastoma-Like Osteosarcoma of the Cuboid and Skull: A Case Report and Review of the Literature. J Foot Ankle Surg 59 (2020): 156-161.
- Choi JH, Ro JY. The 2020 WHO Classification of Tumors of Bone: An Updated Review. Adv Anat Pathol 28 (2021): 119-138.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 