Percutaneous Lumbar Disc Radiofrequency Intervention-With a Review of Newer Lumbar Disc Steerable Plasma Coblation Devices
Dr Rajendra Tiruchelvarayan1*,
1Senior Consultant Neurosurgeon, Spine Neuro Specialist Centre, Gleneagles Medical Centre, Singapore.
*Corresponding Author: Dr Rajendra Tiruchelvarayan. Senior Consultant Neurosurgeon, Spine Neuro Specialist Centre, Gleneagles Medical Centre, Singapore.
Received: 27 August 2025; Accepted: 11 September 2025; Published: 16 September 2025
Article Information
Citation: Dr Rajendra Tiruchelvarayan. Percutaneous Lumbar Disc Radiofrequency Intervention-With a Review of Newer Lumbar Disc Steerable Plasma Coblation Devices. Journal of Spine Research and Surgery. 7 (2025): 91-97.
View / Download Pdf Share at FacebookAbstract
Background:
Lumbar disc disease and prolapsed intervertebral discs(PID) are common conditions. They cause debilitating lower back pain, sciatica. Proven surgical treatments includes lumbar microdiscectomy. However, this comes with effects of muscular, soft tissue disruption, and the potential surgical complications. Recently, interventional devices utilising thermal heating energy(eg. IDET®), and radiofrequency plasma coblation nucleoplasty have been introduced. Since 1999, a straight cannula needle probe nucleoplasty device(Nucleoplasty®) has been introduced. Newer navigable decompression device options(eg. Yesdisc®) can directly treat contained disc herniations, and discogenic pain. The RF Coblation tip can be directed accurately to the actual damaged disc site, for targeted decompression.
Objectives:
To compare the different percutaneous lumbar disc radiofrequency devices and their efficacy. We also assess if the newer navigable plasma coblation devices are more effective.
Methods:
In our article, we searched PubMed and Medline for relevant studies on Percutaneous Lumbar Disc Thermal Ablation, RF Devices for lower back pain. We searched for studies on the efficacy of newer Navigable Coblation Devices. We also reviewed our personal experience with the above devices. The primary outcome measures were improvement in Visual Analogue Scores(VAS) by 50% at 6 months duration or more. Other indices included the Owestri Disability Index(ODI).
Study Results and Discussion:
In the treatment of discogenic pain treatment, devices such as IDET® and Biacuplasty® have shown modest improvement results in pain relief. The improvement in VAS ranges from 40% to 57%. For the IDET procedure, cases of complications such as catheter shearing were found to have have occurred. Percutaneous laser disc decompression shows promising results, ranging from 60-70% improvement in 6 month VAS scores. This procedure requires care, as cases of thermal injury to the vertebral end-plates have been reported. For nucleoplasty devices(which can treat both a herniated disc and discogenic pain), we find the results of navigable coblation devices(eg.Yesdisc and L’Disq) were better(VAS improvement ranging from 68.5% to 88%), when compared to the older straight cannula nucleoplasty device(VAS improvement ranging from 53-60% at 12 months). These results are also demonstrated in the author’s personal intervention series of 61 procedures. The incidence of complications such as discitis, neural damage were low(less than 1%).
Conclusion:
Percutaneous lumbar disc RF intervention has an important role in managing persistent lower back pain. A variety of intervention devices have been introduced. Thermal RF ablation of the annular pain fibres has been shown to be moderately effective in improving discogenic pain. For contained disc herniations, lumbar disc plasma coblation using navigable devices such as Yesdisc® show promising results. Encouraging VAS results are shown, ranging from 70% to 88%, with low procedural risks. This should be considered a good treatment option in selected cases. Further larger scale studies are needed in the future to assess this.
Keywords
<p>Lumbar disc radiofrequency ablation; Plasma coblation nucleoplasty; Discogenic pain; Contained disc herniation</p>
Article Details
Introduction
The burden of lower back pain affecting patients around the world is significant. The prevalence has been studied and can range from 25% to as high as 40% [1,2]. This condition not only affects the health of patients, but also presents an economic burden due to lost days of work [3]. Conservative treatment with analgesic medications, and a physiotherapy programme can resolve this condition in many patients.
The back pain can be of a radicular type, discogenic type, or commonly a combination of both. For persistently symptomatic patients, many interventional treatment modalities have been developed with varying degree of documented success. Minimally invasive percutaneous treatment techniques have been developed as alternatives to the classical microdiscectomy surgery. These techniques avoid the side effects of surgery which include the soft tissue/muscular disruption, and associated complications. The integrity of the annulus fibrosus is also preserved with these techniques [34]. The overall treatment goals would to be to relieve both the radicular and back pain. Over the years, medical product technology has been developing rapidly. There have been a variety of percutaneous devices introduced and studied. However these have shown a range of inconsistent treatment results [4].
The percutaneous disc ablation devices introduced to treat discogenic pain include IDET® and Flextrode®Boston Scientific. These create a thermal lesion targeting the posterior disc annulus pain fibres, to reduce pain from this lumbar spine pain generator source [5].
Subsequently, devices to treat the herniated disc nucleus pulposus as the pain generator source were developed. The first central plasma coblation nucleoplasty device was introduced in 1999(ArthroCare® Co.Sunnyvale CA). This consisted of a straight cannula, and was introduced via a posterolateral approach, via Kambin’s triangle, delivering coblation plasma energy to the nucleus pulposus [6].
This aimed to decrease the central intradiscal pressure, to allow the prolapsed disc fragment to implode inwards. A number of trials were carried out using this device with a wide range of results [7,8].
Subsequently, navigable/steerable radiofrequency coblation devices were developed and used. These include the Yesdisc® and L’Disq®[9,10]. Data from studies of these devices were published from 2011 onwards. These devices are able to be steered directly to the actual herniated portion of the disc prolapse, usually at the posterior lateral aspect of the disc.
The purpose of this review is to assess the evolution of the various percutaneous disc RF devices, and assess the efficacy of the newer navigable coblation devices. The author’s personal experience with these devices is also presented.
Methods
This study involves the analysis of relevant Pubmed and Medline published articles on percutaneous lumbar disc intervention for disc herniation, and discogenic pain. Relevant studies on lumbar disc plasma coblation devices and treatment were reviewed. The primary outcome measures for success was improvement in Visual Analogue Scores(VAS) by 50% at 6 months or more post-procedure. Secondary outcome measures such as the Owestry Disability Index(ODI) were also reviewed. In addition, the author’s personal experience with nucleoplasty is also described. By this, the author seeks to determine if the newer percutaneous lumbar disc RF devices can be considered a good treatment option.
Study Results and Discussion
For large prolapsed/extruded discs with neural compression, many studies have shown the best treatment option would be the standard lumbar microdiscectomy [14]. A less invasive option would be lumbar epidural steroid injections, but this usually brings about only short term relief. As such, various percutaneous RF disc intervention techniques have been developed to address the sources of lower back pain. There are 2 main pain generators in the lumbar disc to be addressed and targeted. Firstly, the posterior annulus Type C pain fibres(which are small and unmyelinated), which are the discogenic source of pain. These nerves arise from the sinuvertebral nerves, and originate from of the ventral rami of the spinal nerves. The second pain generator is the herniated nucleus pulposus, usually posterior lateral in location causing spinal nerve compression sciatica.
It is important to note that these treatment modalities will not be able to address a large extruded disc or disc fragment causing nerve root compression. For large disc herniations causing neural compression and neurological weakness, lumbar microsurgery is the treatment of choice for long term relief of the patient’s symptoms [11,12].
Percutaneous laser disc decompression(PLDD) nucleolysis of the intervertebral lumbar disc has been developed and studied [13]. It was first introduced in 1986 by Peter Ascher and Daniel Choy [14]. This technique uses a straight cannula to target the central disc nucleus, with a variety of laser energy technology types used(eg.Nd-YAG laser, Carbon dioxide laser). The laser energy is delivered via a laser fibre, and the heat at the tip of the probe evaporates the nucleus water. This creates a partial vacuum, reducing intradiscal pressure, and causes the disc bulge to recede inward partially. It also causes structural changes in the protein, with denaturation and subsequent renaturation [15]. In various studies, the success rate ranged from 60-70%. However, a significant reoperation rate was found, as high as 38% [16]. This was also found in a Cochrane review of multiple studies by Gibson et al in 2000 [17]. In this study, laser discectomy was found not to be have a high rate of efficacy, and also to have significant complications. Thermal injury to the vertebral end plates is a concern, thus in patients with a significant loss of disc height, this procedure should not be used.
In these devices, the laser emitting probe cannot be steered to the actual area of disc herniation. It aims to decompress the central disc nucleus, with a view that the posterior-lateral disc bulge will decrease in size over time. Other large scale review studies also suggested more trials were needed to confirm the efficacy of laser disc decompression [18,19].
Intradiscal electrothermal(IDET) treatment has also been introduced from the late 1990s onwards, with mixed results found [5]. This treatment modality involves introducing the IDET heating catheter close to the region of the annular tear in the disc annulus. The IDET wire is first passed across the posterior annulus, and then uses conductive heating to heat the annulus, up to 90 degrees Celsius. The aim would be to ablate the pathological nociceptor nerves and also modify the collagen fibres of the annulus region of the disc. This may potentially seal the annulus fissure [34]. In a study from 2009-2014 on 120 patients, IDET was used for lower back pain treatment [20]. The study duration was for a full 12 months, and there was a modest average improvement in VAS of 57.39%. There have also been adverse outcomes reported such as thermal induced necrosis of the adjacent vertebral bone[21]. There has also been a report of development of a Grade I anteriolisthesis, and catheter shearing post-procedure [22,23]. This procedure can also be technically challenging, and occasionally causes charring around the wire which can limit the lesion size[5]. The use of IDET devices has currently reduced.
There have been a few unilateral approach RF thermal treatment devices developed. The older devices include SpineCATH® and DiscTRODE®. These have been used in various clinical trial with promising early results [5,24] These devices produce RF energy which is delivered to the tissue surrounding the RF probe wire tip. Ionic movements in this tissue generates heat which results in the annulus nerve fibre denervation. However, in a randomised controlled trial in 2009 using the DiscTRODE device, involving 20 patients who were followed up to 1 year, there was no significant improvement in patients outcome measures(VAS pain scores and ODI scores) [25]. These 2 devices are not being widely used currently.
A newer such device is the Flextrode®(Boston Scientific). It has a slightly curved tip, and aims to target the ipsilateral area of the posterior annular disc tear. The radiofrequency energy delivered is able to heal the tear and also denervate the posterior annulus pain fibres. This energy is delivered for 4 minutes duration, up to 80 degrees Celsius. Further studies are being awaited to show its long term results.
Biacuplasty®(Baylis Medical) has been developed to treat discogenic pain. This is also known as cooled RF, in that water is used to cool the distal probe tips. The procedure involves the insertion of two RF needles bilaterally into the disc to apply heat to the posterior annulus, to generate a wide bipolar lesion in the disc [5]. The aim of this treatment would be to treat discogenic pain, and the target would be the sensory nociceptor nerves at the posterior aspect of the annulus fibrosus of the disc. A randomised trial comparing this modality of treatment versus conventional medical management was carried out and published in 2017. This involved a total of 63 patients. In the Biacuplasty intervention group, improvement in VAS was modest at 55% at 12 months post-intervention. There was also a significant 64% improvement in the ODI at 12 months [26]. As the complication rate was also found to be low, this treatment modality can be offered to patients.
Intervention devices to target and reduce the size of the nucleus herniation were developed next. A large number of studies have been carried out on the Arthrocare Wand®(Sunnyvale CA). This is a Straight Cannula plasma coblation device, and has been in use since 1999. It functions by applying radiofrequency energy to the conductive nucleus medium. This would form a plasma field around the charged electrodes of the RF wand. The ionised particles created are able to break down the disc nucleus pulposus contents, by disrupting their molecular bonds [6,14]. This would aim to decrease the central intradiscal pressure, to allow the prolapsed disc fragment to implode inwards [7,8].
The initial studies showed promising results in the treatment of contained lumbar disc herniations [14]. In a prospective study on 47 patients, improvement in the VAS Scores(more than 50%) were good at 1 month(83% of patients), but this dropped to only 53% at 12 months. Improvement in ODI scores were also noted. Functional outcome improvements(Sitting, standing, walking) were also seen at 1 year post-procedure. There were no complications such as discitis, or neural damage reported [27].
A prospective study has also been done to evaluate the efficacy of nucleoplasty. This study involved 30 patients with back pain who underwent nucleoplasty. The follow-up period was up to 12 months. The reduction in VAS score at 6 months was modest at 53.30%, and 60% at 12months [28]. The main disadvantage of the device is it is not able to reach the actual area of disc herniation. It creates multiple central disc channels, vaporising disc nucleus material, with resultant central disc decompression. It thus relies on the central nucleus decompression for the relief of nerve compression sciatica symptoms [9].
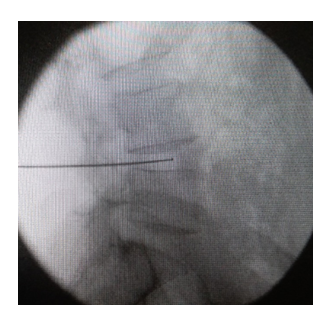
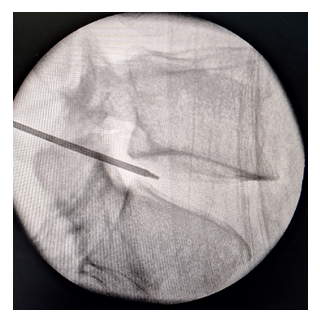
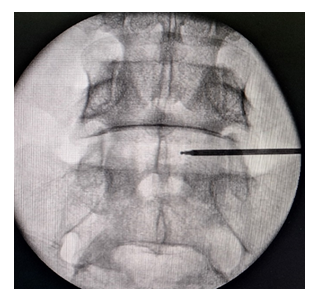
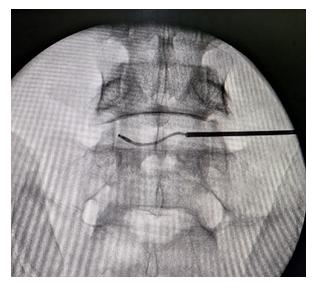
The development of percutaneous lumbar disc nuclear decompression devices continued with newer navigable devices. In 2011, a new study by Prof Lee Sang Heon was published on a navigable coblation device, the L’Disq Wand(U and I Co.Uijeongbu Korea) [9]. This device had a RF Coblation bipolar tip to generate the plasma field. The guide cannula is inserted obliquely from the opposite side(contralateral) of the prolapsed lumbar disc. After insertion, the probe tip can then be curved and steered using a control wheel, so as to direct it into the posterior-lateral herniated portion of the disc. It also can be directed superiorly or inferiorly. On activation, a coblation plasma field is generated which is able to vaporise the herniated nucleus material. This reduces pressure on the compressed spinal nerve root. This study involved 27 patients, and at 6 months post-procedure, the success rate was good. In 88% of patients, the VAS score decreased by 50% or more. The ODI also had reduced significantly. There were no major complications post-procedure. Two patients(7.4%) developed recurrent disc herniations, and required microdiscectomy surgery. This first study had a relatively short follow-up, but showed promising results.
A follow-up larger, longer term study in 2018, also showed similar good outcomes[29]. This involved 170 patients over 2 years. After 2 years, the mean VAS had decreased from 7.1 to 2.1. A total of 78.3% of patients had greater than 50% improvement in VAS. The mean ODI decreased from 50.9 to 20.3. The majority of patients had good improvement in pain outcomes. However, there were 3 cases of foot-drop(1.8%), but only 1 patient’s weakness lasted more than 6 months. The other two patients improved to normal power. The etiology of the neural damage was possibly due to proximity of the spinal nerve to the RF probe tip, with thermal effects occurring. As a standard pre-RF lesioning protocol, motor stimulation is always performed with monitoring for any foot twitches. This confirms the probe is not too close to the spinal nerve root. This is in addition to careful fluoroscopic confirmation of good RF probe tip placement. As with other lumbar spine intervention procedures, informed consent should be obtained from the patient, after discussing the indications and possible risks of the procedure.
A study published in 2012 with the senior author being Prof Kim Yong-Chul[30], involved a second navigable RF Coblation device(Yesdisc® Mcarekorea, Seongnam-Si, Korea). The aim of this study was to study the efficacy of this nucleoplasty device, and the relief of discogenic back pain. Discogenic back pain is commonly caused by annular tears in the posterior part of the disc. This can be diagnosed clinically, and can also be seen on MRI spine imaging as a hyperintensity zone [31].
This study involved 80 patients, and the overall results and outcomes were good. Fifty-six patients(70%)had more than 50% reduction in VAS scores at 6 months. There were no procedural complications. Aside from decompressing the nucleus, and the denervation of the annulus pain fibres, nucleoplasty can possibly also reduce the release of inflammatory mediators eg.phospholipase A2 [32]. More research on the full effects of plasma coblation nucleoplasty is still being carried out.
A subsequent study in 2024 by Yoo Yong-Jae et al [33] showed promising results also. This studied the relief of lumbar discogenic pain with the Yesdisc® navigable RF device. Comparison was made with patients undergoing the IDET thermal ablation procedure. Traditionally, lumbar discogenic pain is a difficult medical condition to relieve. The procedural aim was to ablate the pathological sinuvertebral nerves at the annular tear region [33]. The study involved a total of 142 patients. In the IDET group, there were 53 patients and the rate of pain relief was slightly lower(ranging from 56%-61%). In the Yesdisc group, there were 89 patients, with 61(68.5%) patients experiencing successful pain relief(more than 50% reduction in VAS at 6 months duration). These results are promising as discogenic back pain treatment results are traditionally modest[20]. The steerable nature of the newer navigable RF device possibly enables easier targeting of the posterior annular tear regions.
The author(RT) reviewed his own personal experience with 2 Plasma Coblation Devices. The indications used were for lumbar disc herniations causing predominantly sciatica type pain. The patients had completed a course of medical analgesic treatment, and a physiotherapy program. Patients who were still symptomatic were offered lumbar disc coblation intervention. Patients undergoing nucleoplasty with the straight cannula Arthrocare® wand previously were compared to more recent patients undergoing treatment with the Yesdisc® navigable probe. There were 20 patients in the straight cannula nucleoplasty device group, versus 44 patients in the Navigable Yesdisc probe group(a total of 64 patients). The patients underwent treatment for predominantly sciatica pain, and not pure axial back pain. The results of the VAS pain scores were assessed at 6 months post-procedure. A successful outcome was a reduction in the VAS pain score by 50%.
In the straight cannula wand group, results were encouraging, with 14 patients(70%) having improvement in VAS results(p<0.05). However, there was 1 patient who required a lumbar microdiscectomy, and 1 case of transient leg numbness. The cause of this could be too close a proximity of the probe to the spinal nerve root. The patient’s numbness resolved gradually over 3 months.
In the navigable coblation probe group(Yesdisc®Mcarekorea), the results showed improved effectiveness. There were a total of 44 patients, with a total of 61 disc levels treated(some patients had multi-level disc herniations to be treated). There was significant VAS improvement in 38 out of the 44 patients(86%)(p<0.05). None of the patients in this group required lumbar spine microdiscectomy surgery, and there were no complications such as discitis, or nerve root injury. This series of the author shows promising results with this newer device, but larger studies are needed in the future for further comparison.
Study Limitations
This study has several limitations. Firstly some of the evidence gathered comes from retrospective and non-randomised trials. This can result in non-definitive data gathered. Different procedural RF protocols were sometimes used by spine interventionalists, and hence comparisons in study results can be challenging.
Conclusion
In our review study, percutaneous intradiscal interventional procedures have an important role in the treatment of lower back pain. They are also a useful treatment modality if the patient declines the lumbar surgical option. Both pain due to disc herniations causing sciatica and axial discogenic pain can be addressed. A variety of percutaneous interventions such as radiofrequency annuloplasty devices, have been studied to treat discogenic pain, and these have shown promise. These can decrease the need for lumbar spine surgery such as spinal instrumented fusion. Navigable plasma coblation devices such as the Yesdisc® are able to be directed to the actual posterior-lateral herniated portion of the disc. This enables the spine interventionalist to directly target the actual disc pathology, reducing the actual compression of the nerve root. They are also able to perform denervation of the annulus fibrosus sensory pain fibres. Promising improvement in pain VAS results have been shown, ranging from 70% to 88%, with low procedural risks. These results are also reflected in the author’s(RT) experience using the devices in 61 procedures.
These interventions should be used only if the patient has completed a trial of medical conservative treatment, including spine physiotherapy. When performed for the correctly selected indications, good results can be achieved, with early return to activities of daily living. Further improvements in RF medical product technology can be expected, and larger scale trials will also help to elucidate these.
Acknowledgements
The author would like to thank Professor Lee Sang-Heon, Professor Kim Yong-Chul, and Mr Henry Kwee for guidance and assistance in this article.
Conflict of Interest
The author declares no potential conflict of interests with respect to the research, authorship and/or publication of this article.
References
- Bressler HB, Keyes WJ, Rochon PA, et al. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine 24 (1999): 1813-1819.
- Guo HR, Tanaka S, Halperin WE, et al. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health 89 (1999): 1029-1035.
- Walker BF, Muller R, Grant WD. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health 15 (2003): 79-87.
- Andersson GB, Brown MD, Dvorak J, et al. Consensus Summary of the diagnosis and treatment of lumbar disc herniation. Spine 21(1996): 75S-8S.
- Helm LS, Simopoulos TT, Stojanovic M, et al. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician 20 (2017): 447-470.
- Chen YC, Lee SH, Saenz Y, et al. Histologic findings of disc, end plate and neural elements after coblation of nucleus pulposus: An experimental nucleoplasty study. Spine J 3 (2003): 466-470.
- Delamarter RB, Howard MW, Goldstein T, et al. Percutaneous lumbar discectomy. Perioperative and post-operative magnetic resonance imaging. J Bone Joint Surg Am 77 (1995): 578-584.
- Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine 28(2003):661-5.
- Lee SH, Derby R, Sul DG et al. Efficacy of a new navigable percutaneous decompression device(L’Disq) in patients with herniated nucleus pulposus related to radicular pain. Pain Medicine 12 (2011): 370-376.
- Yoo YJ, Song HG, Park SY, et al. Percutaneous Lumbar Nucleoplasty in the management of lumbar discogenic pain. International Journal of Pain 9 (2018): 15-25.
- Blamoutier A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. 99 (1 Suppl.) (2013): S187-S196.
- Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine 7 (1982): 604-607.
- Nerubay J, Caspi I, Levinkopf M, et al. Percutaneous laser nucleolysis of the intervertebral lumbar disc. An experimental study. Clin Orthop Relat Res 337 (1997): 42-44
- Singh V, Derby R. Percutaneous lumbar disc decompression. Pain Physician 9 (2006): 139-146.
- Schenk B, Brouwer PA, Peul WC, et al. Percutaneous laser disk decompression: A review of the literature. AJNR Jan 27 (2006): 232-235.
- Epstein N E. Should anyone perform percutaneous endoscopic laser diskectomy and percutaneous lumbar disc decompressions? Surg Neurol Int 26-27 (Suppl 42) (2016): S1080-S1084.
- Gibson JN, Grant IC, Waddell G. Surgery for lumbar disc prolapse. Cochrane database Syst Rev 3 (2000): CD001350
- Goupille P,Mulleman D, Mammou S, Griffoul I, et al. Percutaneous laser decompression for the treatment of lumbar disc herniation: a review. Semin Arthritis Rheum 37 (2007): 20-30.
- Rados I, Katusin ML, Budrovac D, et al. Percutaneous laser disc decompression for lumbar radicular pain: A systematic review of Pubmed in the last 5 years. Acta Clin Croat 62 (Suppl4) (2023): 63-67.
- Kircelli A, Coven I, Cansever T, et al. Patient selection and efficacy of intradiscal electrothermal therapy with respect to the dallas discogram score. Turk Neurosurg 27 (2017): 623-630.
- Kim S, Lee SH, Kim ES, et al. Thermal-induced osteonecrosis of adjacent vertebrae after intradiscal electrothermal therapy. J Korean Neurosurg Soc. 60 (2017): 114-117.
- Davis TT, Delamarter RB, Sra P, et al. The IDET procedure for chronic discogenic low back pain. Spine (Phila Pa 1976) 29 (2004): 752-756.
- Orr RD, Thomas SA, Intradural migration of broken IDET catheter causing a radiculopathy. J Spinal Disord 18 (2005): 185-187.
- Finch PM, Price LM, Drummond PD. Radiofrequency heating of painful annular disruptions: One year outcomes. J Spinal Disord Tech. Feb 18 (2005): 6-13.
- Kvarstein G, Mawe L, Indahl, A et al. A randomised double-blind controlled trial of intra-annular RF thermal disc therapy-a 12 month follow-up. Pain Oct 145 (2009): 279-286.
- Desai MJ, Kapural L, Petersohn JD, et al. A prospective multi-centre, open label clinical trial comparing intradiscal biacuplasty to conventional medical management for discogenic lumbar back pain. Spine (Phil Pa 1976) 41 (2016): 1069-1074.
- Singh V, Piryani C, Liao K, et al. Role of percutaneous disc decompression using coblation in managing chronic discogenic low back pain: A prospective observational study. Pain Physician. 7 (2004): 419-425.
- Kumar NS, Siddharth SM, Tan WLB, et al. Discogenic axial back pain: Is there a role for nucleoplasty? Asian Spine Journal 7 (2013): 314-321.
- Kim NH, Hong Y, Lee SH. Two year clinical outcomes of radiofrequency focal ablation using a navigable plasma disc decompression device in patients with lumbar disc herniation: efficacy and complications. J Pain Res 11 (2018): 2229-2237.
- Yoo YJ, Song HG, Park SY, et al. Percutaneous Lumbar Nucleoplasty in the management of lumbar discogenic pain. International Journal of Pain 9 (2018): 15-25.
- April C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol 65 (1992): 361-369.
- Ren D, Zhang Z, Sun T, et al. Effects of percutaneous nucleoplasty with coblation on phospholipase A2 activity in the intervertebral disks of animal model of intervertebral disc degeneration: a randomised controlled trial. J Orthop Surg Res 10 (2015): 38.
- Yoo YJ, Bae JG, Kim H, et al. Percutaneous nucleoplasty and intradiscal electrothermal therapy in the management of lumbar discogenic pain. Medicine 103 (2024): 1-8.
- Park H, Kim N. Intradiscal procedures in chronic spinal pain. Int J Pain 13 (2022): 55-70.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 