Role of Non-Rigid Minimal Intervention Surgery in the Treatment of Degenerative Spondylolisthesis
Bañuls-Pattarelli Miguel1*, García-Ortiz María Tíscar1, Atienza-Vicente Carlos2, 3, López-Prats Fernando1, 4, Mulholland Robert C5
1Department of Orthopaedics and Trauma, Elche University General Hospital, Elche (Alicante), Spain
2Associated Professor of Mechanical and Materials Engineering, Master of Biomedical Engineering, Polytechnic University of Valencia, Valencia, Spain
3Biomechanics Institute of Valencia, Health Technology Group, Polytechnic University of Valencia, Valencia, Spain
4Department of Orthopaedics and Trauma, Miguel-Hernández University, San Juan de Alicante, Spain
5Nottingham University Hospitals NHS, Nottingham, United Kingdom
*Corresponding Author: Bañuls-Pattarelli Miguel, Department of Orthopaedics and Trauma, Elche University General Hospital, Carrer Almazara 11, 03203, Elche (Alicante), Spain
Received: 19 July 2021; Accepted: 27 July 2021; Published: 04 August 2021
Article Information
Citation:
Bañuls-Pattarelli Miguel, García-Ortiz María Tíscar, Atienza-Vicente Carlos, López-Prats Fernando, Mulholland Robert C. Role of Non-Rigid Minimal Intervention Surgery in the treatment of Degenerative Spondylolisthesis. Journal of Spine Research and Surgery 3 (2021): 071-080.
View / Download Pdf Share at FacebookAbstract
Introduction: Degenerative spondylolisthesis produces abnormal intervertebral movement associated with back pain. Standard surgical treatment consists of decompression with or without fusion. There is no consensus about the method of choice.
Purpose of this study: avoiding decompression, a semi-rigid, minimally invasive device that reduces movement was used, removing the necessity for fusion and reducing fixation-loosening, or breakage.
Methods: Analytical prospective observational study. The clinical assessment included the Oswestry Disability Index (ODI) and SF-12 (Short Form-12 Health Survey), X-Rays and MRIs (Magnetic Resonance Imaging) were taken preoperatively and at follow-up. Overall, the mean postoperative follow-up was 3.8 years. It is about a posterior intrapedicular device introduced percutaneously under X-Ray control. The device consists of two semi-rigid bars, allowing 5º multiplanar movement, and 1mm compressive-spring movement. Through manipulation and distraction, reduction of listhesis is possible, increasing disc and lateral recesses height.
Results: At final follow-up, ODI and SF-12 scores significantly improved. ODI from 47.4 ± 14.9 to 22.8 ± 19.7 (p<0.001). In terms of SF-12, PHS (Physical Health Score) improved from 27.9 ± 6.3 to 37.5 ± 11.1 (p<0.001) and MHS (Mental Health Score) from 34.4 Keywords
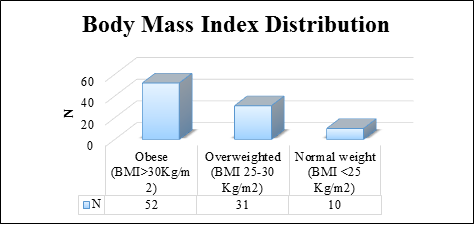
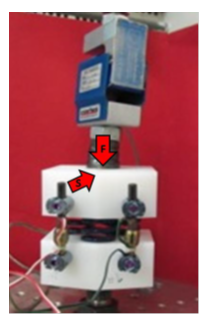
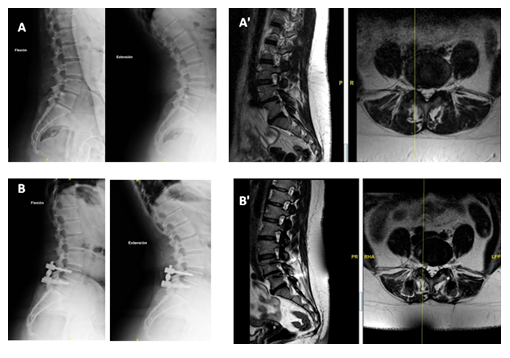
<p>Minimal Invasive Surgery, Degenerative Spondylolisthesis, Percutaneous Posterior Transpedicular Fixation, Non-Rigid Dynamic Stabilisation</p> Degenerative spondylolisthesis is commoner in middle age women, mostly at L4-L5. This is due to failure of the disc that increases loads to the facets that generates cartilage changes and facet subluxation [1]. The cause is probably multifactorial, but weakness of the abdominal muscles, related to pregnancy and obesity may explain the female preponderance [2]. The anatomical distortion may produce pain due to spinal stenosis, and abnormal movement of the disordered facet joints. In severely affected patients surgical treatment is appropriate. Posterior decompression with laminectomy and undercutting of the facet joints is an established technique [3]. Whether spinal fusion should be done at the same time as decompression is still debated [4]. In the past it was established the role of fusion when decompressing a patient with spinal stenosis due to spondylolisthesis improved the results significantly [5]. At present whether instrumentation is of value to improve the chances of a solid fusion is uncertain [6]. Modern tendencies suggest fusion is recommended [7]. Anterior fusion with reduction is now an established technique, now including many minimally invasive procedures of various interbody fusions [8]. However, the morbidity associated with the interbody fusions should be considered [9]. A recent paper [10] shows that extreme lateral interbody fusion (XLIF) is effective in decompressing the neural elements, independently of the degree of decompression. It is likely that stopping movement, by reducing the inflammatory change around the disorganized joints is of equal importance. It was clear from the literature that stopping movement was an important factor in the relief of symptoms, and with various percutaneous techniques this could be achieved, with indirect reduction. The unknown factor was that a rigid fixation would in time loosen if unaccompanied by a fusion. Loosening of fixation is related to the load that the fixation has to take. If the fixation was so designed that it took no load, but at the same time stopped painful movement, then it might be secure in the long term. The authors identified a device, Dynabolt® part of a Silverbolt® System (Vertiflex, Exactech, ChoiceSpine), which could be inserted percutaneously, it allowed a very restricted range of movement. However, biomechanical testing confirmed that most of the load was transferred to the disc. With the advent of Minimal Intervention Surgery (MIS), clearly it may be possible to stop movement and decompress [11]. Using these technique, the present study develops this concept. It involves doing a dynamic pedicle fixation introduced percutaneously [12]. This analytical observational study has a prospective design and it has been approved by the institutional review board. Informed consent was required from every patient prior to operation. The data protection law it is properly followed. The sampling is consecutive, not probabilistic, which consists of selecting the individuals who meet the selection criteria, as they come to the consultation in the given period. From August 2015 until May 2019, 93 patients were operated of lumbar degenerative spondylolisthesis at the single affected level (Table 1) using a minimally invasive non-rigid percutaneous posterior intrapedicular system. Level L3-L4 was addressed in 7 cases (7.5%), L4-L5 in 80 patients (86%) and finally L5-S1 in 6 cases (6,5%). The system is comprised of cannulated standard polyaxial pedicular screws and a semi-rigid bar. It consists of 4 self-tapping polyaxial cannulated screws united by 5mm diameter rods. Each rod allows 5º angular movement in all planes and 1mm of compression (Figure 1). Preoperatively and postoperatively ODI and SF-12 tests were done together with dynamic flexion-extension X-rays and MRI annually. Post-operative length of stay and operative time was recorded. Body mass index (BMI) was recorded preoperatively (Figure 2). 2.1 Evaluations Follow-up was performed annually after the operation (range 2-5 years). On each revision the ODI and SF-12, and flexion-extension dynamic X-rays and MRI were performed. Radiographs at the final follow-up were evaluated by 2 independent observers who were blinded to clinical outcomes. We made the follow-up of 93 patients. Sixty-five were women (69,9%) and twenty-eight (30,1%) men. Mean age was 63.8 years (range, 26-79). Using the Meyerding criteria [13], 75 (80.6%) were grade I and 18 (19.3%) grade II spondylolisthesis. 2.2 Biomechanics The biomechanical characteristics of the non-rigid system was tested against its rigid version. The implants were mechanically tested by means of a validated method using artificial discs and polyethylene blocks resembling vertebral bodies. Both simulate the lumbar spine (ISO 12189:2008). Axial and anteroposterior tests were performed applying forces in the axial and antero-posterior direction resembling the human body transmission of forces (Figure 3). The analysis of the resistance curve shows that the non-rigid system fails at 320N against 420N for the rigid. Both, rigid and non-rigid systems need antero-posterior forces above the 300N mark to produce displacements of more than 1mm. Those forces are within the normal applied anteroposterior load of the human spine [14-17]. The performed biomechanical tests suggest that the non-rigid system does not control loading but acts like a garden stake, controlling antero-posterior gliding movement, this is avoiding lysthesic movement in the sagittal plane. 2.3 Surgical technique The surgeries were performed by experienced spine surgeons; the procedures were standardized in our department performed under general anaesthesia in prone position. Prophylaxis with 2g of cefazolin was given preoperatively to all patients (except allergies). Through four 1.5mm incisions and under X-ray control a Jamshidi type cannula is introduced into the pedicles. Guide wires are placed through the cannulas. The screws placed in assembly towers are then introduced following the guide wires. Once the screws are in place the non-rigid bars are deployed by means of an introductory tool which allows the bar to be guided vertically first, and then lowered to reach the next screw (Figure 4). Through manipulation of the assembly towers, it is possible to reduce the lysthesis and then fix it in place with distraction of the elements. Affected level N L3-L4 7 (7.5%) L4-L5 80 (86%) L5-S1 6 (6,5%) Table 1: Lumbar segments affected. Figure 1: Each rod allows 5º angular movement in all planes and 1mm of compression. Figure 2: Graphic diagram showing BMI distribution. Figure 3: Flexo-compression test configuration and load applied. Figure 4: Introductory tool which allows the bar to be guided vertically first, and then lowered to reach the next screw. 2.4 Statistical analysis The descriptive analysis of the data is presented as mean ± standard deviation (sd) and the proportions as percentages. With the Kolmogorov-Smirnov test, it is verified whether the variables have a normal distribution. With the Student's T test, the differences between the continuous variables for related samples were analysed. All statistical evaluations were bilateral and values ??with p <0.05 were considered statistically significant To perform the statistical analysis, Statistical Package for the Social Science (SPSS v22.0) was used. After applying inclusion and exclusion criteria, 93 patients were included. Minimum follow up was two years (range 2-5). The mean duration of the surgical intervention is 65.1 ± 18.3 minutes, (range 30-120 minutes). Finally, the mean stay was 1.7 ± 0.9 days, with the median being 2 days and the mode being 1 day of hospitalization. No patient was hospitalized for more than a week. 3.1 Clinical evaluation Clinical scores significantly improved. ODI diminished from 47.4 ± 14.9 to 22.8 ± 19.7 at the final follow-up (p<0.001). In terms of SF-12, PHS (Physical Health Score) improved from 27.9 ± 6.3 to 37.5 ± 11.1 (p<0.001) and MHS (Mental Health Score) from 34,4 ± 11,3 to 42,7 ± 13,2 (p<0.002) (Table 2). Revision surgery was not required in any case. Post-surgical complications rate was really low, we only had one postoperatively hematoma solved conservatively, and one mal position of a screw inside the lumbar canal, causing no symptoms in that lady. 3.2 Radiological assessment In flexion-extension x-rays no instability was observed, meaning that in the normal anteroposterior movements the system acts like a rigid fixation one. We observed either complete reduction of the lysthesis 62 %, or improvement of the degree of lysthesic displacement 31%, together with increase height of the discal space because of the locking of the device in distraction when introduced. In addition, the influence of age divided in two groups (under 65, working people, and over 65 years, retired people), sex, level of intervention (L3-L4, L4-L5, L5-S1) and diagnosis (Lysthesis I or II) was assessed with the results of ODI, and SF-12 obtained without finding statistically significant differences between them (p> 0.05). Preop ODI Postop ODI p-value 47.4 ± 14.9 22.8 ± 19.7 <0.001 Preop SF-12 (PHS) Postop SF-12 (PHS) 27.9 ± 6.3 37.5 ± 11.1 <0.001 Preop SF-12 (MHS) 1 year SF-12 (MHS) 34.4 ± 11.3 42.7 ± 13.2 <0.002 Table 2: Oswestry Disability Index (ODI) and SF-12 results (mean ± standard deviation). Degenerative spondylolisthesis is due to changes in the facet joints so that the upper vertebrae progressively moves ventrally on the pedicle towards the vertebral body. This explains two important features, firstly the slip can never be more than about 30%, as the joint would reach the back of the body and secondly the root emerging below the level of the spondylolisthesis is compressed by the superior facet of the lower vertebrae, not by the facet joint of the upper vertebrae. Hence an L4-L5 degenerative spondylolisthesis compresses the 4th root however, the 5th root (traversing) can also be compressed by flavum and exuberant capsule of L4-L5 [18]. The altered anatomy produces spinal stenosis, presenting clinically as back and root pain. Described classically by Herkowitz et al [19, 20], they established that decompression alone was successful in 60% of patients, but an added uninstrumented fusion improved the results to some 90%. Instrumentation did not affect the initial results, but a subsequent paper from that department demonstrated that the addition of instrumentation had benefit in the long term. However, a recent paper by Abdu et al [21, 22] demonstrated that the method of fusion, even anterior fusion showed no differences. It is the case therefore that direct decompression alone, involving partial or total laminectomy and undercutting facetectomy [3] although successful is not the only method of achieving a satisfactory result. The current tendency is that decompression alone is not recommended, and instrumented fusion is the standard [7]. The authors accept that a contributing cause of pain in spondylolisthesis is due to multiple factors (osteoporosis, multilevel involvement and sagittal balance specially at the L5-S1 level in lytic and istmic spondylolisthesis). The literature [19, 20] established that stopping movement that is fusion and neural decompression were key procedures in this disorder. The problem is that those procedures do also denervate the joints, remove most of the ligamentous tissues, and synovium, all potential pain sources [23]. An anterior fusion removes the disc, again a potential source of pain. On those bases we cannot with absolute certainty conclude that stopping movement and decompression are the main reasons for alleviation of pain. This minimal intervention procedure could be regarded as an experiment to see if just stopping movement and indirectly decompressing without major tissue damage are the reasons for the relief of symptoms. Those were the reasons why dynamic x-rays and MRI were taken and demonstrated that abnormal movement present before was not present after fixation. In summary we believe the literature establishes that in this disorder, stopping movement and indirect decompression is an acceptable form of treatment. Our case is that this is achieved by this procedure. In our series we have compared in each patient pre- and post-operative MRI scans and established that on visual examination reduction does increase space for the neural tissue (Figure 5). We believe that is well established that reduction increases spinal diameters and decompresses, the neural elements. Indeed, it is the whole basis of anterior fusion and indirect decompression. Clearly indirect decompression, achieved by an anterior fusion will reduce the spondylolisthesis, but will not decompress the root lying below the superior facet joint of the lower vertebrae. Yet it does cure L4 root pain. The likely reason for this is revealed if we study the pre- and post-operative MRI scans. In the pre-operatively scans it is clear that around the facet joint is exuberant inflammatory tissue related to the moving degenerate joints. The exuberant tissue, of capsule and synovium is an important factor in compressing the nerve. Post-operatively on the MRI scan this tissue is gone (Figure 5). The reduction contributes to increase diameters as the redundant capsule is pulled back, but the diminished space for the nerve beneath the superior facet of the lower vertebrae remain. This suggests that it was the movement of the degenerate joint that produced the exuberant tissue and stopping movement caused it to regress. These considerations are of relevance to the success of this minimal intervention technique. The lamina of the upper vertebrae is reduced solving the central canal stenosis and any L5 root compression but, by the stopping of movement reduces the irritation on the root, by inflammatory synovium and capsule although it still remains entrapped below the superior facet of the lower vertebrae. Our results are comparable to anterior fusion [24, 25] as the one described by Takahashi [9], 76% of satisfaction. Similar to the ones described by Oliveira et al [10] 86.5% by XLIF. In summary the results in those 93 patients demonstrated that in 79 of the patients stopping movement, and indirectly reducing compression, both confirmed by dynamic x-rays and MRI scans at review stopped both their back pain and claudication. Because of the nature of the intervention, we can be confident that no other access related factors could explain this. In the present study, the pain was related either to the stenosis, or the facet degeneration not to an abnormal loading pattern. Adequate reduction of the spondylolisthesis is important to ensure decompression of the neural elements. This is a device that is only appropriate when the pain is related to stenosis or clearly facet degeneration as is seen in degenerative spondylolisthesis. Although implant failures have been reported in recent papers [26, 27] we did not record implant failure in our series, not in the dynamic rod and only one screw breakage with no clinical significance in the patient. No adjacent segment degeneration was noticed in the present study. The authors believe that abnormal movement inflammation and stenosis in degenerative spondylolisthesis can be treated by a minimally invasive device without the need of decompression and fusion. We looked at the results of this series and it was clear that stopping movement, and reduction of the lysthesis even to some degree was of clinical benefit. Figure 5: A) Preoperative flexion-extension X-ray; A') MRI; B) postoperative flexion-extension X-ray; B') postoperative MRI. Shows reduction of lysthesis and increase of diameters of central canal and recesses. We conclude that in this group of patients, that is elderly, mainly women who may have generalized lumbar degeneration, but who have spinal stenosis due to a degenerative spondylolisthesis, can be treated very effectively, with little likelihood of operative related complications. This appliance deals effectively with pain due to movement or stenosis, but will not deal with pain due to abnormal loading, as it does not unload the disc. Hence this series does not validate its use more generally for back pain considered to be due to abnormal loading. The authors conclude that the non-rigid system is a good option for the treatment of demonstrated mobile single segment degenerative spondylolisthesis. There is minimal access related injury, a short operating time, short stay in hospital and good recorded 3–4 years results. The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The author(s) received no financial support for the research, authorship, and/or publication of this article.Article Details
1. Introduction
2. Materials and Methods


3. Results
4. Discussion
5. Conclusion
Declaration of Conflicting Interests
Funding
References
Article Views: 1586
Journal Statistics




Discover More: Recent Articles


