Scientific Consideration of the Misinterpretations of Test Results During the Corona Pandemic
Lars Homagk
MVZ GmbH, Schillerstraße 14, 06667 Weißenfels, Germany
*Corresponding author: Lars Homagk, MVZ GmbH, Schillerstraße 14, 06667 Weißenfels, Germany.
Received: 16 November 2023; Accepted: 22 November 2023; Published: 06 December 2023
Article Information
Citation: Lars Homagk. Scientific Consideration of the Misinterpretations of Test Results During the Corona Pandemic. Journal of Women’s Health and Development 6 (2023): 102-107.
DOI: 10.26502/fjwhd.2644-288400112
View / Download Pdf Share at FacebookAbstract
SARS-CoV-2 in 2019 a coronavirus started circulating. Nevertheless, in 2021 there was a significant decrease in respiratory infections with a simultaneous significant increase in pandemic-related SARS-CoV-2 infections found. The end of the 2019/2020 influenza season was already registered in early summer 2020, and in the following season. There was an nearly complete absence of influenza. The further processing of this influenza gap showed multifactorial reasons also the lack of registration of influenza cases This study looks for further reaseons and from several perspectives in order to develop strategies for a representative recording of acute respiratory diseases (ARI). For Evaluation the data of GrippeWeb, the RKI’s Survstat® tool and the RKI’s reporting data on the new coronavirus were used. In addition, an evaluation of several billing numbers (32006, 32816, 32841) in the outpatient system from 2017 to 2022. Furthermore an evaluation of data on sick leave and illness statistics from 2019 to 2021. The data shows an average of 300,000 annual reports for ARI per year. In 2019 it increased to 1,985,985 reports, in 2020 (5,453,017) and in 2021 to 29,681,158. There is also a correlation between the SARS-CoV-2 test frequency and the positive results, as well as an increase in the previously 6% positive rate for SARS-CoV-2 to over 50% in 2022. At the same time decreases the medical burden due to acute respiratory diseases (ARI) contrary to the increase of the acute respiratory diseases reported. In contrast to influenza A/B, the other viral respiratory pathogens (adenovirus, parainfluenza virus and RS virus) do not show any significant reduction. From 2020, the number of reports of respiratory infections to the RKI increased from an average of 300,000 annual reports by 2019 to 1,985,985 reports in 2020, over 5,453,017 reports in 2021 and to 29,681,158 in 2022. On the other hand cases of incapacity to work due to respiratory infections fell from 31.0% in 2019 to 15.3% in 2021. The reduction in influenza A and B from 2020 as a result of the comprehensive Covid-19 control measures, including the obligation to wear masks, cannot be considered a major reason; rather, the aspect of underreporting of influenza cases plays a significant role. Therefore, the reporting quantity of the sentinal practices should be considered and the recording of incapacity diagnoses should be taken into account. Furthermore, an infection positive rate should not be used as a criterion for infection avoidance strategies and the recording of test results should always be validated and controlled. Only the testing of symptomatic persons should be remunerated and only these validated test results should be considered in the registration.
Keywords
<p>Influenza; Covid-19; SARS-CoV-2; RKI; GrippeWeb</p>
Article Details
Introduction
Seasonal influenza causes 3 to 5 million cases of illness and an estimated 290,000–650,000 deaths annually worldwide [1]. A meta-analysis published in 2018 comes to the conclusion that around 10% of unvaccinated adults become infected with influenza every year [2]. In Germany, the RKI has been using the GrippeWeb portal since 2011 to conduct an intensive and detailed scientific examination of influenza outbreaks, which plays a pioneering role in Europe [3]. In the 2017/18 season, for example, the estimate of influenza-related treatments were allmost 9 million. Most illnesses were caused by influenza B viruses. Influenza-related sick leave was estimated at 5.3 million this season and influenza-related hospitalizations at approximately 45,000 [4]. The premature end of the influenza season in 2019/2020 and the almost complete absence of the influenza season 2020/2021 was registered both in Germany and in Europe [5]. Expressed in numbers, 479 laboratory-confirmed influenza cases have been reported to the Robert Koch Institute (RKI) since week 40/2020. In the same period of 2019 of the 2019/20 flu season, 165 036 cases were reported. The ECDC also notes in Flu News for the 2020/2021 season that the positive rate of sentinel samples has fallen to 0.1% [6,7]. With SARS-CoV-2, a coronavirus start a circulation and the resulting disease - called Covid-19 - has been manifested since December 2019 as an accumulation of severe pneumonia, initially in Wuhan, China [8]. In 2021 in particular, there will be a decline in all respiratory infections with a significant increase in the number of SARS-CoV-2 infection reports caused by the pandemic, also based on an exorbitant increase in specific test procedures [9]. This study looks for further reaseons and from several perspectives in order to develop strategies for a representative recording of ARI and to show optimizations in the test strategy during pandemic times, to depict a realistic depiction of the infection situation and thus to improve civil protection.
Methods
The reporting data from the RKI on the novel coronavirus [9] were used and statistically evaluated for the evaluation. The data from GrippeWeb and the RKI's Survstat® tool [10] were used and statistically evaluated to evaluate the flu cases. In addition, a written request was sent to all 17 County associations of health insurance departments (KV) with the request for billing data to be transmitted for billing number from the years 2017 to 2022:
- [32006 ] Illnesses or suspected illnesses for which there is a legal obligation to report if microbiological tests are carried out, or cases of illness with reportable evidence of a pathogen
- [32841] Influenza A and B (not if bird flu is suspected)
- [32816] nucleic acid detection of the beta coronavirus SARS-CoV-2 using RT-PCR
The data analysis on incapacity for work was based on the results of the Federal Ministstry of Health, which breaks down the cases and days of incapacity for work according to diagnoses [11,12].
The collection and statistical evaluation of the data was carried out with SPSS Statistics 26 for Windows and was purely descriptive.
A vote by the ethics committee is not necessary, since no data protection-relevant and personal data was evaluated.
Results
The data initially show the expected billing frequency in the flu months around the 1st quarter of each year with a significant increase in the test frequency from the 2nd quarter of 2020 for the EBM fee items 32006 and 32841. At the same time, the positive reports are reduced to less than 100 cases, also from the 2nd th quarter of 2020 in GrippeWeb [10]. This data results in a positive rate for influenza A and B of up to a maximum of 23.38% in the first quarter of 2018 and an annual average of 4.26%. Furthermore, there is no correlation between the test frequency and the positive report (Fig. 1) the Pearson correlation coefficient is -0.14.
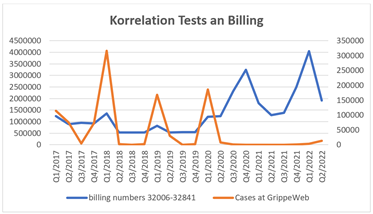
Figure 1: Representation of billing and flu case reports for 2017 to 2021 using the Survstat tool.
If one considers the other viral respiratory tract pathogens (adenovirus, parainfluenza and RS viruses) in addition to influenza A and B, there are no significant differences in the occurrence of adenovirus-related respiratory tract infections. Parainfluenza and RSV infections only show a significant reduction in 2022, but not in 2021, like influenza A/B (Figure 2).
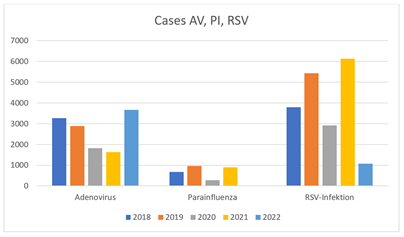
Figure 2: Representation of viral respiratory infections for 2017 to 2021 using the Survstat tool.
A clear change in the spread of viral respiratory infections can be seen from 2020. Not only did influenza A/B, which had previously been the most common ARI at over 90%, fell to 10% of the total in 2020 and tended towards zero from 2021. The number of respiratory infections, reported to the RKI exploded from an average of 300,000 annual reports by 2019 to 1,985,985 reports in 2020, over 5,453,017 reports in 2021 and by week 49/2022 to 29,681,158 per calendar year due to the spread of the novel SARS-CoV-2 [9,13].
Furthermore, in contrast to the known test results for respiratory infections in GrippeWeb [13], which have been collected for years, there is a significantly increased test frequency for the novel SAR-CoV-2. A consistently high distribution of the same over the entire observation period from 2020 to 2022 found that the Pearson correlation coefficient was 0.71, providing a correlation between testing frequency and a positive report that had not occurred in previous respiratory disease testing procedures (Figure 3).
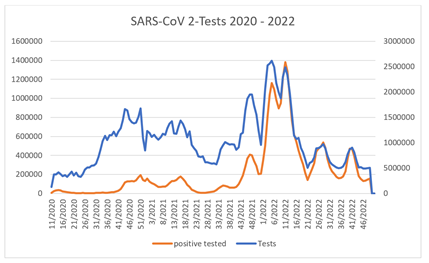
Figure 3: Test frequency and positive report for SARS-CoV-2 in the period from week 11/20 to 49/22.
While there is an average positive rate of 4.26% for influenza A and B over the calendar year, which increases in the flu waves and falls to 0% in the summer quarters, but is still independent of the test frequency, this is evident in the case of novel SARS-CoV -2 another picture. Not only do test frequency and test result correlate, there are also differences in the positive detection at the RKI depending on the Survstat evaluation module or the RKI's own data table. In addition, the reporting rate according to the RKI method exceeds the number of PCR samples billed many times over, especially from the fourth quarter of 2021. Also noticeable in the quarters mentioned above is the massive increase in the positive rate for SARS-CoV-2, which was previously 6%, to over 50% [9].
This significant decrease in the burden of illness among the German population is due in particular to the significant decline in "classic" respiratory diseases with an increase in the frequency of SARS-CoV-2 disease from 0% to 2.8% of all disease frequencies in 2020 and to 5.5 % in 2021. According to the results of the statistics of the Federal Ministry of Health for the years 2019 and 2020 for the ICD-Codes: J00, J01, J02, J03, J06, J09, J20, J32, J40, J98, B34, B99, the total number of sick leave days in 2019 was 73,281,305 and 75,106,232 in 2020. However, a massive increase in sick leave would have been expected from 2020 and especially 2021, since the frequency of respiratory infections reported to the RKI was around 2684 % increase (Fig. 4).
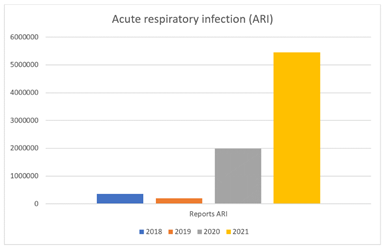
Figure 4: Positive reports to the RKI of respiratory infections 2019 – 2021.
Likewise, from the 1st quarter of 2020 with the introduction of the ICD codes for the novel SARS-CoV-2 (U07.1 COVID-19, virus detected, U07.2 COVID-19, virus not detected) show a significant increase in encryption due to the pandemic situation. However, there is a discrepancy with the data from the RKI. The test frequencies and positive tests according to the RKI resulting in an annual average positive rate of 5.4% for 2020 and 10.4% for 2021.
From 2019 to 2020 we see much fewer diseases of the respiratory system and for 2021 with a simultaneous increase of only 19.0% in cases of illness with "code numbers for special purposes", which the code numbers of the SARS-CoV-2 diseases U07 and Includes U99. These were not yet recorded by the Federal Ministry of Health in 2021. This clear net decline in cases of sick leave, especially in 2021, is also reflected in the evaluation of the health reports of the health insurance for the diagnoses of respiratory diseases among the 40 most common ICD-Codes: J00, J01, J02, J03, J06, J09, J20, J32, J40, J98, B34, B99, U07, U99 (Figure 3).
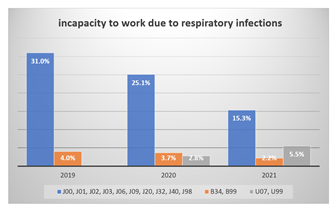
Figure 5: Frequency of incapacity to work due to respiratory infections 2019 - 2021
Discussion
The premature end of the 2019/2020 influenza season and the almost complete absence of the 2020/2021 influenza season was registered both in Germany and in Europe [6,14]. These studies show that COVID-19 containment measures and general behavioral changes in the population have likely had an impact on the transmission of other infections. The main containment measures implemented in Germany were contact restrictions and mobility restrictions, and from mid-March 2020 schools and restaurants were closed and most sports and leisure activities were banned. Travel was also restricted and social distancing measures were ordered and monitored. In addition, the mask requirement was introduced at the end of April 2020. The Covid-19 control measures also had a significant impact on the norovirus positivity rates. Norovirus is highly contagious, being transmitted via the fecal-oral route, through contaminated hands, or by consuming contaminated food or water [15]. Wu D et al. also explain the decline in chickenpox, herpes zoster, rubella and measles in China [16] and de Miguel et al. the decline in foodborne infections and sexually transmitted diseases in Spain [17]. A decline in all infectious diseases has been described for Switzerland for the same reasons [18]. However, influenza and corona viruses differ only marginally in their properties and size. The coronavirus is described as a membrane-enveloped RNA virus with a spherical to pleomorphic shape and a diameter of 60 to 140 nanometers (nm) [19]. Similarly, the influenza viruses are globular or spherically ellipsoid (round to ovoid), occasionally also filamentous, enveloped virus particles with a diameter of 80 to 120 nm [20]. These similar epidemiological profiles and the same physico-chemical properties are essential for the probability of transmission [21]. Influenza viruses, but also adeno, parainfluenza and RS viruses are mainly transmitted by droplets that have a particle size of more than 5 μm, especially when coughing or sneezing, and via airborne transmission by so-called droplet nuclei that are smaller than 5 μm. In addition, transmission is possible through direct contact of hands with surfaces contaminated with virus-containing secretions and subsequent hand-mouth/hand-nose contact [21]. This suggests that there can be no significant differences between corona viruses and the other viral pathogens of respiratory infections, neither in size nor in the way of contamination, so that the isolated influenza gap is not sufficiently explained by the Covid containment measures. This assumption is also supported by the fact that our analyzes did not show a significant decrease in infections with the adenovirus or RS virus in 2020 and 2021. For this reason, the comprehensive Covid-19 control measures, including the obligation to wear masks, cannot be used as a significant reason for the reduction in influenza A and B, which Jefferson et al. confirm [22]. Thus, the comprehensive Covid-19 control measures should have had a significant impact on reducing the spread of Covid-19, which has been largely refuted by studies and meta-analyses [23,24]. This assumption is supported by the fact that our analyzes did not show a significant decrease in infections with the adenovirus or RS virus in 2020 and 2021. Jefferson et al. confirm this with their meta-analysis on the efficiency of a mask requirement in endemic and pandemic respiratory infections, which does not exist [22].
The fact that corona viruses (HCoV) have been responsible for around 5-10% of acute respiratory infections (ARI) for decades is somewhat underexposed in public perception [25]. This probably led to an underestimation of the clinical and epidemiological impact of the endemic coronaviruses NL63, HKU1, OC43 and 229E. Biere et al. examined the endemic distribution of these four CoV types in 2019 and 2020 and showed that HKU1 was predominant and was present in 8% of all samples of this virus. The less pronounced NL63 population was also found with 4% of the positive results. Corona viruses are mainly detectable from late autumn to spring with a sharp increase in autumn and a peak from December to April. Only sporadic evidence was shown as the season progressed, but nevertheless the data indicate frequent circulation of coronaviruses [26]. Therefore, when testing asymptomatic people, more false-positive results can be detected, which is one reason for the increase in corona cases, especially in 2020, and explains the development of the test-positive rate to over 50% [9]. The fact that this would have to lead to a large number of medical treatments and also to an enormous number of sick leave was refuted on the basis of the available data. In the context of the corona pandemic, the phenomenon that a high positive rate also correlates with more cases of illness in contrast to the previous flu waves seems to have been eliminated. Since the coronaviruses, in particular with the establishment of the omicron variant, also show a reduced morbidity compared to influenza viruses [27], the positive rate cannot be used as a criterion for infection avoidance strategies and, on the other hand, the recording of test results should be validated.
This test strategy, even for asymptomatic people, was taken up by the Ifo Institute in 2020 and rated negatively [28]. Nevertheless, this increase in the positive rate is particularly evident in 2022, which can certainly be associated with the spread of the omicron variant of SARS-CoV-2. But if these corona tests had only been used in symptomatic patients, this should have resulted in an increase in ICD coding, which we are seeing, but on the other hand the sickness burden and sick leave would have to increase to the same extent. Our data show exactly the opposite trend. In 2021 in particular, all health insurance data examined indicate a significant decrease in respiratory diseases - despite SARS-CoV-2. This mismatch is based on the testing of healthy people, who are then classified as corona cases and which, in their exorbitant number, then led to politicians sticking to infection prevention strategies. For this reason, only the testing of symptomatic persons should be remunerated and only these test results should flow into a registration. During the pandemic, testing healthy people became a political control instrument to regulate containment measures, which should be reconsidered. Farkas et al. confirm this argument through their work on blanket testing of air travelers in spring 2022 at Heathrow and Bristol airports [29].
Our evaluations of test billing according to EBM from 2020 show a strong correlation between these 3 fee items (32816, 32006, 32841). It can therefore be assumed that in a large number of patients both an influenza and a SARS-CoV-2 test were billed and thus also evaluated. This is also reflected in the increase in ICD encryption for respiratory diseases from 71,199,754 in 2021 compared to 55,919,358 in 2019. Influenza A and B was encrypted 112,424 times in 2019 and still 33,727 times in 2021. Therefore, an under-recording of notifiable influenza cases on the part of the RKI's influenza working group must be regarded as the cause, which can be understandable given the exceptional pandemic situation. Heinzinger et al. bring the aspect of underreporting of influenza cases into the discussion. Possible reasons for lower submissions are a work overload of doctors due to the Covid-19 pandemic and a drop in demand from patients, who may have contacted a test center directly without consulting their general practitioner [7]. Furthermore, the weekly reports of the RKI from the second quarter of 2020 no longer contain any projections of flu cases for the entire German population, which was previously carried out regularly [10].
In summary, the decline in influenza A and B from the 2019/2020 season is based on a reduction in notifications in the sentinel practices system, the significant under-recording by the RKI and the general significant decrease in respiratory diseases - certainly also due to the corona pandemic and the associated containment measures. The authors propose the following recommendations for future exceptional pandemic situations and for recording respiratory infections:
- Clinical testing in symptomatic individuals only
- No compensation incentives for new testing procedures
- Include corona viruses in the statistical recording
- To establish a uniform test recording that is also used in the event of a pandemic
References
- WHO Influenza (Seasonal). https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal). letzter Zugriff 11.11.23 (2018).
- Zambon MC, Stockton JD, Clewley JP, et al. Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: an observational study. Lancet 358 (2001): 1410-1416
- de Fougerolles TR, Puig-Barbera J, Kassianos G, et al. A comparison of coronavirus disease 2019 and seasonal influenza surveillance in five European countries: France, Germany, Italy, Spain and the United Kingdom. Influenza Other Respi Viruses 16 (2022): 417-428.
- Buchholz U, Buda S, Prahm K. Abrupter Rückgang der Raten an Atemwegserkrankungen in der deutschen Bevölkerung. Epidemiologisches Bulletin 16 (2020): 7-9.
- Dzien A, et al. Will the COVID-19 pandemic slowdown in the northern hemisphere by the onset of summer? An epidemiological hypothesis. Infection 48: (2020), 627–629.
- Adlhoch C, et al. Very little influenza in the WHO European Region during the 2020/21 season, weeks 40 2020 to 8 2021. Eurosurveillance 26 (2021): 2100221.
- Heinzinger S, et al. Reciprocal circulation pattern of SARS-CoV-2 and influenza viruses during the influenza seasons 2019/2020 and 2020/2021 in the Bavarian Influenza Sentinel (Germany). Epidemiology and Infection 149 (2021): 1–7.
- Hu B, et al. Characteristics of SARS-CoV-2 and COVID-19. Nature Reviews Microbiology 19 (2021): 141-154.
- https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Testzahlen-gesamt.xlsx?__blob=publicationFile, letzter Zugriff 11.11.23
- https://survstat.rki.de/Content/Query/Create.aspx , letzter Zugriff 11.11.23
- Arbeitsunfähigkeit: Fälle und Tage nach Diagnosen 2020. Ergebnisse der Krankheitsartenstatistik der gesetzlichen Krankenversicherung. bundesgesundheitsministerium.de , 1-48
- Arbeitsunfähigkeit: Fälle und Tage nach Diagnosen 2019. Ergebnisse der Krankheitsartenstatistik der gesetzlichen Krankenversicherung. www.bundesgesundheitsministerium.de. 1-52
- https://www.rki.de/DE/Content/Infekt/Sentinel/Grippeweb/grippeweb_node.html, letzter Zugriff 11.11.23
- Fricke LM, Glockner S, Dreier M, et al. Impact of non-pharmaceutical interventions targeted at COVID-19 pandemic on influenza burden - a systematic review. J Infect 82 (2021): 1-35
- Eigner U, Verstraeten T, Weil J. Decrease in norovirus infections in Germany following COVID-19 containment measures. Letters to the Editor / Journal of Infection 82 (2021) 276-316.
- Wu D, Liu Q, Wu T, et al. The impact of COVID-19 control measures on the morbidity of varicella, herpes zoster, rubella and measles in Guangzhou, China. Immun Inflamm Dis 8 (2020): 844-846
- de Miguel Buckley R, Trigo E, de la Calle-Prieto F, et al. Social distancing to combat COVID-19 led to a marked decrease in food-borne infections and sexually transmitted diseases in Spain. J Travel Med 27(2020): taaa134
- Steffen R, Lautenschlager S, Fehr J. Travel restrictions and lockdown during the COVID-19 pandemic-impact on notified infectious diseases in Switzerland. J Travel Med 27 (2020): taaa180
- Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. Engl J Med 382 (2020): 727-733.
- Lamb RA, Choppin PW. The gene structure and replication of influenza virus. In: Annual Review of Biochemistry 52 (1983): 467-506.
- Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 368 (2020): 860-868.
- Jefferson T, Del Mar CB, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews 11 (2020): CD006207.
- Bjørnskov, Christian. “Did Lockdown Work? An Economist’s Cross-Country Comparison.” CESifo Economic Studies 00 (2021):14.
- Herby, Jonas, Lars Jonung, et al. “Protocol for ‘What Does the First XX Studies Tell Us about the Effects of Lockdowns on Mortality? A Systematic Review and Meta-Analysis of COVID-19 Lockdowns.” SSRN Electronic Journal (2021)
- Park S, Lee Y, Michelow IC, et al. Global Seasonality of Human Coronaviruses: A Systematic Review. Open forum infectious diseases 7 (2020): ofaa443.
- Biere B, Djin-Ye O, Wolff T, et al. Surveillance of endemic human Coronaviruses in Germany, 2019/2020. The Lancet Regional Health - Europe 11 (2021): 100262
- Pezzullo AM, Axfors C, Contopoulos-Ioannidis DG, et al. Age-stratified infection fatality rate of COVID-19 in the non-elderly population. Environ Res 216 (2023): 114655.
- Dorn F, Fuest C, Gstrein D, et al. Corona-Infektionen und die Dunkelziffer: Vergleichen wir Äpfel mit Birnen? ifo Schnelldienst digital 12 (2020): S1-5.
- Farkas K, Williams R, Alex-Sanders N, et al. Wastewater-based monitoring of SARS-CoV-2 at UK airports and its potential role in international public health surveillance. PLOS Global Public Health 3 (2023): e0001346.


 Impact Factor: * 3.4
Impact Factor: * 3.4 Acceptance Rate: 78.89%
Acceptance Rate: 78.89%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 