Spinal Instrumentation in Spondylodiscitis: An Experience from Saudi Arabia
Ahmed A Farag1*, Bokhary Mahmoud2, Wael Hammad2, Mohamed A Khoudir3, Faisal A Sukkar4
1Department of Neurosurgery, King Abdullah Medical City, Holy Capital, Mecca, Saudi Arabia
2Department of Neurosurgery, Armed Force Hospital, Southern Region, Saudi Arabia
3Department of Neurosurgery, Aseer Central Hospital, Abha, Saudi Arabia
4Department of Neurosurgery, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
*Corresponding Author: Ahmed A Farag, Department of Neurosurgery, Assistant Consultant Neurosurgery, King Abdullah Medical City, Holy Capital, Mecca, Saudi Arabia
Received: 10 November 2020; Accepted: 23 November 2020; Published: 26 November 2020
Article Information
Citation:
Ahmed A Farag, Bokhary Mahmoud, Wael Hammad, Mohamed A Khoudir, Faisal A Sukkar. Spinal Instrumentation in Spondylodiscitis: An Experience from Saudi Arabia. Journal of Spine Research and Surgery 2 (2020): 115-129.
View / Download Pdf Share at FacebookAbstract
Objective: For evaluation of safety and effectiveness of instrumentation in treatment of spondylodiscitis cases, taking into consideration the clinico-radiological outcome.
Material and Method: In a retrospective case series study, patients of spondylodiscitis were operated between 2015 and 2019 in Armed Force Hospital Southern Region, Saudi Arabia. The data of the 30 patients who had suffered from spondylodiscitis have been analyzed and studied.
Results: 30 patients with spondylodiscitis were included. Male to female ratio 2.3:1 and the mean age in our study was 50 ± 2 years. Predisposing risk factors in these cases were found in 22 patients (73.3%). The mean duration of follow up was 7 ± 1 months. The mean VAS score was 8 ± 1 before surgery and 2 ± 1 at end of follow up with a markedly significant p-value (<0.001). The mean Barthel index was 45 ± 16 (range, 10 -70) before surgery and 90 ± 18 (range, 65-100) at end of follow up period with a highly significant p-value (<0.001).
Conclusion: Spinal instrumentation is an effective and safe method in the treatment of spondylodiscitis in selected patients.
Keywords
<p>Spondylodiscitis, Instrumentations, Spinal Infection, Visual Analogue Scale</p>
Article Details
Abbreviations
VAS: Visual Analogue Scale; AFHSR: Armed Force Hospital Southern Region; TLIF: Transforaminal Lumbar Interbody Fusion; ACDF: Anterior Cervical Discectomy And Fixation; PEEK: Polyetheretherketone
1. Introduction
Spondylodiscitis is a relatively rare disorder, accounts for 2-4% of all infectious bone disease, but an increase in the incidence of pyogenic as well as granulomatous spondylodiscitis has been reported [1]. It frequently follows some kind of recent infections or surgical procedure, and this depends on invasiveness of the operation [2]. The lumbar and the thoracic regions are affected in 50% and 35 % of patients, respectively; the cervical spine is affected in 3 to 10% of cases [3]. Spondylodiscitis symptoms are usually non-specific with insidious onset and often underestimated by the patient. Back or neck pain is the most frequent presenting complaint, and spinal tenderness is the commonest sign detected on examination [4-6]. Diagnosis of spondylodiscitis necessitating specific laboratory and radiological studies, with MRI which is the modality of choice [7].
The majority of patients with spondylodiscitis can be treated conservatively. Though non-surgical treatment may terminate the infection in most cases, it does not, however, avoid deformity that can lead to chronic spine pain. The surgery is indicated for cases with neurologic deficit, abscess formation, destruction of endplates evident with proper imaging, chronic osteomyelitis with instability in dynamic x-ray, local kyphosis, septic pseudarthrosis or failure of medical treatment. For the management of these cases, several surgical approaches exist and the choice of specific approach depends on the pathology, whether anterior or posterior, and co-existence of spinal instability. Instrumentation in the presence of active infection is still controversial [8]. In the presence of active infection, internal spinal fixation began to gain some popularity in reconstructive surgery with the advantages of improved sagittal balance and substantial fusion rates. Instrumentation can also minimize the need for prolonged external immobilization as opposed to non-instrumented situations [9, 10].
2. Materials and Methods
2.1 Study setting
This study was performed in Neurosurgery Department, AFHSR, Saudi Arabia. The study type was retrospective observational one. The study was conducted over a period of almost four years (Nov 2015 to December 2019). A total of 30 patients were included.
2.2 Inclusion criteria
We included patients who had been diagnosed as spondylodiscitis not responding to medical treatment within maximum 6 weeks as evidenced by persistent pain and persistent elevation ESR and CRP. Patients with significant neurological deficit due to compressive mechanism, epidural abscess, spinal deformity, or instability.
2.3 Exclusions criteria
We excluded patients responded to medical treatment or unfit for surgery and also patients had multiple distant levels more than two distant levels.
2.4 Clinical management
The patients were subjected to
- -History taking with stress on any past history of diseases, drug, operation, or any invasive spinal procedure and history of TB or contact with animals. VAS was used to assess the severity of pain.
- -Complete general examination with searching for primary infection and systemic disease that may affect the surgery, and neurological assessment.
- -All patients submitted to routine laboratory investigations with special interest for CRP, ESR and WBC count: Blood culture, urine culture, sputum culture. CRP level was used as a serum marker during follow-up.
- -Neuroimaging studies (plain X-ray- CT-MRI); MRI (with gadolinium contrast) was the gold standard in the diagnosis.
2.6 Surgical procedures
Different technique and instrumental approaches have been used in the managemnt of these patients according to their pathology, including:
- a. Anterior corpectomy and reconstruction by either (titanium mesh cage and z-plate or expandable cage).
- b. Posterior decompression and transpedicular screws fixation.
- c. Single stage Combined anterior and posterior approach.
- d. Lateral extracavitary approache with posterior Transpedicular screws fixation.
- e. TLIF and Posterior Instrumentation.
Biopsy material sent for aerobic, anaerobic, fungal, mycobacterial cultures and stained with gram stain, Ziehl-Neelsen and special stain for fungi.
Postoperative empiric antibiotics were given then were modified according to cultures results.
2.7 Follow up and outcome
The patients were followed monthly post-operative
taking into consideration the clinical outcome using Barthel Index, as regarding activity of daily living, and Visual pain analogue scale (VAS) was used to assess the severity of pain. These data were compared with the preoperative state. Also follow up included the laboratory markers (WBC count, CRP and ESR) and radiological follow up, included X-rays within 3 days post-operatively, and CT was done in cases that needed more evaluation. We performed the one-sample t-test and the paired t-test using SPSS 12.0 for statistical comparisons. In all cases, p values < 0.05 were, statistically, considered significant.
3. Results
3.1 Age range
The mean age was 50 ± 2 years, ranging from 22 to 62 years, in 30 patients with spondylodiscitis.
3.2 Gender distribution
9 female (30%) and 21 male (70%), with a male: female ratio of 2.3:1.
3.3 Risk factors
Risk factors in these cases were observed in 22 patients (73.3%), 10 patients underwent spinal surgeries, 9 patients underwent lumbar spine surgery and lumbar puncture in one reported case of meningitis. 6 patients were having diabetes, 3 patients with liver disease, 1 patient was suffering from end-stage renal disease, 1 patient was a smoker and 1 woman was on chronic steroid use for systemic lupus erythromatosis.
3.4 Clinical presentation
The period of symptoms prior to diagnosis was between 2 and 24 weeks, with a mean duration of 11.60 ± 6.64 weeks. Persistent back pain, local spinal tenderness during palpation, paravertebral muscle spasm in 26 cases, fever in 11 cases, radiculopathy in 10 cases and radiculopathy of the neck and upper limbs in one case were found. Neurological deficits have been detected in 6 cases, and in 1 case, deformity (Table 1). The lumbar spine (21 cases) was the most common site of infection in our series, followed by the thoracic spine (5 cases). Lumbosacral spines were diagnosed in three cases, with the cervical area being the least affected (one case). The number of vertebral bodies affected was: one vertebra in four patients, two vertebrae in 25 patients, and four vertebrae in one patient. In these cases, the indications of surgical intervention were medical trial failure for 3 weeks in 9 cases, as indicated by persistent elevation of inflammatory markers and radiological progression of the inflammatory phase, the development of abscesses (6 cases), Extreme chronic pain (5 cases), cognitive deficit (4 cases), end-plate destruction and severe pain (3 cases), deformity (2 cases), and, in one case, the diagnosis was unclear in the presence of end-plate destruction (Table 2).
|
Clinical picture |
No. of cases |
% |
|
Back pain, tenderness and spasm |
26 |
86.66 |
|
Fever |
11 |
36.60 |
|
Radiculopathy |
10 |
33.33 |
|
Neurological deficit |
6 |
20 |
|
Deformity |
1 |
3.33 |
|
Neck pain and brachialgia |
1 |
3.33 |
Table 1: Clinical pictures in the studied cases.
|
No. of patients |
% |
Indications |
|
9 |
30 |
Failure of medical management |
|
6 |
20 |
Abscess formation |
|
5 |
16.7 |
Severe persistent pain |
|
4 |
13.3 |
Neurological deficit |
|
3 |
10 |
Endplate destruction and severe pain |
|
2 |
6.7 |
Neurological deficit and deformity |
|
1 |
3.3 |
Unsure diagnosis and destruction of end plate |
Table 2: Indications for surgical intervention in our patients.
Twenty-one patients were referred to the posterior approach only, two patients were referred to the anterior approach only (one retroperitoneal and the other anterior cervical), and three patients were referred to the combination anterior and posterior approach. TLIF and posterior instrumentation were used in 3 other patients, while the lateral extracavitary approach with posterior instrumentation was used in one case (Figure 1). Transpedicular screws used in 24 patients, PEEK cage with transpedicular screws used in 3 patients, expandable anterior plate cage in one patient, titanium mesh cage anterior plate in one patient and titanium mesh cage transpedicular screws in another patient. In one case of TB spondylodiscitis, pre-operative CT guided aspiration of the paraspinal cold abscess was carried out. For periods ranging from 6 to 10 months with a mean of 7 ± 1 months, all patients were followed up. Complication was identified in 6 cases (20%); 1 case of intraoperative dural tear, handled with immediate intraoperative end to end watertight direct dural closure without postoperative leakage, 3 cases of superficial wound infection, treated with superficial debridement and antibiotics, In one case, malposition of transpedicular screws was found but without any symptoms and the patient declined a second repositioning procedure. Except for one case that died 6 months after surgery from chronic renal failure, no mortality was reported in our series (Figure 2). Postoperatively, inflammatory markers in all cases were normalised within 2-4 weeks (Figures 3 and 4). In all our 30 patients, tissue cultures were collected, but no bacterial growth was isolated in 5 patients. Among the 25 positive culture patients, the most common strain was Staphylococcus Aureus in 8 cases , followed in 6 cases by mycobacterium tuberculosis. In 4 cases, Brucella was isolated, in 2 cases, Streptococci, and in 2 cases, Coagulase -ve staph. Also isolated were Escherichia coli, Pseudomonas and Pneumococci, each in a single case (Figure 5). The mean VAS score (Figure 6) was 8 ± 1 (range, 6 -10) before surgery and 2 ± 1 (range, 1-4) with a significant p-value (< 0.001) at the end of the follow-up period. The mean Barthel index (Figure 7) was 45 ± 16 (range, 10 -70) before surgery and 90 ± 18 (range, 65-100) with a markedly effective p-value (< 0.001) at the end of the follow-up period. In all patients, no recurrence of the infection was reported until the end of the follow-up. Radiologically, symptoms of infection were resolved, with sufficient fusion in all bone graft patients, and no hardware defects, with strong sagittal alignment.
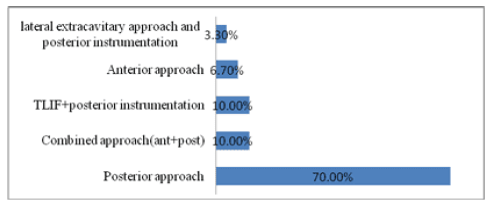
Figure 1: Surgical approaches.
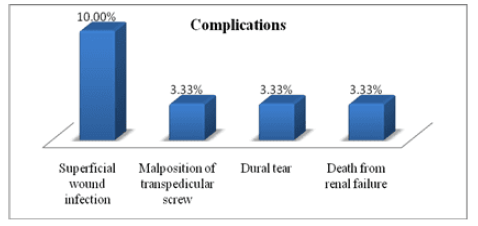
Figure 2: Percent distribution of complications among the studied group.
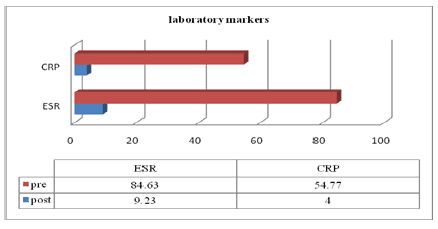
Figure 3: The mean values of laboratory markers preoperative and at 4 weeks.
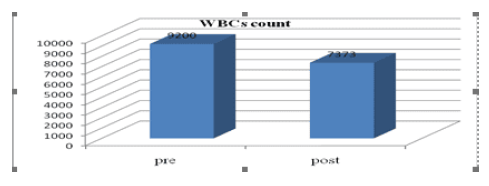
Figure 4: The mean values of WBCS count preoperative and at 4 weeks.
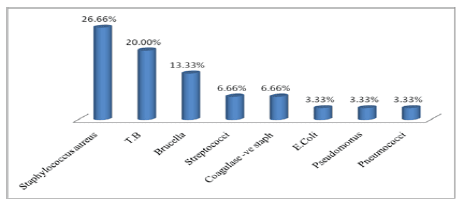
Figure 5: Causative organisms.
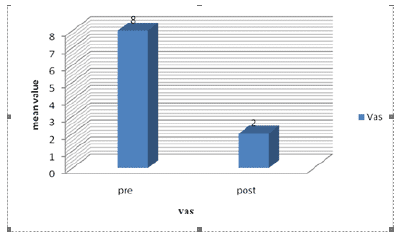
Figure 6: Comparison between the mean value of VAS scores preoperative and at the end of follow up.
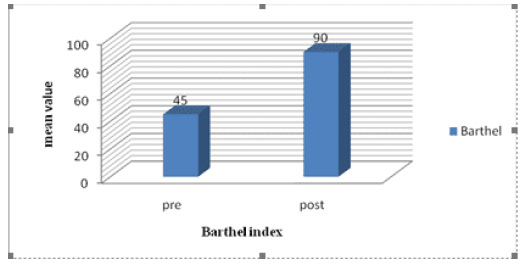
Figure 7: comparison between the mean value of Barthel index preoperative and at the end of follow up.
3.5 Case Presentation
3.5.1 Case 1: A 51-year-old male patient, diabetic, postoperative spondylodiscitis L4-5 (Figure 8), treated with posterior approach (Figure 9), showed streptococcus infection in culture.
3.5.2 Case 2: Male 60-year-old T10-11 tuberculosis spondylodiscitis (Figures 10 and 11), treated with a combined method (Figure 12).
3.5.3 Case 3: A heavy smoker with C5-6 tuberculous spondylodiscitis (Figure 13 and 14) treated with anterior corpectomy and expandable cage, plate and screws (Figure 15) is a 65-year-old male patient.
3.5.4 Case 4: Laminectomy-treated 55-year-old male diabetic patient, T10-T11 pyogenic spondylodiscitis (Figure 16), with posterior transpedicular screw fixation (Figure 17).
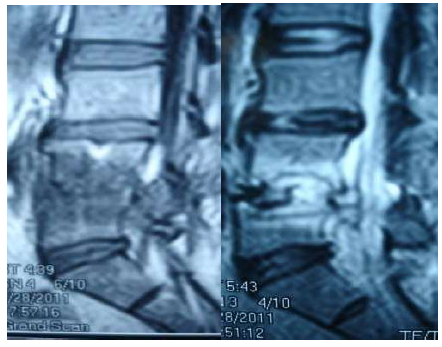
Figure 8: Post-discectomy MRI (2months postoperative).
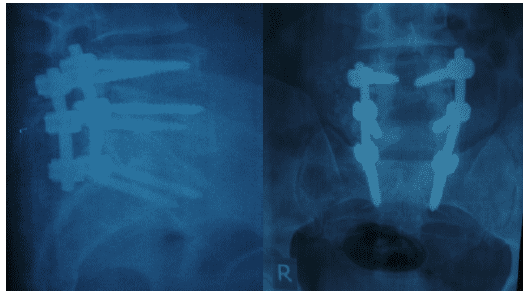
Figure 9: Post-fixation plain x-rays (lateral - AP) views.

Figure 10: Preoperative CT scan showed destruction endplates and narrow space.

Figure 11: Preoperative MRI T1 and T2.
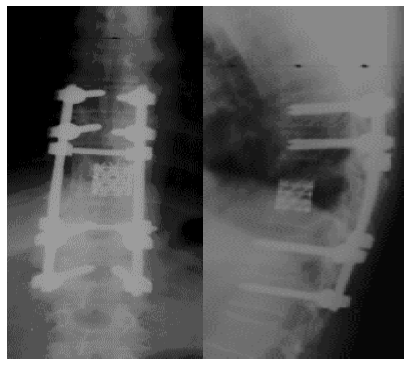
Figure 12: Postoperative plain x-rays (AP- lateral) views.
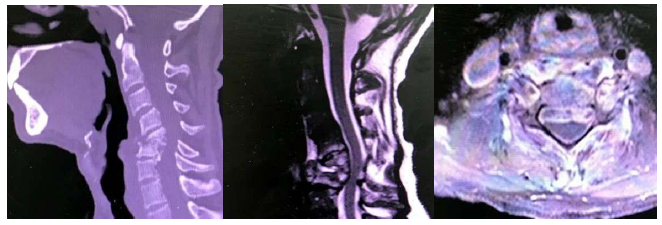
Figure 13: Preoperative CT, MRI Sagittal T2, and axial T1 with contrast.
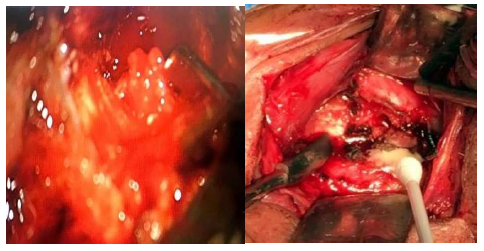
Figure 14: Intraoperative showed necrotic tissue and caseous material.
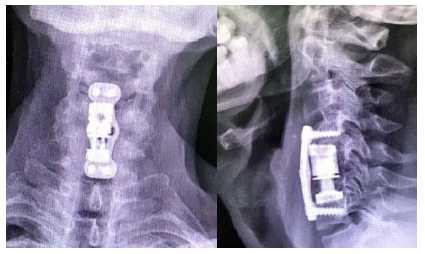
Figure 15: Postoperative Plain x ray AP and Lateral views.

Figure 16: MRI of thoracic spine.
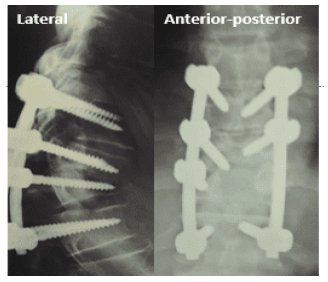
Figure 17: Postoperative Plain x ray AP and Lateral views.
4. Discussion
In beginning of 1990s, internal fixation, in the setting of active infection, started gaining some acceptance in reconstructive spinal surgery [10]. Anterior cervical plating with ACDF is recommended for management of cervical pyogenic spondylodiscitis with better surgical outcomes compared with ACDF without plating. Kim et al [11] found that, fusion rate was higher in the ACDF with plating group as compared with the ACDF without plating group. Also, Luo et al. [12] analyzed 7 patients with lumbar spondylodiscitis treated with PEEK cages loaded with autologous bone graft, and posterior transpedicular fixation. The infection had been resolved in all patients without relapse and solid fusion was obtained in all patients had. Lim et al [8] found that, recurrence of infection is the same in cases with and without instrumentation and this indicating that its use may not be a contraindicated in presence of infection. Our study included 30 patients with spondylodiscitis who underwent surgical management with spinal instrumentation. In this study, the number of male patients was 21cases (70%), and the number of female patients was 9 cases (30%), with male: female ratio 2.3:1. In Lim el [8] study on 28 patients, the male to female ratio was 3:1, and in the study conducted by Pee et al [13], it involved 60 patients, the male to female ratio 1.5:1. This means that our study correlates with other studies in the predilection of spondylodiscitis for male population. The mean age of our cases was 50 years (ranged from 22 to 68 years) which is very close to the mean age of 51 years reported by Lim et al [8], but lower than the mean age of 58 years reported by Pee et al [13], and the mean age of 56.8 years reported by Lee et al [14].
The risk factors encountered in this study, were identified in 86.7% of cases, and the most common predisposing factor was previous spinal surgery / lumbar puncture 10 (33.3%) followed by diabetes mellitus 6 (20.0%), systemic infection 10.0%, liver disease 10.0%, chronic renal disease (3.3%), and other predisposing factors, such as smoking (1 case), intravenous drug abuse (1 case) and one female (3.3%) on chronic steroid for systemic lupus erythromatosis. The reported risk factors, In the study by Lee et al [14] were; diabetes mellitus (44%); long term steroid drug use (24%); malignancy (17%); and alcoholism (11%) and in study by Lim et [8] the previous spinal surgery and diabetes mellitus were the most common predisposing factors for their cases. Diagnosis of spondylodiscitis in our study was based on clinical presentation; radiological studies, and hematologic examinations, with the duration of complaint before diagnosis ranged from 2 to 24 weeks with the mean duration 11.60 ± 6.64 weeks which is correlated with that reported by most authors [4]. This delay in the diagnosis occurred because the onset of symptoms is insidious, can be sometimes not specific, vague or almost absent, and often underestimated by the patients. The rarity of the disease and the high frequency of low back pain in general population was also a contributing factor to delayed diagnosis. Furthermore, it gives a chance for complications to occur, the same rationale mentioned by Mariconda et al. [15].
Most of cases in this study presented with persistent back pain, and the most common signs were local tenderness and paravertebral muscle spasm, presented in 86.66% (26 cases). Fever was present in 11 cases (36.60%), radiculopathy in 10 cases (33.33%), neurological deficit in 6 cases (20%), deformity in 1 case (3.33%), and neck pain & brachialgia in 1 case (3.33%). This is similar to study of Lee et al [14], who reported that, the most common clinical presentation was axial spine pain presented in (95%) followed by radicular pain in 20 to 65% of cases, and 15% present with neurological deficits, which is slightly lower than that in our study. CRP value was the preferred laboratory marker for monitoring response to treatment in this study as it has short half-life and rapidly normalized and this is similar to what Zarrouk et al [16] decided. The lumbar spine was the most affected site of spondylodiscitis in 21 cases (70.00%), followed by the thoracic spine in 5 cases (16.66%) that the lumbosacral and cervical spines were involved in three cases (10.00%) and one case (3.33%), respectively. Regarding the isolated organisms in our study there were no bacterial isolates in 5 patients (16.7%) which is almost the same as the (16.2%) reported by Pee et al [13], but lower than 43% reported by Lim et al [8] Staphylococcus aureus was the most common, isolated strain, in our series (26.7%), followed by mycobacterium tuberculosis (20.0%), with a similar results in the study of Lim et al [8] in which the most common identified bacteria was staphylococcus (25%). Indications of surgery in this study were failure of medical management which was the most common indication (30%) after at least 2-3 weeks, followed by abscess formation (20%), severe persistent pain (16.7%), neurological deficit (13.3%), and multiple indications (20%) such as endplate destruction, spinal deformity, severe pain, neurological deficits and unsure diagnosis.
In a study done by Pee et al [13], indications for treatment were mostly due to persistent pain, failure of medical treatment, vertebral body destruction, and large abscess formation. Fifty-eight patients from sixty (96.7%) complained of severe back pain and this higher difference because pain is a subjective variable. Posterior approach used in 21 patients (70%) in our cases and 2 patients (6.7%) were managed with the anterior approach only (one case by retroperitoneal and another case by anterior cervical approach), 3 patients (10%) were managed with a single stage combined anterior and posterior approach. In another 3 patients (10%), TLIF and Posterior fixation were used, while the lateral extracavitary approach with posterior instrumentation was used in one case (3.3%). In the study of Lim et al [8], anterior interbody fusion with anterior instrumentation was done in 13 patients (46%). Anterior interbody fusion with posterior fixation was performed in15 cases (54%), and a two-staged surgery was done in 6 patients (21%). In the study conducted by Pee et al [13] the combined approach (a one-stage anterior debridement and fusion followed by posterior instrumentation) was performed. Instrumentation used in our cases depended on the type of approach and availability of the implants; transpedicular screws alone was used in 24 patients (80%), this is because posterior approach was the most predominant in our study, transpedicular screws with PEEK cage in 3 patients (10%), expandable cage with anterior plate in one patient (3.3%), anterior plate with titanium mesh cage in one patient (3.3%) and transpedicular screws with titanium mesh cage in another patient. Bone graft was used in 7 cases (23.3%); iliac bone graft in 6 cases (20.0%), Rib and Iliac bone graft in the other case (3.3%).
In a study of Lee et al [14], wide variations of graft were used (autograft, allograft from ribs, fibula, humerus, iliac bone, femur and bone morphogenic protein) and in study of Pee et al [13], autologous iliac bone graft or a bone-chips-filled cage was used. It is generally agreed that the administration of antibiotics is warranted. But the dosage, route, and duration of antibiotic therapy advocated by various investigators have been extremely debated. In our cases, the postoperative antibiotics were administered intravenously for 6 weeks, and orally for 6 weeks, and the duration was monitored by ESR and CRP values, the same regimen was used by Pee et al [13]. The incidence of Complications in our series was 20% (6 cases); one case of intraoperative dural tear (3.3%) which was managed with direct closure, superficial wound infection occurred in three cases (10%) which were resolved by superficial debridement and antibiotics. Mal-position of transpedicular screws was noticed in one case (3.3%) but without symptoms. No mortality in our series except one case (3.3%) who died 6 months after surgery from chronic renal failure. Lee et al [14] reported complications in rate of 20% while Pee et al [13] reported a rate of 9.7% complications. We found a relation between the route of spread of infection and the incidence of complications as all complications, occurred in our series, were in patients with hematogenous spread of infection rather than the postoperative patients. To the best of our knowledge, the cause of death in all published series was not related to the surgery, the instruments, the persistence or the recurrence of infection However, it was related to preoperative systemic disease which mostly reflected the compromised health of the patients.
In our study, as well as in study of Lim et al [8], ESR, CRP and leukocyte counts were normalized within 6 months. In our series, it has been noticed that the neurological outcome after surgery for spondylodiscitis was determined mostly by preoperative neurological state, and this is similar finding in most published series. It is unusual for neurological worsening to be due to surgery itself. Nevertheless, postoperative neurological deterioration is often associated with recurrence [17]. No recurrence of infection were noted in any of our patients till end of follow up period and these findings were consistent with other published literature [18]. Postoperative radiological studies revealed adequate fusion in all patients with bone graft, and bone trabeculae at the graft were documented. In series of Lim et al [8], a successful interbody bony fusion was reported in 27 patients from 28 and Luo et al [12] analyzed 7 patients with lumbar spondylodiscitis who treated with PEEK cages loaded with autologous bone graft, and posterior transpedicular screw fixation. The infection had been resolved in all their patients without relapse and all patients had solid fusion within a 2-year follow-up.
4.1 Recommendations for study
For patients with spondylodiscitis who do not tolerate
pain, who have a neurological deficiency due to compression or spinal instability, and those who do not respond to conservative medical care, spinal instrumentation is a better option.
4.2 Limitations of study
A significant number of patients should be included, as well as a longer duration of follow up, in order to generalize our study results.
5. Conclusion
Spinal instrumentation is an effective and safe method in the treatment of spondylodiscitis in appropriately selected patients. If infected tissue is completely debrided, instrumentation shows neither persistence nor recurrence of infection and does shorten the hospitalization. Further study would be necessary to give a more definite conclusion.
Conflict of Interest
The authors certify that there is no conflict of interest with any financial organization about the material described in the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics Approval and Consent to Participate
All patients were consented before they do the surgery. All data used was anonymized and encrypted to comply with all research ethics. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Sobottke R, RöllinghoFF M, Zarghooni K, et al. Spondylodiscitis in the elderly patient: clinical mid term results and quality of life. Arch Orthop Trauma Surg 130 (2010): 1083-1091.
- Hsieh MK, Chen LH, Niu CC, et al. Postoperative anterior spondylodiscitis after posterior pedicle screw instrumentation. The Spine Journal 11 (2011): 24-29.
- Acosta FL Jr, Chin CT, Quinones-Hinojosa A, et al. diagnosis and management of adult pyogenicosteomyelitis of the cervical spine. Neurosurg Focus 17 (2004): E2.
- Cone LA, Hirschberg J, Lopez C, et al. Infective endocarditis associated with spondylodiscitis and frequent secondary epidural abscess. Surg Neurol 69 (2008): 121-125.
- Mann S, Schütze M, Sola S, et al. Nonspecific pyogenic spondylodiscitis: clinical manifes-tations, surgical treatment, and outcome in 24 patients. Neurosurg Focus 17 (2004): 1-7.
- Euba G, Narvaez JA, Nolla JM, et al. Long-term clinical and radiological magnetic resonance imaging outcome of abscess-associated spontaneous pyogenic vertebral osteomyelitis under conservative management. Semin Arthritis Rheum 38 (2008): 28-40.
- Dimar JR, Carreon LY, Glassman SD, et al. Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine 29 (2004): 326-332.
- Lim JK, Kim SM, Jo DJ, et al. Anterior Interbody Grafting and Instrumentation for Advanced Spondylodiscitis. J Korean Neurosurg 43 (2008): 5-10.
- Christodoulou AG, Givissis P, Karataglis D, et al. Treatment of tuberculous spondylitis with anterior stabilization and titanium cage. Clin Orthop 444 (2006): 60-65.
- Fukuta S, Miyamoto K, Masuda T, et al. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine 28 (2003): E302-E308.
- Kim SK, Park JB, Chung JY, et al. Anterior Cervical Debridement and Fusion for Cervical Pyogenic Spondylodiscitis: Use of Anterior Cervical Plating or Not?. Spine 45 (2020): 431-437.
- Luo W, Zhu Y, Zhao ZH, et al. Application of polyetheretherketone cages through minimally invasive oblique retroperitonealapproach for the treatment of lumbar polymicrobial spondylodiscitis. a STROBE-compliant retrospective study with 7 cases. Medicine 99 (2020): 17(e18594).
- Pee YH, Park JD, Choi YG, et al. Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone struts versus cage. J Neurosurg Spine 8 (2008): 405-412.
- Lee MC, Wang MY, Fessler RG, et al. Instrumentation in patients with spinal infection. Neurosurg Focus 17 (2004): E7.
- Mariconda M, Cozzolino A, Attingenti P, et al. Osteoarticular tuberculosis in a developed country. J Infect 54 (2007): 375-380.
- Zarrouk V, Feydy A, Salles F, et al. Imaging does not predict the clinical outcome of bacterial vertebral osteomyelitis. Rheumatology (Oxford) 46 (2007): 292-295.
- Ouellet J, Jarzem P, McGill RR. factors predicting good outcome in surgical management of spondylodiscitis. Internation- al society for the study of lumbar spine. 34th annual meeting abstracts (2008).
- Kuklo TR, Potter BK, Bell RS, et al. Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech 19 (2006): 376-382.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 