Study on the Role of Non Penetrating Titanium Clips in Dural Repair
Naveenkumar kuppan1*, Krishnakumar R2
1Department of Orthopaedics & Spine surgery, Sree Manakula Vinayagar Medical College & Research Centre, Puducherry, India
2Department of Spine surgery, Consultant, Medical Trust Hospital, Kochi, India
*Corresponding Author: Naveenkumar kuppan, Department of Orthopaedics & Spine surgery, Sree Manakula Vinayagar Medical College & Research Centre, Puducherry, India
Received: 14 May 2020; Accepted: 26 May 2020; Published: 01 June 2020
Article Information
Citation:
Naveenkumar kuppan, Dr. Krishnakumar R. Study on the Role of Non Penetrating Titanium Clips in Dural Repair. Journal of Spine Research and Surgery 2 (2020): 067-076.
View / Download Pdf Share at FacebookAbstract
Study design: A Prospective study. Objective: Dural injuries (Durotomy) are a common complication often seen in spine surgeries. Primary repair of dura using conventional techniques with sutures (silk or prolene) is considered gold standard in management.
Overview of Literature: The use of Non-penetrating Titanium clips as an alternate for the sutures in Dural closure has been described in literatures. The surgical use of titanium clips alone for the primary repair of dura in spine surgeries is yet to be substantiated. Aim of this study is to assess the role of non-penetrating Titanium clips in Dural repair surgeries.
Methods: This is a study conducted from November 2017 to July 2019 involving a total of hundred forty one spine patients. Thirty seven patients who had undergone spinal epidural steroid injections and scoliosis surgeries were excluded from the study. Of the hundred and four cases, fifteen cases had undergone Dural repair. Non-penetrating Titanium clips were applied in five of the cases.
Results: Among the five cases, three were female and two male patients. Three cases undergone spinal decompression and fusion, one case of microdiscectomy and one case of intradural extramedullary tumor excision. Size of Dural tear range from 0.5 cm to 3 cm. The number of clips applied ranges from one to fifteen numbers. Among the study group, four patients had a smooth post-operative period without any signs and symptoms. One patient who had undergone intradural tumor excision, developed post-operative wound leakage and postural headache.
Conclusion: Non-penetrating titanium clips produce complete Dural closure with no suture holes. We conclude non-penetrating clips can be used as an alternative for conventional sutures for durotomy repair.
Keywords
<p>Non-penetrating Titanium Clips, Dural Repair, Pseudo Meningocele</p>
Article Details
1. Introduction
Dural injuries (Durotomy) are a common complication often seen in spine surgeries. The incidence of Dural tear in primary surgeries is 3%, while 16% [1] in revision surgeries. Management of a Dural tear is a demanding task for surgeons. Primary repair of the dura using conventional techniques such as sutures (silk or prolene) is considered gold standard. Failure rate with direct repair using sutures varies from 5% to 9% [2].
The neurological sequelae following inadequate Dural repair include CSF leakage, pseudo meningocele, root herniation and CSF fistulas [3]. The use of Non-penetrating Titanium clips as an alternate for sutures in Dural closure has been described in literatures. The surgical use of titanium clips alone for the primary repair of dura in spine surgeries is yet to be substantiated. Aim of this study is to assess the role of non-penetrating Titanium clips in Dural repair surgeries.
2. Material and Method
This is a prospective study conducted at our institute from November 2017 to July 2019 involving a total of hundred forty-one patients, who had undergone spine surgery. Institutional ethical committee approval was obtained and a detailed consent was obtained from all the patients involved in this study. Thirty seven patients who had undergone spinal epidural steroid injections and scoliosis surgeries were excluded from the study. All surgeries were performed by a single surgeon. Of the hundred and four cases, fifteen cases had undergone Dural repair (Chart 1).
Among them, ten cases had Incidental Dural tear and three cases undergone durotomy for intradural tumor excision. Non-penetrating Titanium clips were applied in five among the fifteen Dural repair cases. The number of clips applied vary on the size of the Dural tear. Valsalva given intraoperatively (40mm of Hg for 10 seconds [4]) after applying the clips and patency of the closure noted. Drain was kept in low pressure active suction mode. Tight sub fascial closure was done using 1-0 vicryl, 2-0 vicryl and skin closure was done with staples. Mobilization was started from day two to five depending upon patients’ tolerance.
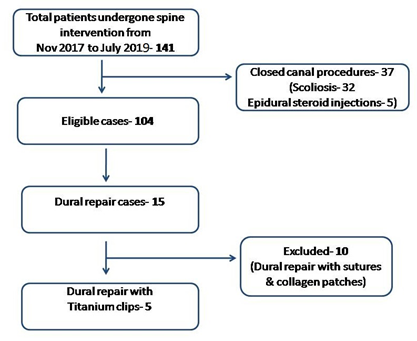
Chart 1: Shows patient selection criteria for the study.
3. Results
Among the five cases, three were female and two male patients. Age range from 43 to 72 years, with a mean age of 56.8 years. Two cases involve a Dorsal spine level and three cases involve the Lumbar spine. Three cases undergone spinal decompression and fusion, one case of microdiscectomy and one case of intradural extramedullary tumor excision. Size of Dural tear range from 0.5 cm to 3 cm, with a mean size of 1.16cms (Chart 2).
Non-penetrating Titanium clips small size was used in all our cases. The number of clips applied ranges from one to fifteen numbers, with a mean of 5 clips. Drain was kept in all cases except in a case of microdiscectomy. Intraoperative Valsalva maneuver showed all repairs were patent. Among the study group, four patients had a smooth post-operative period without any signs and symptoms of Dural leak. Wound was dry and clean in further follow ups. One patient who had undergone intradural tumor excision, developed post-operative wound leakage and postural headache.
3.1 Case illustration
57-year-old patient came to our institution with walking difficulty, pain and weakness over left leg. History of difficulty in micturition was present. On examination, patient found to have motor and sensory deficits with exaggerated reflexes. MRI shows a hypointense lesion in T2 weighted images around D1 to D3 seen dorsally compressing the cord (Figure 1).
Patient explained about the surgical procedure and the risks involved. Patient undergone intradural tumor excision of the intradural extramedullary mass (D1 to D2 Schwannoma causing Compressive myelopathy) with a durotomy size of 3cms (Figure 2, 3 & 4), fifteen titanium clips were applied. Intraoperative Valsalva was patent, shows a tight closure without CSF leakage. Drain kept and tight sub fascial closure done. He was kept in absolute bed rest in reverse Trendelenburg position for 2 days. Patient developed severe postural headache, wound leakage and multiple episodes of cough post operatively on day two. Third post-operative day his symptoms progressed and he started developing worsening of neurology. MRI was done, showing pseudo meningocele with spinal cord herniation at the surgical site (Figure 5 & 6). Emergency surgery was planned. On re-exploration there was collection of CSF in surgical site, all the titanium clips seen given away and cord was seen bulging out through durotomy site like a trap door. CSF collections were suctioned out and cord repositioned. All the Titanium clips were removed with ease. There were no difficulties in removing the clips and no incidence of Dural injuries. Dura was inspected for any further tear. Dural repair done using 5-0 silk. Repair site augmented with tissue glue coated collagen sponge [5, 6] (Collagen & Fibrinogen patch- Tachosil). Drain kept and water tight closure done. Post-operative period was uneventful. Drain was removed on day two and patient started mobilization. With twenty-four weeks follow up, patient has symptomatically improved, wound is clean and dry. MR imaging was done at follow up shows no recurrence and an intact dura with no CSF leak (Figure 7).
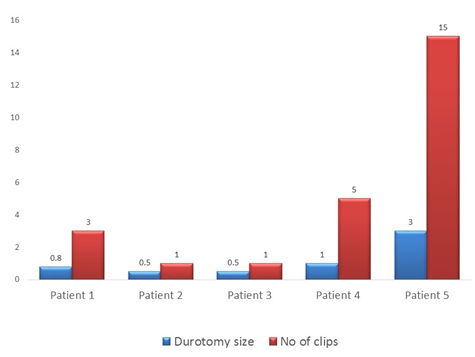
Chart 2: Bar diagram shows the size of Dural tear and number of Titanium clips applied.
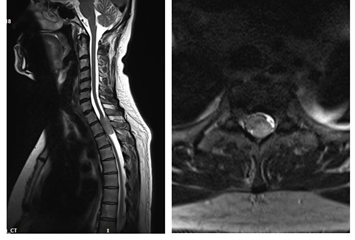
Figure 1: MRI sagittal and axial images of cervico-dorsal spine shows hypointense lesion compressing cord from D1-D3.
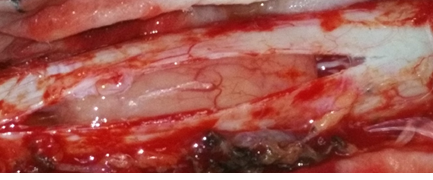
Figure 2: Intraoperative image shows durotomy exposing the intradural mass lesion.
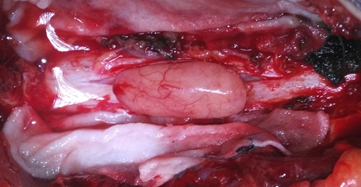
Figure 3: Intraoperative image shows pinkish smooth mass lesion removed from the dural sac.

Figure 4: Intraoperative image shows durotomy closure using titanium clips.

Figure 5: Immediate Post-operative MRI image shows fluid collection at the surgical site with herniation of spinal cord.
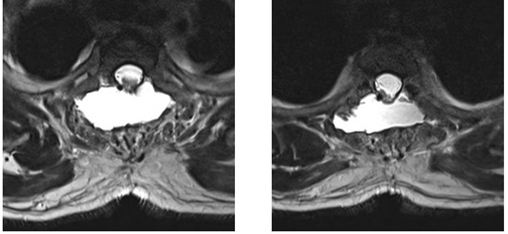
Figure 6: Immediate Post-operative MRI image shows Pseudo meningocele with cord herniation.
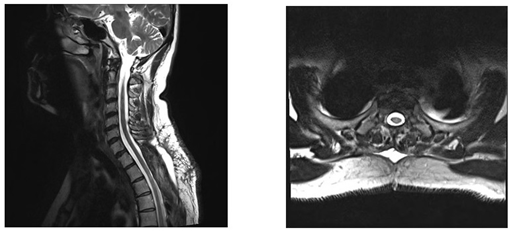
Figure 7: Follow up MRI image after revision surgery shows intact dura without any fluid collection at the surgical site.
4. Discussion
The success rate of non-penetrating titanium clips in Dural repair with this study is around 80%. All cases with size of Dural opening up to 1 cm had excellent outcome, without any complications and a smooth post-operative period. Outcome was poor in a case with 3 cm Dural opening. Intermittent episodes of cough was present post operatively in this patient alone. This study questions the usage of titanium clips in patients with a large Dural opening. Also, the role of Titanium clips in patients with history of chronic cough is not yet clear. In terms of time required for application of the clips, the average time required for application per clip is 10 seconds. One of the great advantages of this clips is they can be used with ease in minimally invasive surgeries and microdiscectomies, avoiding the need for further exposure. In terms of number of clips used, we used clips with average spacing of 2 to 3 mm between clips and got patent closure. Valsalva maneuver to be practiced in all Dural primary repairs to check patency of the repair and to define further post op care [7]. A tight sub fascial closure [8] is must in all cases of Dural repair. The role of drains in Dural repair surgeries is still under debate, in this study we used active suction drain with low pressure and obtained good results. A smooth awakening from anesthesia is to be performed in all cases, as violent awakening results in failure of the primary repair. Patients position after surgery is based on Bernoulli’s theory, keeping the repair site at higher level [9]. If the size of the tear is less than 1 cm and intra op Valsalva shows patent repair then we kept all our patients in neutral position. Absolute bed rest was given in all patients in the first 24 hours. Then gradual mobilization is started. Initially patients were made to sit up with head end elevation of 60 degrees. Observed for 4 hours and if tolerating, were subjected to trials to stand. If tolerating, they were made to ambulate. If they are not tolerating, then bed rest was continued for 24 hours and again mobilized in a stepwise manner [10]. Drain was removed when the collection is less than 50 ml. If the drain is more than 50 ml after 72 hours, leakage from wound site and patient having clinical symptoms of CSF headache, a re exploration surgery is planned [7]. One of our case with persistent leak after 72 hours with signs of neurological deterioration, was re operated. Post op MRI is recommended in all cases with persistent leak. Metal artifacts by titanium clips is minimal. A thorough planning is required in re exploration. Multiple modalities of Dural repair should be available. Watchful exploration of the dura is done to look for secondary tears or extension of primary tear. Chances of root or spinal cord herniation is high and it should be gently relocated.
The Non-Penetrating Titanium clips designed by Wolff Kirsch are initially used for application in vascular injuries and later extended its usage in Dural closures. FDA has approved its usage in Dural closures in the year 1996 [11]. Non-penetrating Titanium clips give tighter closures without producing any suture holes [12]. They are easy to apply and consume less time for application. With the advancement of minimally invasive surgeries, role of titanium clips is much of a value. In these surgeries, there is less need for further dissection and clips can be easily applied in a narrow space. Titanium clips produce less foreign body reactions and have a low risk of intradural adhesions. Timothy et al. [13], studied the use of Titanium clips in their fifty eight patients involving durotomies for intradural lesions. They found the advantages of the clips in ease of usage, speed, use in narrow areas and MRI compatibility. They recommend titanium clips usage in minimally invasive spine surgeries. Failure rate in their study was 13.7%, in which three cases required re-exploration. Ito et al. [11], in their study comparing titanium clips and sutures found that leakage pressure of non-penetrating titanium clip was 15.7 times greater than suture group. In their study, clips were applied with a 2mm spacing between them. Leppaniemi et al. [14], study found that 88% Dural repair time saved with nonpenetrating titanium clips compared with sutures. Fang et al. [2], in their study recommend <3mm distance between two sutures/ clips with each 1mm apart. Faulkner et al. [15], in their experimental study in calf spine comparing monofilament suture, Braided suture and Medium sized titanium clips found the mean time for repair were 250, 255 & 111 seconds respectively. They concluded that nonpenetrating clips are stronger than conventional suture techniques and they are not in favor of application of sealants over primary repair. Palmer et al. [16], in their experimental study in canine dura, found fewer incidence of inflammation, foreign body reaction and Dural adhesions. Levy et al. [17], stated the disadvantages of titanium clips including dislodgement of clips, difficulty in reapplication and Dural lacerations. Kaufman et al. [18], in their 27 paediatric cases managed with nonpenetrating titanium clips found no interference with CT or MR imaging in post op follow up. They limited the use of titanium clips to those cases with small Dural opening < 2cm and suggested the use of sutures for longer Dural openings, since there is no significant advantage of clips in those cases. Kiyoshi Ito et al. [19], evaluated the metallic artifacts produced by Non-penetrating titanium clips in follow up imaging of seventeen intradural tumor excision cases. Visualization of both the spinal cord and paraspinal muscles were of very good quality. The Dural closure using Non-penetrating titanium clips did not alter the quality of follow up imaging. The size of the titanium clips was found to be 200% larger than their original size. Glenn et al. [20], in their study on 53 patients who had undergone Dural closure with Titanium clips, suggested Non-penetrating titanium clips an additional method of primary Dural repair. Cheng et al. [21], in their experience with Non-penetrating Titanium clips in durotomy repair in a case of MIS TLIF, found it to be effective in limited tubular spaces. Kirsch et al. [22], stated non-penetrating clips an excellent instrument for effective and rapid Dural closure.
5. Conclusion
Non-penetrating titanium clips produce complete Dural closure with no suture holes. Usage in patients with history of chronic cough, constipation and urinary retention is debatable. We conclude non-penetrating clips can be used as an alternative for conventional sutures in durotomy repair. Further long series of studies are needed to find the efficacy of Non-penetrating titanium clips in longer durotomy repairs.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. No financial aid or funding received.
References
- Cammisa FP Jr, Girardi FP, Sangani PK. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 25 (2000): 2663-2667.
- Zhao Fang, Rong Tian, Yu-Tao Jia. Treatment of cerebrospinal fluid leak after spine surgery., Chinese Journal of Traumatology 20 (2017): 81e83.
- Black P. Cerebrospinal fluid leaks following spinal or posterior fossa surgery: use of fat grafts for prevention and repair. Neurosurg Focus 9 (2000): e.
- Rudrashish Haldar, Ankur Khandelwal, Devendra Gupta, et al. Valsalva maneuver: Its implications in clinical neurosurgery. Neurology India 64 (2016).
- Marcelo Galarza, Roberto Gazzeri, Raúl Alfaro, et al. Evaluation and management of small dural tears in primary lumbar spinal decompression and discectomy surgery. Journal of Clinical Neuroscience 11 (2018).
- Pradeep K Narotam, Sunil Jose, et al. Collagen Matrix (DuraGen) in Dural Repair: Analysis of a New Modified Technique. SPINE 29 (2004): 2861-2867.
- Wolff S, Kheirredinea W, Riouallona G. Surgical dural tears: Prevalence and updated management protocol based on 1359 lumbar vertebra interventions. Orthopaedics & Traumatology: Surgery & Research 98 (2012): 879-886.
- Jeon SH, Lee SH, Tsang YS. Watertight sealing without lumbar drainage for incidental ventral dural defect in transthoracic spine surgery: a retrospective review of 53 cases. Clin Spine Surg (2016).
- Menon SK, Onyia CU. A short review on a complication of lumbar spine surgery: CSF leak. Clin Neurol Neurosurg 139 (2015): 248e251.
- Mustafa h Khan, Jeffery rihn, Garen steele, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery a review of 3,183 consecutive degenerative lumbar cases. spine 31 (2006): 2609-2613.
- Kiyoshi Ito, Tatsuro Aoyama, Tetsuyoshi Horiuchi, et al. Utility of nonpenetrating titanium clips for dural closure during spinal surgery to prevent postoperative cerebrospinal fluid leakage. J Neurosurg Spine 23 (2015): 812-819.
- Gaskill DM, Stewart S, Kirsch WM, et al. Sutureless vasovasostomy: new technique using experimental microclip in rat model. Urology 40 (1992): 191-194.
- Timothy J , Hanna SJ , Furtado N. The use of titanium non-penetrating clips to close the spinal dura. Br J Neurosurg 21 (2007): 268-271 .
- Leppäniemi A, Wherry D, Pikoulis E, et al. Arterial and venous repair with vascular clips: comparison with suture closure. J Vasc Surg 26 (1997): 24-28.
- Nathan D Faulkner, Michael A Finn, Paul A Anderson. Hydrostatic Comparison of Nonpenetrating Titanium Clips Versus Conventional Suture for Repair of Spinal Durotomies., Spine 37 (2012): E535- E539.
- Palmer SJ, Kirsch WM, Zhu YH. Dural closure with nonpenetrating clips prevents meningoneural adhesions: an experimental study in dogs. Neurosurgery 45 (1999): 875-882.
- Levy DI, Sonntag VKH. Titanium dural clip testing. J Neurosurg 81 (1994): 947- 949.
- Kaufman BA, Matthews AE, Zwienenberg-Lee M. Spinal dural closure with nonpenetrating titanium clips in pediatric neurosurgery. J Neurosurg Pediatr 6 (2010): 359- 363.
- Kiyoshi Ito, Tatsuya Seguchi, Takuya Nakamura. Evaluation of Metallic Artifacts Caused by Nonpenetrating Titanium Clips in Postoperative Neuroimaging., WORLD NEUROSURGERY 96 (2016): 16-22.
- Chad A Glenn, Cordell M Baker, BS Joshua D Burks, et al. Dural Closure in Confined Spaces of the Skull Base with Nonpenetrating Titanium Clips. Operative neurosurgery (2017).
- Yen Po Cheng, Ping Yi Lin, Abel Po Hao Huang, Chun Yuan Cheng. Durotomy repair in minimally invasive transforaminal lumbar interbody fusion by nonpenetrating clips. Surgical Neurology International 5 (2014): 36.
- Wolff K, Justin B J. Applications of the AnastoClip® for Neurosurgical Interventions. Tech Neurosurg Neurol 1 (2018).


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 