Subclinical Vascular Impairment in Newly Diagnosed Asymptomatic Patients with Type-2 Diabetes Mellitus: Emphasis on Coronary Plaque Features
Sine Skov MD1, Lotte Grumsen MD1, Gulia Faizi MD1, Jeppe Gram MD, PhD1, Niels Peter Rønnow Sand MD, PhD1, Monija Mrgan MD, PhD1*
1Department Physician, Ph.D, Department of Cardiology, Southwest Jutland Hospital, Denmark.
*Corresponding author: Monija Mrgan MD, PhD, Department Physician, Ph.D, Department of Cardiology, Southwest Jutland Hospital, Denmark.
Received: 30 September 2025; Accepted: 06 October 2025; Published: 16 October 2025
Article Information
Citation: Sine Skov MD, Lotte Grumsen MD, Gulia Faizi MD, Jeppe Gram MD, PhD, Niels Peter Rønnow Sand MD, PhD, Monija Mrgan MD, PhD. Subclinical Vascular Impairment in Newly Diagnosed Asymptomatic Patients with Type-2 Diabetes Mellitus: Emphasis on Coronary Plaque Features. Archives of Internal Medicine Research. 8 (2025): 317-323.
View / Download Pdf Share at FacebookAbstract
Purpose:
To assess the presence of subclinical atherosclerosis in asymptomatic patients with newly diagnosed (<1 year) type-2 diabetes mellitus (T2DM) without known cardiovascular disease (CVD) with special emphasis on coronary artery disease.
Methods:
Non-contrast cardiac CT and coronary artery calcium scoring (CAC) was performed in 115 patients. A subset of the population (77 %) underwent contrast enhanced coronary CT angiography (CTA). Advanced coronary plaque analysis was performed using a validated semi-automated program (AutoPlaque). Measurements of intima media thickness (IMT) by carotid ultrasound, arterial stiffness by pulse wave analysis (PWA), occurrence of peripheral artery disease (PAD) by ankle brachial index (ABI) and vascular leakage by albumin creatinine ratio (ACR) were performed in all patients. Thresholds for sifgns of atherosclerosis were: IMT>0.9 mm; ABI<0.9 and ACR>30 mg/g.
Results:
Patients with CAC >0 was significantly older (61 vs 52 y, p<0,05), were more frequently men (38 vs. 35, p<0,05), had higher PWA (8,9 vs 7,9 m/s, p<0,01) and IMT (0,8 vs 0,7 mm, p=0,01). LD-NCP ratio increased with higher total plaque volume (TPV) in patients with CAC (τ = 0.45, p <0.05). A high amount of LD-NCP was significantly associated with higher D-dimer (p=0,011) and higher LDL cholesterol (p=0,003). Sign of PAD and increased ACR was present in 8% of the patients of whom all had CAC>0.
Conclusion:
At the time of diagnosis of T2DM more than 60 % of asymptomatic patients present with signs of subclinical atherosclerosis. Coronary plaque composition in these patients displays features associated with an increased vulnerability.
Keywords
Type 2 diabetes; cardiac CT; remote vessel disease; atherosclerosis; pulsed wave analysis; intima media thickness
Article Details
Introduction
Worldwide coronary artery disease (CAD) is one of the leading causes of morbidity and mortality. It has already been established that T2DM increases the risk of developing CAD and a poor long-term prognosis [1-3]. In Denmark it is indicated to treat diabetics no matter duration with cholesterol lowering drugs to reach a goal of LDL ≤ 1.8 mmol/L to prevent CAD [1]. The main part of already conducted studies relied on populations of diabetic patients with long diabetes duration and/or known cardiovascular disease (CVD). This study examines presence of subclinical atherosclerosis and plaque composition in patients with early stage (<1 year) T2DM. So far, any research involving newly diagnosed T2DM patients and CAD remains scarce, a search made on the 20th of September 2025, showed only 15 results where only two articles were relevant and none with the knowledge on TVP, d-dimer, and LD-NCP. “Vascular newly diagnosed asymptomatic type-2 diabetes”. The above mentioned can be related to INTEN-CT, whether or not treatment is indicated.
Methods
Population
From March 2014 to August 2016, a total of 213 adult individuals diagnosed with T2DM (hemoglobinA1c >47mmol/mol and plasma glucose >7mmol/L) within the last year were identified via general practitioners or outpatient clinics in Region South of Denmark, and invited by letter to participate in the study. A total of 115 (54 %) of patients agreed to participate, with an exclusion of 3, therefore a total of 112. A detailed description of patient cohort exclusions criteria and demographic data have been published previously [2]. Data on this full population and data regarding PWA and ABI has not been published, a demographic table can be viewed in table 1.
Table 1: Clinical characteristics of the study populations.
|
All participants |
Participants with |
Participants with |
p-value |
|
|
Demographics |
||||
|
Age, years |
56.1 (11.2) |
60.9 (8.6) |
52.3 (11.6) |
0 |
|
Male |
74 (66) |
38 (76) |
35 (56) |
0.045 |
|
Risk factors |
||||
|
Ever smoker |
63 (56) |
31 (62) |
32 (52) |
0.271 |
|
Body mass index, kg/m2 |
31.1 (5.5) |
29.8 (4.0) |
32.3 (6.3) |
0.02 |
|
24-hours systolic blood pressure, mmHg |
131.7 (11.5) |
131.4 (11.3) |
131.8 (12.0) |
0.864 |
|
24-hours diastolic blood pressure, mmHg |
76.2 (71.8; 80.9) |
75.5 (70.3; 80.8) |
77.7 (71.9; 81.3) |
0.433 |
|
Laboratory findings |
||||
|
Total cholesterol, mmol/L |
4.4 (0.9) |
4.3 (1.0) |
4.5 (0.8) |
0.237 |
|
Low-density lipoprotein, mmol/L |
2.5 (0.8) |
2.3 (0.7) |
2.6 (0.8) |
0.066 |
|
High-density lipoprotein, mmol/L |
1.2 (0.3) |
1.1 (0.3) |
1.2 (0.3) |
0.546 |
|
Triglycerides, mmol/L |
1.7 (1.3; 2.5) |
1.6 (1.3; 2.5) |
1.8 (1.3; 2.5) |
0.686 |
|
Fasting glucose, mmol/L |
7.5 (7.0; 8.3) |
7.35 (6.8; 8.0) |
7.6 (7.0; 8.6) |
0.063 |
|
Haemoglobin A1c, mmol/mol |
46.0 (42.5; 51.5) |
45.0 (41.0; 49.0) |
47.0 (43.0; 54.0) |
0.059 |
|
Serum creatinine, umol/L |
74.8 (13.1) |
77.2 (13.4) |
70.2 (5.7) |
0.072 |
|
eGFR, mL/min |
88.3 (18.2) |
86.8 (17.4) |
88.9 (18.3) |
0.522 |
|
Urine Albumine Creatinin Ratio, mg/g |
8.0 (5.0; 13.0) |
6.0 (4.5; 15.0) |
8.0 (5.0; 10.0) |
0.626 |
Values are mean (SD), n (%) or median (IQR). eGFR: estimated glomerular filtration rate.
The study was approved by the Regional Scientific Ethical Committee for Southern Denmark (S20140137) and by the Danish data Protection Agency (2008-58-0035), and was conducted in accordance with the Declaration of Helsinki.The study was registered at ClinicalTrials.gov ID: NCT03022344 and protocol ID: 44110
Cardiac computed tomography
Image acquisition was performed in accordance with guidelines defined by the Society of Cardiovascular Computed Tomography. Danish guidelines were followed for heart rate, sublingual nitroglycerine, Agaston socre, contrast, technical stetting and reconstruction processing.
Coronary artery calcification
All patients underwent a standard non-contrast scan, with a reference mAs of 50 for assessment of coronary artery calcifications (CACs) by the Agatston score CAC was assessed by summing up the scores from all foci in the coronary arteries, using dedicated software (Syngo Calcium scoring, (Siemens Healthcare)). Patients were classified as having atherosclerosis, if CAC >0 U.
Data analyses and plaque quantification
Reconstructed CCTA images were transferred to a workstation, syngo.via (Siemens Healthcare) for post processing. One experienced CT cardiologist, blinded to all clinical data, analysed the CT datasets, and one trained reader performed plaque analysis using validated semi-automated software (AutoPlaque, version 2.0, Cedars-Sinai Medical Center, Los Angeles, CA, USA). A detailed description of CT acquisition and plaque analysis has been published previously.
Ultrasound of carotids
Ultrasound of the carotid arteries was performed using a Philips iE33 High resolution, B-mode cardiovascular system (Philips Medical System) using a linear array transducer, L11-3 with an extended operating frequency range up to 11 MHz and 288 elements. The right and left common carotid arteries were systematically reviewed both horizontally and longitudinally three times at three different angels (0º, 90º and 180º). The Bulbus was reviewed at one angle three times. Three cardiac cycles of the common carotid artery and bulb, respectively, were digitally acquired for offline analysis. Intima-media thickness (IMT) was analysed via Excelera using a semi-automatic edge-detection software package (Q-LAB, version 8.0 with software plug.in IMT). IMT was determined at the far wall in each recording during the end-diastole and measured at 3 R-spikes. The largest value was used. IMT >0.9 mm was considered a sign of atherosclerosis. An average IMT was calculated for all sites and angles. A single reader, MM, blinded to other data, analysed all ultrasound data. Twenty (17.8 %) of the ultrasound examinations were re-analysed, in order to estimate the intra-observer variability.
Pulse wave analysis
PWA is a method for assessment of arterial stiffness which can indicate aterisclerosis. Oscillometry measures small oscillations in the blood pressure via a cuff around the a. brachialis as when determining blood pressure using electronic blood pressure monitor. The cuff is inflated corresponding to the diastolic blood pressure, and the changing amplitude of the oscillations is recorded as an expression of the pulse wave. In our study, PWA-Mobil-O-Graph device (IEM, Stolberg, Germany) is used. Patients rest for 10 minutes before measuring, fasting and abstinence from alcohol and tobacco 3 hours before measuring. The measurements are made for a total of 60 minutes where the patient sits down for 30 minutes and lies down for 30 minutes in a quiet room.
Ankle brachial index
In all patients the ankle brachial index (ABI) was measured: after 10 min of rest the systolic blood pressure was measured twice in both arms with the person in the supine position. Systolic blood pressures were measured by doppler ultrasonography, twice in the a. dorsalis pedis and twice in the a. tibialis posterior in both legs. The right and left ABI values were determined by dividing the average of the two highest ankle blood pressures of each leg, respectively, by the average of the two highest arm blood pressures. A ratio of <0.9 were considered a sign Start of peripheral arterial disease. Doppler ultrasonography was performed by one trained person.
Statistical analysis
Continuous variables were plotted as empirical histograms and quantile-quantile plots, and distributions were visually inspected. Summary statistics were presented as means and standard deviations (SD) if continuous variables were normally distributed, or as median and interquartile ranges (IQR) if continuous variables were skewed distributed. Dichotomous data were presented by frequencies and corresponding percentages. Group comparisons were done with Student’s paired t-test for matched data or Student’s unpaired t-test for independent data for normally distributed variables, non-parametric Wilcoxon rank-sum test for skewed distribution variables and the chi-squared for dichotomous variables. Intra-observer variability of plaque characteristics was analyzed using the paired t-test.
The statistical software Stata/IC version 13-15 (StataCorp LP, College Station, TX, USA) was used for all analyses. In all cases two-sided p-values <0.05 were considered statistically significant.
Results
CAC was performed in 115 patients, 3 were excluded.
Therefore, the study sample comprised a total of 112 patients (66% males) with newly diagnosed T2DM without known cardiovascular disease. Clinical characteristics are present in table 2.
Peripheral artery disease (PAD) was meassured by ankle brachial index (ABI) and vascular leakage by albumin creatinine ratio (ACR).
Patients with CAC >0 was significantly older (61 vs 52 y, p<0.05), were more frequently men (38 vs. 35, p<0.05), compared to patients with CAC=0. There was no significant difference regarding other clinical characteristics.
Due to exclusion criteria, 24 patients (54 % male) solely underwent a non-contrast cardiac CT scan. Distribution of CAC, n (%), in the non-contrast cardiac CT group was: CAC of zero: 8 (33); CAC 1-400: 10 (42); CAC above 400: 6 (25). Distribution of CAC, n (%), in the contrast enhanced coronary CTA group was: CAC of zero: 38 (43); CAC 1-400: 39 (44); CAC above 400: 11 (13). No differences in risk factors between these groups were observed.
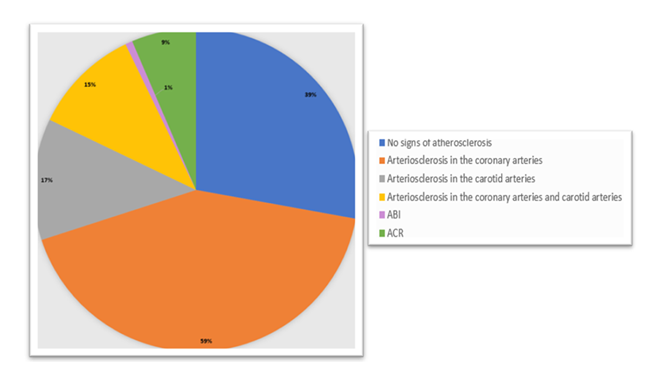
Overall, 66 (59 %) patients had coronary atherosclerosis. Mean (SD) CAC score was 179 U (384 U) and 15 % of all patients had a CAC > 400.
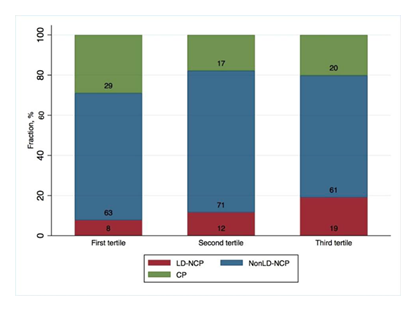
A total of 50 (57%) patients had coronary plaques. Three patients had significant coronary stenosis; two had coronary plaques and CAC=0. In 32 (36.4%) patients, coronary plaques were present in more than one coronary artery. In the group of 88 patients eligible for contrast enhanced cardiac CT it was found that the LD-NCP ratio increased with higher TPV in patients with CAC (τ = 0.45, p <0.05), see figure 2. There were no differences in BMI and radiation doses between tertiles of plaque volumes. Patients with high LD-NCP (third tertile) had significantly higher d-dimer as well as higher LDL cholesterol, compared to patients with low LD-NCP (first tertile).
IMT was 0.7 mm (0.2), mean (SD). ABI was 1.2 (0.1), mean (SD), and ACR was 8.0 mg/g (5.0; 13.0), median (IQR). PWA was 8.3 m/s (1.4), mean (SD). Patients with CAC > 0 vs CAC=0 had significantly higher PWA (8.9 vs 7.9 m/s, p<0.01) and IMT (0.8 vs 0.7 mm, p=0.01) compared to patient with CAC = 0. Sign of PAD and increased ACR was present in 10 % of the patients of whom all had CAC>0, though the association was not significant. No difference in ABI and ACR between CAC>0 and CAC =0 was observed.
In figure 2, a circle diagram, illustrates our findings, that 59% of asymptomatic newly diagnosed T2DM showed signs of arteriosclerosis in the coronary arteries, only 39% showed no signs of arteriosclerosis. 15% had both arteriosclerosis in the carotid and coronary arteries, and 17 % only had arteriosclerosis in the coronary arteries.
Discussion
In this study, we assessed the presence of subclinical atherosclerosis in asymptomatic patients with newly diagnosed T2DM by five different non-invasive methods. The major finding of this study was that more than 60 % of asymptomatic patients with a new diagnosis of T2DM present signs of subclinical arteriosclerosis. Furthermore, we found that coronary plaque composition in these patients displays features associated with an increased vulnerability.
The strenuous work in obtaining a population of newly diagnosed asymptomatic T2DM individuals, in whom we had only very sparse information on subclinical cardiovascular manifestations, should be mentioned, table 1 with demographics.
In asymptomatic patients with newly diagnosed T2DM we demonstrated:
- That 59 % had coronary arteriosclerosis.
- That 57% had coronary plaques.
- Coronary plaque composition displays features associated with an increased vulnerability.
- Patients with sign of PAD and increased ACR had also coronary atherosclerosis.
- The majority of the patients with arteriosclerosis in carotid artery also had coronary arteriosclerosis.
The occurrence of CAC implies the presence of CAD beyond cardiovascular risk factors or symptoms, mirrors coronary plaque burden, is associated with CVD progression and predicts future cardiovascular outcomes. In general, T2DM patients and non-diabetic individuals who do not have any CAC have similar mortality rates. However, patients with T2DM and CAC have a higher mortality risk compared to non-diabetic patients with CAC. We found that 59% of patients had coronary atherosclerosis already at time of diagnosis. Our data on CAC frequency is comparable to the data by Scholte et al (20), in which CAC was demonstrated in 56 % despite a higher frequency of males (74 %) and a longer diabetes duration of approximately 110 months.
In this study, we demonstrated, by figure 2, a positive association between CAC and the carotid arteries. Subclinical atherosclerotic manifestations in asymptomatic patients with newly diagnosed T2DM. Almost all patients in this study had a normal ABI (only one patient had ABI <0.9) indicating that patients with newly diagnosed T2DM seldom possess impaired peripheral arterial circulation. This finding is similar to findings in Danish non-diabetic asymptomatic individuals [8]. In contrast, we found that the existence of subclinical arteriosclerotic manifestations were more frequent in the carotids (by IMT) and in the aorta (by PWA). In addition, we found that patients with CAC>0 more often had remote vessel impairment as measured by a higher PWA and an increased IMT as compared to patients without CAC. IMT is a marker for structural morphologic changes in the arterial vessel wall and reflect histopathological verified arteriosclerosis [9]. PWA reflects arterial stiffness. It is a marker of the severity and prognosis of vascular disease as well. Therefore, it is usable in diagnosing high-risk patients at the stage where clinical intervention can prevent further disease development. Additionally, several studies have shown that patients with T2DM have higher PWA values and higher IMT compared to controls [5-7]. In the populations of the aforementioned studies the patients had T2DM for a lengthier duration, opposed to this study which exclusively included newly diagnosed T2DM patients. It is well established through previous studies that age, duration of diabetes, BMI, hypertension, and hyperlipidemia increase both IMT and PWA [10-12]. Patients in our study have already been in initial therapy for T2DM and some of them in antihypertensive and lipid-lowering treatment, which potentially might have confounded the relationship between the obtained values (blood pressure, lipid profiles, and HbA1c), IMT and PWA. The information on associations between coronary and remote vessel pathologies in the very early stages is new and support speculations on T2DM as being central for induction of impaired arterial circulation and as a cause of further deterioration of the cardiovascular system.
A previous study by Mrgan et al. suggested that patients in the early stages of T2DM had a significantly higher prevalence of the LD-NCP component compared to controls [2]. Additionally, the study showed, that the LD-NCP ratio increased with higher total plaque volumes in newly diagnosed T2DM, which did not apply for the healthy controls. The findings were confirmed, with a larger population added to the former. Indicating, in figure 1, that LD-NCP increases with higher TPV at an early stage of T2DM and thereby leaving the patients with a more vulnerable plaque morphology already at the time of diagnosis. Indeed, previous studies has shown that LD-NCP is directly associated to the risk of developing acute myocardial infarction (AMI) [14,15]. It has previously been established that LD-NCP is more strongly related to impaired coronary flow compared to calcified plaque (CP) [16]. Supporting this, Mrgan et al. found that flow impairment measured by fractional flow reserve - computed tomography (FFRCT) was significantly associated with higher LD-NCP volumes [17]. A previous study based on intravascular ultrasound found a more lipid-rich coronary plaque content in patients suffering AMI [18]. The recent SCOT-HEART trial also supports these findings, concluding that low-attenuation plaque burden is the strongest predictor of both fatal and non-fatal AMI [19].
The absolute values of total plaque volume were divided into tertiles with the following values given as median (IQR): first tertile: 12.2 mm3 (7.3; 44.2), second tertile: 237.8 mm3 (139.6; 273.9) and third tertile: 718.9 mm3 (506.4; 829.9). CP: calcified plaque; LD-NCP: low-density non-calcified plaque; Non-LDNCP: non-low-density non-calcified plaque.
Figure 1: Ratio of coronary plaque components in relation to total plaque volume
Cardiovascular risk remains high in patients with T2DM. Early detection of subclinical vascular involvement and intensive medical risk factor control may be essential in the prevention of manifest CVD. Identification and treatment of patients at risk of developing adverse clinical outcomes have for years been based on screening for traditional risk factors. Characterisation of subclinical atherosclerosis seems challenging but also highly relevant. The findings in this study, compared to already existing evidence might lead to a debate whether prophylactic measurements must be taken to prevent cardiovascular morbidity and mortality among T2DM patients already at an early stage of diagnosis. The subject of offering ex. cardiac CT or carotid ultrasound to bigger populations remains up for discussion. Prophylactic statin treatment, which remains at debate with a meta-analysis involving 52,319 patients showing an average adherence to statin therapy at 65% [20], one could argue that early intervention with Sodium-glucose inhibitors or Gliptin-like-protein 1, or newly indicated weight loss drugs, which very well could effect atherosclerosis. Shah et al argues, that even though controlled prospective data to prove the efficacy of imaging-guided risk assessment lacks, a large amount of cohort studies and prospective data supports imaging-based risk valuation especially in intermediate-risk groups identified by ex. The Framingham Risk Score [21]. Shah et al suggests that the first line imaging modality should be non-invasive (carotid ultrasound), and if plaques or thickening of the intima media was found, no further screening is needed. Since only a minor portion of the patients in this study presented with an IMT>1mm, an additional cardiac CT could be provided for the rest to uncover CAC so the right, prophylactic measurements might be taken.
Limitations
The main limitation of this study is the small sample size of 115 newly diagnosed patients with T2DM. Furthermore, only 54% of the invited number patients agreed to participate. Those who agreed to participate might tend to be healthier than the non-responders, though this only highlights the importance of the significant findings. Additionally, 66% of the patients were males, which might also cause the data to be slightly skewed, though findings were significant.
The primary strength of the study was related to the use contemporary non-invasive techniques to obtain information on coronary morphology compared to other more established non-invasive measurements of vascular atherosclerosis.
In asymptomatic patients with newly diagnosed T2DM we demonstrated an early detection of arteriosclerosis in multiple vessels.
References
- Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383 (2014): 1068-1083.
- Mrgan M, Funck KL, Gaur S, et al. High burden of coronary atherosclerosis in patients with a new diagnosis of type 2 diabetes. Diabetes and Vascular Disease Research 14 (2017): 468-476.
- Rawshani A, Rawshani A, Franzén S, et al. Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N Engl J Med 376 (2017): 1407-1418.
- Dey D, Schuhbaeck A, Min JK, et al. Non-invasive measurement of coronary plaque from coronary CT angiography and its clinical implications. Expert Rev Cardiovasc Ther 11 (2013): 1067-1077.
- Taya N, Katakami N, Mita T, et al. Associations of continuous glucose monitoring-assessed glucose variability with intima-media thickness and ultrasonic tissue characteristics of the carotid arteries: a cross-sectional analysis in patients with type 2 diabetes. Cardiovasc Diabetol 20 (2021): 95.
- Resende L, Silva MAV, Resende JAM, et al. Comparison of pulse wave analysis parameters by oscillometry in hypertensive diabetic and nondiabetic patients in a Brazilian outpatient care. Medicine (Baltimore) 98 (2019): e18100.
- Solanki JD, Munshi HB, Mehta HB, et al. Central hemodynamics and arterial stiffness in Gujarati diabetics not receiving any antihypertensive: A case-control study based on oscillometric pulse wave analysis. J Family Med Prim Care 8 (2019): 1352-1358.
- Bjerrum IS, Sand NP, Poulsen MK, et al. Non-invasive assessments reveal that more than half of randomly selected middle-aged individuals have evidence of subclinical atherosclerosis: a DanRisk substudy. Int J Cardiovasc Imaging 29 (2013): 301-308.
- Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr 21 (2008): 93-111.
- Kawamori R, Yamasaki Y, Matsushima H, et al. Prevalence of carotid atherosclerosis in diabetic patients. Ultrasound high-resolution B-mode imaging on carotid arteries. Diabetes Care 15 (1992): 1290-1294.
- Taniwaki H, Kawagishi T, Emoto M, et al. Correlation between the intima-media thickness of the carotid artery and aortic pulse-wave velocity in patients with type 2 diabetes. Vessel wall properties in type 2 diabetes. Diabetes Care 22 (1999): 1851-1857.
- Megnien JL, Simon A, Valensi P, et al. Comparative effects of diabetes mellitus and hypertension on physical properties of human large arteries. J Am Coll Cardiol 20 (1992): 1562-1568.
- Karim R, Hodis HN, Detrano R, et al. Relation of Framingham risk score to subclinical atherosclerosis evaluated across three arterial sites. Am J Cardiol 102 (2008): 825-830.
- Motoyama S, Ito H, Sarai M, et al. Plaque Characterization by Coronary Computed Tomography Angiography and the Likelihood of Acute Coronary Events in Mid-Term Follow-Up. J Am Coll Cardiol 66 (2015): 337-346.
- Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol 54 (2009): 49-57.
- Gaur S, Øvrehus KA, Dey D, et al. Coronary plaque quantification and fractional flow reserve by coronary computed tomography angiography identify ischaemia-causing lesions. Eur Heart J 37 (2016): 1220-1227.
- Mrgan M, Nørgaard BL, Dey D, et al. Coronary flow impairment in asymptomatic patients with early stage type-2 diabetes: Detection by FFR(CT). Diab Vasc Dis Res 17 (2020): 1479164120958422.
- Amano T, Matsubara T, Uetani T, et al. Abnormal glucose regulation is associa+ted with lipid-rich coronary plaque: relationship to insulin resistance. JACC Cardiovasc Imaging 1 (2008): 39-45.
- Williams MC, Kwiecinski J, Doris M, et al. Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction: Results From the Multicenter SCOT-HEART Trial (Scottish Computed Tomography of the HEART). Circulation 141 (2020): 1452-1462.
- Kalia NK, Miller LG, Nasir K, et al. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis 185 (2006): 394-399.
- Shah PK. Screening Asymptomatic Subjects for Subclinical Atherosclerosis. Journal of the American College of Cardiology 56 (2010): 98-105.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 78.21%
Acceptance Rate: 78.21%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 