Surgical Management of Fractures in Vertebrae with Ankylosing Spondylosis- A Systematic Review with Newer Principles of Management
Suhasish Ray1*, D K Jha2, Bikramjit Gayen3
1Orthopaedic and Neurospine Surgeon, Woodlands Multispeciality Hospital, Spine Surgeon-Ramakrishna Mission Seva Pratisthan, Kolkata, India
2Professor, Department of Orthopaedic and Spine Surgery, Ramakrishna Mission Seva Pratisthan, Vivekananda Institute of Medical Sciences, Sishumangal Hospital, Kolkata, India
3Associate Professor, Department of Orthopaedics and Spine Surgery, Ramakrishnamission Seva Pratisthan, Vivekananda Institute of Medical Sciences, Kolkata, India
*Corresponding Author: Dr. Suhasish Ray, Doctorate in Orthospine Surgery, Orthopaedic and Neurospine Surgeon, Chief Spine Surgeon, Woodlands Multispeciality Hospital, Ramakrishna Mission Seva Pratisthan, Kolkata, India
Received: 19 July 2021; Accepted: 26 July 2021; Published: 16 August 2021
Article Information
Citation:
Suhasish Ray, Jha D K, Bikramjit Gayen. Surgical Management of Fractures in Vertebrae with Ankylosing Spondylosis- A Systematic Review with Newer Principles of Management. Journal of Spine Research and Surgery 3 (2021): 081-090.
View / Download Pdf Share at FacebookAbstract
Ankylosing Spondylosis denotes seronegative arthritis that causes inflammation and eventual fusion of the spine and the spinal joints. Involvement of peripheral joints and extraarticular manifestations. it includes-Ankylosing spondylitis (AS); (DISH); End-stage spondylosis multiform (EASM); Ossified posterior longitudinal ligament (OPLL). The prevalence ranges from 0.1 to 1 percent of the population, M>F, between15- 40 years; 95% share the genetic marker HLA-B27. Numerous bony changes to spine include-Intraosseous bone loss; erosion; sclerosis; fractures; extra osseous squaring; syndesmo and enthesophytes . Incidence of ASVF is 3.5 times more than in general people, 75% in the cervical spine followed by thoracic and lumbar spine. There is 11 times more chance of Spinal cord injury than in general. Mean age of fracture is 63.4 years. Treatment is challenging due to kyphosis, osteoporosis, associated comorbities and cardiopulmonary restrictions. Treatment goals are to reduce or prevent- inflammation, ankylosis, abnormal posture. The principle is to treat the fracture as long bone osteoporotic diaphyseal fracture. Apart from 360* fracture fixation with long construct, MIS surgery, other fracture managements in AS are deformity correction, laminectomy, laminoplasty, rhizotomy, neuromodulation. Complication rates are high,wound infections up to16%,pulmonary complications up to 63%, 23% mechanical complications among various reports. A standard guideline should exist for ASVF workup, management and complications appraisal.
Keywords
<p>Ankylosing Spondylytis, Vertebral Fracture, Anteropostero Fixation, Wedge Osteotomies, Significant Complication</p>
Article Details
1. Introduction
1.1 Vertebral fracture in ankylosing spondylosis
ASVF increases as the clinical consequences aggravates in spine deformities (hyperkyphosis) and complications are higher (Geusens et al. 2007). In a study in France VF in AS was found as high as 17% [1]. Low energy trauma predispose to ASVF due to change in matrix compositi-on, bone structure changes and ossification of the ligame-nts and surrounding soft tissues which become ossified. These fractures are hence unstable and susceptible to neurological deficit [2, 3]. Complication rates are high with 51% in AS patients, overall mortality rate within 3 months period being 17.7% in AS patients. 8-13% of patients have multilevel fractures. Spinal cord injury is 11 times more than in general population [4], The average age of fracture is 63.4 yrs [5] [Figure 1 and 2].
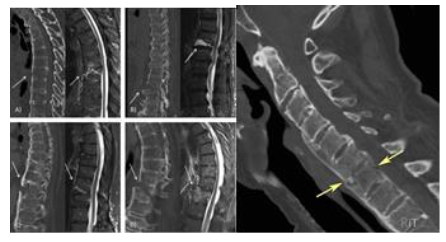
Figure 1 and 2: Preoperative Tomography and MRI showing acute vertebral fractures in AS vertebra.
1.2 Management of vertebral fractures in ankylosing spondylytis
The management would be divided into medical and surgical managements. Protected transfers are essential to prevent secondary neurological insult. Conservative methods, including immobilization by a Halo vest and prolonged bed- rest in traction or a collar, have been associated with a high rate of complications. With advances in care and surgical technique, there is a rising trend to surgery.
2. Methods
2.1 Conservative treatment
Conservative methods are chosen in46% people because of high anasthaetic risk, patients undergoing resusal to surgery [5]. There is a high risk of fracture displacement, worsening neurological status and a high rate of non union in conservative approach than in surgery [5]. Conservative care includes bed rest, roto rest bed, Halo traction, collars and braces for cervical fractures [6]. Customised body braces in kyphosis rarely maintain the preinjury contour ans neurological status. Regular follow up must be done not without downhill complications.
2.2 Surgical principles
ASVF is similar to long bone fracture where the principle is multilevel fixation. Elective operation is planned whereas in neurological deficit and displacement should be operated as an emergency.
2.3 Preoperative traction and positioning
5-20 lbs of skull traction is required for cervical displacement. The traction direction should be such to put it in prefracture alignment. Hyperextension should be avoided to avoid neurological deficit. Intubation is a difficulty, armoured tubes are mostly used and often awake fibre optic intubation. Intraoperative neuromonitoring is a must, Mayfield traction clamps or similar devices must be used for cervical spine and thoracic spine.
2.4 Anterior vs posterior vs circumferential stabilization
Anterior access is less traumatic, minimizes the risks of displacement during positioning, provide immediate stability and a greater surface area for bony fusion and has less incidence of postoperative infections. Anterior approach biomechanically is less stable due to vertebral body osteoporosis. Failure rate is 50% or more. Posteriorly spinal alignment is restored, stabilized well as the pedicle is the last part of the vertebra to be weakened, and broad decompression can be achieved of the neurological elements. Posterior fixation of multiple segments with autoharvested corticocancellous bones as graft give more biomechanical strength over anterior approach. Less muscle dissection, less bleeding, lower morbidity thus better wound healing and less chance of pseudarthrosis.
In addition, a fusion of the posterior elements may make localization of the anatomic landmarks difficult which can lead to pedicle fracture, neurodeficit, and vertebral artery injury. The anteroposterior or the circumferential approach is the current treatment of choice in cases with marked three column instability [7]. It is used in approximately 25% of ASVF cervical spine fractures. The primary indication of adding an anterior approach to posterior surgery is the presence of a persistent deformity, gap or displacement that is compromising the spinal cord following posterior instrumented reduction. Combined anteroposterior approach has longer surgical duran, higher anasthesia, higher morbidity, infection and hospital stay. We would recommend a combined approach for unstable fractures (translation, distraction, or angulation) and fractures with anterior gap. Whatever be the approach there must be increasing point of fixation, larger bore screw, augmented scrwes or dual core or convergent screws. Bivortical purchase is imperative.
2.5 Role of fusion in ASV fracture
Spinal fusion approaches for ASVF depend on the location of the fracture and can include posterior spinal fusion (PSF), anterior-posterior spinal fusion (APSF), and anterior spinal fusion (ASF). With the advent of new instrumentation and techniques, trends of approaches have changed [Figure 3 and 4].
2.6 Minimally invasive stabilization in ASVF
Minimally Invasive Fixation and Stabilization is to be used in ASVF with good neurological status, in DISH patients, less or no displacement and green stick fractures.limited operation scars , morbidity and postoperative status. It is approach of choice in old age, higher morbidities, greater risk of operation, lesser operation time, and earlier mobilization Krüger et al. [8] reported improved patient outcomes with closed reduction and MISS dorsal instrumentation [Table 3].
2.7 Osteotomies in deformity correction in ASV fracture
Extreme kyphosis in neglected fracture or pseudoarthrosis inability to look straight is sinequa non of osteotomy correction in ASVF before instrumentation and stabilization. Correction of thoracolumbar kyphotic deformities (TLKDs) in this patient population. With regard to options for the surgical treatment of TLKDs, the two best described techniques are the pedicle subtraction osteotomy also known as Closed wedge osteotomyand the opened wedge osteotomy (OWO) or a modified Smith—Petersen osteotomy (Figure 5 and Figure 6) [9-12].
2.8 Radiofrequency rhizotomy
Radio-frequency rhizotomy is a technique of pain modulation minimally invasive under IITV, contrast and nerve locator control. It uses heat to ablate and stop transmission of pain along the nerves. In chronic pain, sacroilitis, non surgically non displaced non Neurological deficit impinged and painful nerves. Avoids surgery, immediate pain control, early recovery, less need of pain meficines early rehabilitation and mobilization.
2.9 Outcome measures
Operative characteristics that were evaluated included surgical approach (PSF, APSF, and ASF). Major in-hospital complications,potentially long-term sequelae, implant status, post operative rehabilitation, and mobilization.
2.10 Statistical methods
Statistical analysis was performed using software SPSS IBM Ver. 22.0 criterios incomplementing surgical approach, complications, sex Race, Hospital stay. Analysis by Pearson's chi square d test, Analysis of Variance model was used for comparing age, hospital stay, total hospital costs between three surgical approaches. P< 0.05 was considered significant.
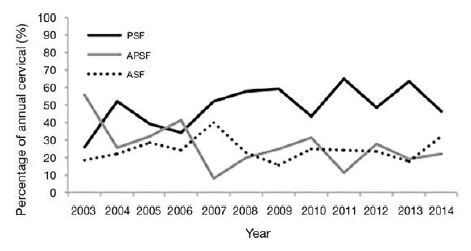
Figure 3: Multicentric data- Departments of Orthopaedic And Spine Surgery, Multicentre trends in cervical fusion from 2003-2014 in cervical spine fracture in AS vertebra. ASF=Anterior spinal fusion; PSF=Posterior Spinal Fusion; APSF=Antero-posterior Spinal Fusion.
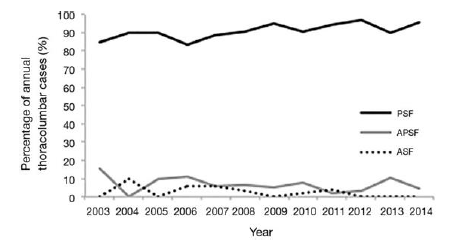
Figure 4: Multicentric Data - Departments of Orthopaedic And Spine Surgery, Multicentre trends in thoracolumbar fracture in AS vertebra. Multicentre trends in thoracolumbar fusion following TL fracture in AS vertebra.
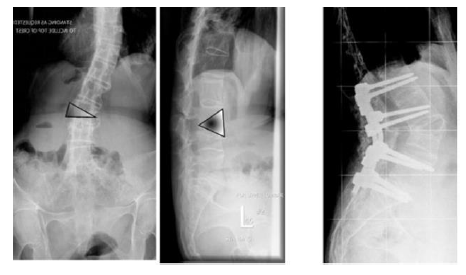
Figure 5: Asymmetrical spinal osteotomy consisting of pedicle subtraction and opening wedge osteotomy performed at L3, correcting both coronal and sagittal plan deformity.
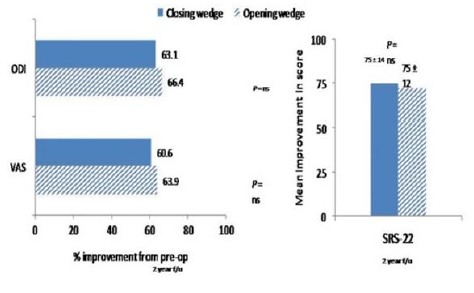
Figure 6: Comparison between Closing vs Opening wedge osteotomy. N=22 2 yrs f.u. Clinical outcomes in pain; ODI; quality of life (Arun et al 2011).
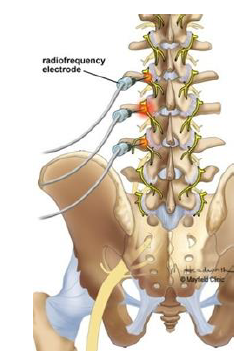
Figure 7: A heating current is passed through an electrode to destroy the medial branch of the sensory nerve to block the transmission of pain signals.
3. Result
Spinal fusion surgeries increased significantly (P<0.01). Cervical fusion results were non significant (P>0.05). However, there was a shift in the surgical approaches for cervical fractures. PSF increased by four fold while ASF surgeries increased 3.8 fold. Thoracolumbar fracture operation increased significantly (P<0.01) [Figure 3 and 4].
3.1 Complications
Compared to the healthy general population, the morbidity of ASVF is 3.5 times higher [13]. Commonest causes being acute post fracture stage and cardiopulmonary failure. Visceral injuries may occur, intrathoracic complications, aortic laceration and dissection has been multiply quoted. Loss of reduction, pseudarthrosis, nonunion and neurological deterioration have been reported after nonoperative treatment, which often leads to secondary surgery [14, 15]. A standardized workup before decision making, techniques, meticulous planning is required [Table 1 and 2].
Westerveld et al. noted 77.5% of fractures were located in the subaxial cervical spine [15]. Surgical treatment offered fusion strength, improvement in neurological conditions compared to non surgical management. For Thoracolumbar fracture fixation should be at least three levels above and below [16, 17]. MISS techniques are used for comorbities, old, frail and fast surgeries in ASVF. We argue MISS is advantageous in Thoracolumbar ASVF than open techniques especially long pedicle screw construct [19]. But this is not so in cervical spine where careful location and deformities have to be taken accounted for Werner et al. [20] stated posterior spinal fixation or anteroposterior spinal fixation is better in cervical spine because anterior spinal fixation is associated with higher failure rate. Though Anterior spinal fixation in cervical spine is still popular.
While APSF (55.6%) was most frequently used in 2003, PSF (46.7%) and ASF (31.7%) is popular in 2014. A higher prevalence of pulmonary disease is often seen in AS patients due to restrictive ankylosis of the thoracic cage [21, 22, 23]. There was significant association between both cervical ASVF and Thoracolumbar ASVF with highest rate of pulmonary complications. This significant findings will assist surgeons to choose a treatment protocol. Overall, complication risks ranged from 0 to 16.7% in the Closing Wedge Osteotomy group and from 0 to 23.6% in the Open Wedge Osteotomy group across the four studies [24-27]. The risks of dural tear in the closing versus the opening wedge groups. Paralytic ileus occurred consistently less often in the CWO (0 to 5.9%) versus the OWO (10.5 to 16.7%) The risk of superficial infection following CWO ranged from 2.0 to 8.3% comparedwith 0 to 1.5% followingOWO as reported by two studies [24-25]. Neurological injuries. Radiofrequency rhizotomy has complaints like neuritis, neuroma, increasing pain.
|
Post surgical Issues |
PSF (%) |
APSF (%) |
ASF (%) |
P value |
|
Cervical complications |
||||
|
Pulmonary |
30 |
45 |
35.5 |
0.01 |
|
Cervical spine related |
11.3 |
17.56 |
17.7 |
0.12 |
|
UTI |
12.8 |
6.1 |
9.7 |
0.12 |
|
Implant related |
2.3 |
6.1 |
3.2 |
0.14 |
|
Thromboembolic |
3.8 |
7.6 |
4 |
0.23 |
|
Cardiac |
13.2 |
10.7 |
8.1 |
0.32 |
|
Infectious |
5.3 |
3.8 |
7.3 |
0.49 |
|
Neurological |
0.38 |
0.76 |
0.81 |
0.62 |
|
Renal |
7.9 |
9.2 |
7.3 |
0.85 |
|
Incidental Durotomy |
0.75 |
0 |
0 |
0.99 |
|
Died |
7.1 |
9.9 |
13.7 |
0.11 |
|
Total complications |
50.4 |
58 |
53.2 |
0.36 |
|
Blood transfusion |
22.6 |
18.3 |
7.6 |
<0.01 |
Table 1: In house complication rates in different cervical spine fusion surgeries following ASVF. UTI=Urinary tract Infection.
|
Post surgical issue |
PSF (%) |
APSF (%) |
ASF (%) |
P value |
|
Pulmonary |
22.2 |
53.6 |
42.9 |
<0.01 |
|
ThLumbar spine rel. |
3.7 |
10.7 |
14.3 |
0.07 |
|
Infectious |
4.8 |
7.1 |
14.3 |
0.25 |
|
Implant related |
2.3 |
7.1 |
0 |
0.3 |
|
Thromboembolic |
3.4 |
7.1 |
0 |
0.44 |
|
UTI |
13.7 |
7.1 |
0 |
0.54 |
|
Neurological |
1.8 |
0 |
0 |
0.99 |
|
Cardiac |
16.2 |
14.3 |
14.3 |
0.99 |
|
Renal |
13.5 |
10.7 |
14.3 |
0.99 |
|
Incidental durotomy |
2.1 |
0 |
0 |
0.99 |
|
Died |
4.1 |
10.7 |
0 |
0.27 |
|
Total complications |
49.5 |
71.4 |
57.1 |
0.06 |
|
Blood transfusion |
28.1 |
21.4 |
14.3 |
0.67 |
Table 2: Inhouse complication rates in different thoracolumbar spine fusion surgeries following ASVF.
|
Parameter |
Average value (range) or % |
|
Age at Surgery (yrs) |
77 (52-88) |
|
Male |
45% |
|
ASA grade |
3 |
|
Low impact mechanism |
45% |
|
BMI |
34 (20.4-44.5) |
|
No. of segments fused/incorporated |
7(6-10) |
|
Operative time (minutes) |
227(79-449) |
|
Blood Loss (ml) |
251(25-900) |
|
Post operative LOS (days) |
14.4(4-60) |
|
Postoperative ODI |
21.5%(0-34%) |
|
Postoperative EQ-5D |
0.77(0.60-1.0) |
|
Follow up time (months) |
28(5-58) |
Table 3: Patient reported outcomes in MIS Surgeries for ASVF. ASA- American Society of Anasthesiologists; BMI- Body Mass Index; LOS- length of stay,; ODI- Oswestry Disability Index; EQ-5D-European Quality 5 D.
4. Conclusion
Fractures are a serious complication of AS and patients are more prone to develop neurological deficits. Most often, the underlying mechanism of injury is a small magnitude force. Nonsurgical treatment has largely been replaced by surgical treatment in view of the significant risk for secondary loss of reduction and neurological aggravation along with pulmonary and decubitus complications. It can be anterior, posterior (most commonly performed), or combined depending upon the location and pattern of injury. We found that surgical treatment has been growing in popularity for thoracolumbar fractures but staying consistent for cervical fractures in AS patients.
Patients subjected to Anteroposterior spinal fixation has higher cardiopulmonary complications. However, surgical management does not change the inherent complication rates and mortality risks which are largely dependent on the initial injury severity and comorbid conditions. Choice of osteotomy depended on predetermined patient characteristics (e.g., significant aortic atherosclerosis, severe osteoporosis, ossification of the longitudinal ligaments) in two studies resulting in potential confounding by indication in these cases [25-27]. The authors feel that the incidence of this complication in association with OWO was minimized due to a strong selection bias. It follows that in patients with clinically significant atherosclerosis, the CWO may be a more appropriate procedure.
Competing Interests
The authors declare that they have no competing interests.
Ethical Statement
Because the article is a multisource review, our study was exempt from institutional review board (IRB) approval.
References
- Sahuguet J mancini P; Lafforgue P, et al. THU0273 Prevalence of vertebral fractures in ankylosing spondylitis: a meta-analysis (2018).
- Lange U, Pape HC, Bastian L, et al. Operative management of cervical spine injuries in patients with bechterew’s disease. Unfallchirurg 108 (2005): 638.
- Surin VV. Fractures of the cervical spine in patients with ankylosing spondylitis. Acta Orthop Scand 51 (1980): 79-84.
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J 18 (2009): 145-156.
- Rustagi T, Drazin D, Oner C, et al. Fractures in spinal ankylosing disorders: A narrative review of disease and injury types, treatment techniques, and outcomes. J Orthop Trauma 31 (2017): S57-S74.
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J 18 (2009): 145-156.
- Woodruff FP, Dewing SB. Fracture of the cervical spine in patients with ankylosing spondylitis. Radiology 80 (1963): 17-21.
- Krüger A, Frink M, Oberkircher L, et al. Percutaneous dorsal instrumentation for thoracolumbar extension-distraction fractures in patients with ankylosing spinal disorders: a case series. Spine J 14 (2014): 2897-2904.
- Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976) 26 (2001): 2036-2043
- Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine (Phila Pa 1976) 26 (2001): E354-E360
- Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. J Bone Joint Surg Am 90 (2008): 2509-2520
- van Royen BJ, de Kleuver M, Slot GH. Polysegmental lumbar posterior wedge osteotomies for correction of kyphosis in ankylosing spondylitis. Eur Spine J 7 (1998): 104-110
- Lazennec JY, d’Astorg H, Rousseau MA. Cervical spine surgery in ankylosing spondylitis: Review and current concept. Orthop Traumatol Surg Res 101 (2015): 507-513.
- Yeoh D, Moffatt T, Karmani S. Good outcomes of percutaneous fixation of spinal fractures in ankylosing spinal disorders. Injury 45 (2014): 153-148.
- Robinson Y, Robinson AL, Olerud C. Complications and survival after long posterior instrumentation of cervical and cervicothoracic fractures related to ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976) 40 (2015): E227-E233.
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 18 (2009): 145-156.
- Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine 35 (2010): E458-E464.
- Werner BC, Samartzis D, Shen FH. Spinal Fractures in Patients With Ankylosing Spondylitis: Etiology, Diagnosis, and Management. J Am Acad Orthop Surg 24 (2016): 241-249.
- Krüger A, Frink M, Oberkircher L, et al. Percutaneous dorsal instrumentation for thoracolumbar extension-distraction fractures in patients with ankylosing spinal disorders: a case series. Spine J 14 (2014): 2897-2904.
- Lu ML, Tsai TT, Lai PL, et al. A retrospective study of treating thoracolumbar spine fractures in ankylosing spondylitis. Eur J Orthop Surg Traumatol 24 (2014): S117-S123.
- Werner BC, Samartzis D, Shen FH. Spinal Fractures in Patients With Ankylosing Spondylitis: Etiology, Diagnosis, and Management. J Am Acad Orthop Surg 24 (2016): 241-249.
- Kanathur N, Lee-Chiong T. Pulmonary manifestations of ankylosing spondylitis. Clin Chest Med 31 (2010): 547-554.
- Davies D. Lung fibrosis in ankylosing spondylitis. Thorax 1972;27:262.
- Arun R, Dabke HV, Mehdian H. Comparison of three types of lumbar osteotomy for ankylosing spondylitis: a case series and evolution of a safe technique for instrumented reduction. Eur Spine J 20 (2011): 2252-2260
- Chang KW, Chen YY, Lin CC, et al. Closing wedge osteotomy versus opening wedge osteotomy in ankylosing spondylitis with thoracolumbar kyphotic deformity. Spine (Phila Pa 1976) 30 (2005): 1584-1593
- Lazennec JY, Saillant G, Saidi K, et al. Surgery of the deformities in ankylosing spondylitis: our experience of lumbar osteotomies in 31 patients. Eur Spine J 6 (1997): 222-232
- Zhu Z,Wang X, Qian B, et al. Loss of correction in the treatment of thoracolumbar kyphosis secondary to ankylosing spondylitis: a comparison between Smith-Petersen osteotomies and pedicle subtraction osteotomy. J Spinal Disord Tech 25 (2012): 383-390.


 Impact Factor: * 3.123
Impact Factor: * 3.123 Acceptance Rate: 75.30%
Acceptance Rate: 75.30%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 