Effect of Thermocycling on Microhardness of Three CAD/CAM Provisional Materials
Mohammad Mahdi Tavajoh¹*, Farzan Younesi², Solmauz Eskandarion3
¹Dental department, Islamic Azad University Dental Branch, Tehran, Iran
²Department of Prosthodontics, Islamic Azad University Dental Branch, Tehran, Iran
³ Dental Materials Research Center, Islamic Azad University Dental Branch, Tehran, Iran
*Corresponding Author: Mohammad Mahdi Tavajoh, Dental department, Islamic Azad University Dental Branch, Tehran, Iran
Received: 20 August 2025; Accepted: 29 August 2025; Published: 03 September 2025
Article Information
Citation: Mohammad Mahdi Tavajoh, Farzan Younesi, Solmauz Eskandarion. Effect of Thermocycling on Microhardness of Three CAD/ CAM Provisional Materials. Dental Research and Oral Health. 8 (2025): 92-96.
View / Download Pdf Share at FacebookAbstract
Purpose: This study aimed to evaluate and compare the surface Microhardness of three CAD/CAM provisional restorative materials before and after Thermocycling.
Materials and Methods: In this in-vitro study, ten rectangular specimens (12 × 13 × 1.5 mm) were prepared from each of the following CAD/CAM provisional materials: Structur CAD (VOCO GmbH, Germany), Telio CAD (Ivoclar Vivadent, Liechtenstein), and Vita CAD Temp Monocolor (Vita Zahnfabrik, Germany). Surface Microhardness was measured using the Vickers test (20 g load for 10 seconds). All specimens underwent 5,000 thermal cycles between 5°C and 55°C to simulate six months of clinical service. Post-cycling Microhardness was measured, and results were statistically analyzed using Repeated Measures ANOVA.
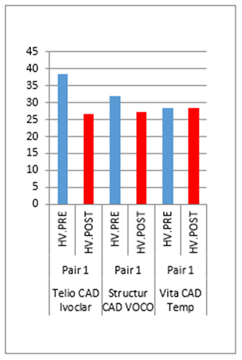
Results: Before Thermocycling, Telio CAD exhibited significantly higher Microhardness compared to Structur CAD and Vita CAD Temp (p < 0.05). After Thermocycling, differences among the three groups were not statistically significant (p > 0.05). Telio CAD and Structur CAD showed a significant decrease in surface Microhardness post-Thermocycling, while Vita CAD Temp did not show a statistically significant change.
Conclusion: Thermocycling affected the surface Microhardness of CAD/ CAM provisional materials differently. While initial hardness varied among the materials, all showed comparable performance after simulated clinical aging. For temporary restorations lasting up to 6 months, none of the tested materials demonstrated a clinically superior advantage in terms of surface microhardness.
Keywords
<p>Thermocycling, Surface Microhardness, CAD/CAM, Provisional Restoration, Vickers Test</p>
Article Details
Introduction
Mechanical deficiencies in temporary restorations, particularly in properties such as surface microhardness, can compromise the clinical success of fixed prosthodontic treatments. A reduction in surface microhardness can lead to increased surface roughness, which promotes plaque accumulation and may result in periodontal complications. Therefore, temporary restorations must possess adequate mechanical and biological properties to fulfill their critical functions. These include pulpal protection, prevention of supra-eruption or tooth tipping, maintenance of interproximal and occlusal stability, and serving as a prototype for the final prosthesis [1,2].
In recent years, the use of computer-aided design and computer-aided manufacturing (CAD/CAM) systems for fabricating provisional restorations has gained popularity. These systems offer advantages such as faster production and improved physical properties due to the use of pre-polymerized blocks and discs with a more homogeneous and durable internal structure [3]. Several studies have compared the mechanical behavior of CAD/CAM-based provisional materials to that of conventionally fabricated materials. CAD/CAM materials have generally shown better performance in terms of mechanical strength, surface hardness, and marginal adaptation [3-5].
Given the dynamic nature of the oral environment, temporary restorations must retain their mechanical integrity over time. To simulate clinical aging, thermocycling is commonly used in laboratory settings. This process mimics thermal stresses encountered in the oral cavity, enabling evaluation of material behavior under fluctuating temperatures [6]. However, not all studies assessing mechanical properties of provisional restorations have included thermocycling, despite evidence suggesting it may significantly influence results [7].
Some studies have reported increased surface roughness after thermocycling without affecting microhardness [8], while others have shown that thermocycling can either decrease or increase surface microhardness, depending on the material. These inconsistencies, along with the limited number of comparative studies focused on CAD/CAM provisional materials, highlight the need for further investigation.
Thus, the aim of this study was to evaluate and compare the surface microhardness of three commercially available CAD/CAM provisional restorative materials before and after thermocycling. The materials were selected based on availability and clinical use at the Islamic Azad University Dental Branch.
Materials and Methods
This in vitro experimental study evaluated the surface microhardness of three commercially available CAD/CAM provisional restorative materials: Structur CAD (VOCO GmbH, Germany), Telio CAD (Ivoclar Vivadent, Liechtenstein), and Vita CAD Temp Monocolor (VITA Zahnfabrik, Germany). Ten rectangular specimens were prepared from each material, measuring 12 mm × 13 mm × 1.5 mm in thickness (n = 10 per group) (Figure 1).
Each block was sectioned using a precision cutting machine (Presi T210, France) operating at 3200 rpm with a feed rate of 0.2 mm/s. The specimens were polished using a polishing unit (Malek Teb, Iran) at 250 rpm with successive silicon carbide abrasive papers of 1200, 2000, and 3000 grit, each applied for 60 seconds. Surface debris was removed using an air syringe. Specimens were then ultrasonically cleaned in distilled water at 37 ± 1°C for 10 minutes (Euronda Eurosanic 4D, Italy) under 100% humidity. Dimensional accuracy was verified using a digital caliper (MAX150, Netherlands).
Surface microhardness was measured using a Vickers microhardness tester (Baresiss, Germany) equipped with a square-based pyramidal diamond indenter. An initial load of 10 g was found insufficient to produce clear indentations; therefore, a load of 20 g was applied for 10 seconds. Three indentations were made per specimen(figure 2), and the diagonal lengths of each square indentation were recorded. The Vickers hardness number (VHN) was calculated using the standard formula:
HV = 1.854 × F / d²
where F is the applied force (kg) and d² is the average of the squared diagonals of the indentation (mm²).
After baseline measurements, all specimens underwent thermocycling using a laboratory thermocycler (Vafaei TC300, Iran). The process involved 5,000 cycles between water baths at 5°C and 55°C, with a dwell time of 30 seconds in each bath and a transfer interval of 10 seconds. This protocol simulates approximately six months of clinical intraoral thermal exposure.
Post-thermocycling microhardness was reassessed using the same protocol. The collected data were analyzed using repeated measures analysis of variance (ANOVA) to evaluate changes in microhardness within and between material groups. The level of statistical significance was set at α = 0.05.
3. Results
A total of 30 specimens were prepared and evaluated, comprising three groups of CAD/CAM provisional restorative materials (n = 10 per group). The mean and standard deviation of surface microhardness values (Vickers hardness number, VHN) before and after thermocycling are presented in Table 1 Prior to thermocycling, Telio CAD exhibited significantly higher surface microhardness compared to Structur CAD and Vita CAD Temp (p < 0.05). No significant difference was observed between Structur CAD and Vita CAD Temp.
|
Timepoint |
Material |
n |
Mean |
SD |
SE |
95% CI (Lower) |
95% CI (Upper) |
Min - Max |
|
Before thermocycling |
Telio CAD (Ivoclar) |
10 |
38.55 |
5.9 |
1.87 |
34.33 |
42.77 |
29.60 - 50.20 |
|
Structur CAD (VOCO) |
10 |
31.92 |
4.39 |
1.39 |
28.78 |
35.06 |
25.40 - 37.40 |
|
|
Vita CAD (VITA) |
10 |
28.43 |
1.74 |
0.55 |
27.18 |
29.68 |
26.10 - 31.50 |
|
|
Total |
30 |
32.97 |
6 |
1.09 |
30.73 |
35.21 |
25.40 - 50.20 |
|
|
After thermocycling |
Telio CAD (Ivoclar) |
10 |
26.68 |
2.22 |
0.7 |
25.09 |
28.27 |
23.60 - 30.90 |
|
Structur CAD (VOCO) |
10 |
27.17 |
1.89 |
0.6 |
25.82 |
28.52 |
24.30 - 29.90 |
|
|
Vita CAD (VITA) |
10 |
28.31 |
2.21 |
0.7 |
26.73 |
29.89 |
25.00 - 31.00 |
|
|
Total |
30 |
27.39 |
2.15 |
0.39 |
26.58 |
28.19 |
23.60 - 31.00 |
SD: Standard Deviation; SE: Standard Error; CI: Confidence Interval; VHN: Vickers Hardness Number.
Table 1: Mean and standard deviation of surface Microhardness of the studied groups before and after Thermocycling.
After thermocycling, no statistically significant differences in microhardness were found among the three groups (p > 0.05) (Table 2, Figure 3). However, within-group analysis revealed a statistically significant decrease in surface microhardness in both the Telio CAD and Structur CAD groups (p < 0.05). In contrast, the change in surface microhardness in the Vita CAD Temp group was not statistically significant (Figure 3).
|
Timepoint |
Comparison |
Mean Diff. |
Std. Error |
p-value |
95% CI (Lower) |
95% CI (Upper) |
|
Before |
Telio vs Structur |
6.63* |
1.95 |
0.006 |
1.79 |
11.47 |
|
Before |
Telio vs Vita |
10.12* |
1.95 |
0 |
5.28 |
14.96 |
|
Before |
Structur vs Telio |
-6.63* |
1.95 |
0.006 |
-11.47 |
-1.79 |
|
Before |
Structur vs Vita |
3.49 |
1.95 |
0.192 |
-1.35 |
8.33 |
|
Before |
Vita vs Telio |
-10.12* |
1.95 |
0 |
-14.96 |
-5.28 |
|
Before |
Vita vs Structur |
-3.49 |
1.95 |
0.192 |
-8.33 |
1.35 |
|
After |
Telio vs Structur |
-0.49 |
0.94 |
0.863 |
-2.83 |
1.85 |
|
After |
Telio vs Vita |
-1.63 |
0.94 |
0.213 |
-3.97 |
0.71 |
|
After |
Structur vs Telio |
0.49 |
0.94 |
0.863 |
-1.85 |
2.83 |
|
After |
Structur vs Vita |
-1.14 |
0.94 |
0.459 |
-3.48 |
1.2 |
|
After |
Vita vs Telio |
1.63 |
0.94 |
0.213 |
-0.71 |
3.97 |
|
After |
Vita vs Structur |
1.14 |
0.94 |
0.459 |
-1.2 |
3.48 |
*Statistically significant differences are marked with an asterisk (*). CI: Confidence Interval
Table 2: Pairwise comparisons of surface microhardness (VHN) between groups before and after thermocycling.
Discussion
This study evaluated the effect of thermocycling on the surface microhardness of three CAD/CAM provisional restorative materials. Among the groups, Telio CAD exhibited the highest baseline microhardness, which was significantly greater than that of Vita CAD Temp and Structur CAD. However, after thermocycling, no significant differences were observed among the groups, suggesting a convergence of their mechanical performance under thermal stress. Notably, Telio CAD and Structur CAD demonstrated a statistically significant reduction in surface hardness, whereas Vita CAD Temp maintained its microhardness.
Provisional restorations are essential for maintaining biological, functional, and esthetic stability during the interim phase of treatment. Surface microhardness is a critical factor that influences wear resistance, surface smoothness, and plaque accumulation, all of which are important for long-term success—especially in patients with parafunctional habits or those requiring extended temporization periods [3,8,17–19].
The Vickers microhardness test is a commonly used, non-destructive method for evaluating surface hardness in dental materials. Despite its simplicity and reproducibility, it is sensitive to variables such as indenter load and dwell time, which can affect measurement accuracy [3,10,13–15]. In the present study, a 10 g load was initially used, but insufficient indentation clarity led to the adoption of a 20 g load, consistent with findings from previous studies [3,8].
Our results are in agreement with those of Basak et al. and Atai et al., who reported significant decreases in the microhardness of CAD/CAM temporaries following thermocycling [3,24]. Similar findings were observed by Diaz-Arnold et al., who reported hardness reduction after immersion in artificial saliva [25]. In contrast, Oliveira et al. and Swabi et al. found no significant changes in surface microhardness following thermal or aqueous aging [8,26]. These conflicting findings may stem from differences in material composition, testing parameters, or sample preparation methods.
The mechanical behavior of provisional materials is highly influenced by their chemical structure. PMMA-based materials, such as Telio CAD, typically exhibit low filler content and high water absorption, leading to decreased mechanical stability over time. This may explain the significant reduction in microhardness observed in this group post-thermocycling [24]. On the other hand, materials like Vita CAD Temp, which are composed of highly cross-linked dimethacrylate (DMA) resins with microfillers, are known for their superior dimensional stability and resistance to hydrolytic degradation [17,19].
These differences underscore the importance of filler content and resin matrix composition in determining the long-term performance of provisional materials. Previous studies have also suggested that higher filler loading is positively correlated with greater surface hardness [17].
While thermocycling provides valuable insight into the thermal aging of materials, it does not replicate all oral conditions. Clinical aging is influenced by mechanical loading, pH fluctuations, salivary enzymes, and dietary acids. Therefore, future studies should incorporate these additional factors to better predict the intraoral performance of provisional restorations.
Conclusion
Within the limitations of this in vitro study, it was found that the initial surface microhardness of the evaluated CAD/CAM provisional restorative materials differed significantly. However, after 5,000 thermal cycles simulating six months of intraoral thermal stress, no statistically significant differences remained among the materials. These results suggest that, despite initial variability, all tested materials demonstrated comparable performance following thermal aging.
The main limitation of this study is its in vitro design, which does not fully replicate the complex oral environment, including mechanical forces, salivary enzymes, and pH variations. Additionally, the selection of materials was restricted due to local availability and import regulations. Further clinical studies are warranted to validate these findings under real-world conditions.
References
- Regish KM, Sharma D, Prithviraj DR. Techniques of fabrication of provisional restoration: an overview. Int J Dent 9 (2011):134659.
- Tom TN, Uthappa MA, Sunny K, et al. Provisional restorations: an overview of materials used. J Adv Clin Res Insights 3 (2016): 212-214.
- Basak SS, Özmen MF, Sagsöz Ö, et al. Effect of thermo-cycling on microhardness of CAD-CAM provisional materials. Int J Appl Dent Sci 6 (2020): 254-257.
- Reeponmaha T, Angwaravong O, Angwarawong T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J Adv Prosthodont 12 (2020): 218-225.
- Rayyan MM, Aboushelib M, Sayed NM, et al. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J Prosthet Dent 114 (2015): 414-419.
- Medeiros IS, Gomes MN, Loguercio AD, et al. Diametral tensile strength and Vickers hardness of a composite after storage in different solutions. J Oral Sci 49 (2007): 61-66.
- Digholkar S, Madhav VN, Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J Indian Prosthodont Soc 16 (2016): 328-334.
- Oliveira JC, Aiello G, Mendes B, et al. Effect of storage in water and thermocycling on hardness and roughness of resin materials for temporary restorations. Mater Res 13 (2010): 355-359.
- Porto TS, Park SJ, Faddoul AJ, et al. Evaluation of the surface roughness and accelerated aging of CAD/CAM materials. Int J Prosthodont 33 (2020): 418-28.
- Quek SH, Yap AU, Rosa V, et al. Effect of staining beverages on color and translucency of CAD/CAM composites. J Esthet Restor Dent 30 (2018): E9-17.
- Kanca J. Visible light-activated posterior composite resins- A comparison of surface hardness and uniformity of cure. Quintessence Int 16 (1985): 345-347.
- Sakaguchi RL, Powers JM. Craig’s restorative dental materials (13th edtn), St. Louis: Elsevier Health Sciences (2012).
- Jani K, Bagda K, Jani M, et al. Effect of storage in water on solubility and effect of thermocycling on microhardness of four different temporary restorative materials. Natl J Integr Res Med 6 (2015): 75-78.
- Goyal RK, Tiwari AN, Negi YS. Microhardness of PEEK/ceramic micro- and nanocomposites: correlation with Halpin–Tsai model. Mater Sci Eng A 491 (2008): 230-236.
- Lee SY, Lai YL, Hsu TS, et al. Evaluation of hardness and microhardness of polymethyl methacrylate resin. Eur J Oral Sci 123 (2015): 179-183.
- Abdullah AO, Pollington S, Liu Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent Mater J 37 (2018): 957-963.
- Liebermann A, Wimmer T, Schmidlin PR, et al. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J Prosthet Dent 115 (2016): 321-328.
- Negahdari K, Tavanagar MS, Bagheri R. Sorption, solubility, and surface microhardness of 3 nanohybrid resin composites after 60 days of water storage. J Dent Med 30 (2018): 200-207.
- Hensel F, Koenig A, Doerfler HM, et al. CAD/CAM resin-based composites for use in long-term temporary fixed dental prostheses. Polymers (Basel) 13 (2021): 34-69.
- Kim JW, Jang KT, Lee SH, et al. Effect of curing method and curing time on the microhardness and wear of pit and fissure sealants. Dent Mater 18 (2002): 120-127.
- Dayan C, Kiseri B, Gencel B, et al. Wear resistance and microhardness of various interim fixed prosthesis materials. J Oral Sci 61 (2019): 447-453.
- Chuenarrom C, Benjakul P, Daosodsai P. Effect of indentation load and time on Knoop and Vickers microhardness tests for enamel and dentin. Mater Res 12 (2009): 473-476.
- Bauer R, Zacher J, Strasser T, et al. In vitro performance and fracture resistance of interim conventional or CAD-CAM implant-supported screw- or cement-retained anterior fixed partial dentures. J Prosthet Dent 126 (2021): 575-580.
- Atay A, Sagirkaya E. Effects of different storage conditions on mechanical properties of CAD/CAM restorative materials. Odovtos Int J Dent Sci 22 (2020): 83-96.
- Diaz-Arnold AM, Dunne JT, Jones AH. Microhardness of provisional fixed prosthodontic materials. J Prosthet Dent 82 (1999): 525-528.
- Savabi O, Nejatidanesh F, Fathi MH, et al. Evaluation of hardness and wear resistance of interim restorative materials. Dent Res J (Isfahan) 10 (2013): 184-189.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 76.66%
Acceptance Rate: 76.66%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 